Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Anomalies of the fetal spine, particularly spina bifida, are amongst the commonest fetal malformations detectable. Anencephaly and spina bifida are the commonest neural tube defects (NTDs), accounting for up to 95% of all NTDs, and they occur with a nearly equal frequency of 1 in 1000 births though there is some variation depending on geographic location and sex of the fetus. Historically the UK and Ireland have had the highest prevalence of neural tube defects. Before the use of folic acid supplementation, Ireland had the highest incidence in the world at 1% of all births. There has been a marked decline over the last 30 years and at present the incidence is believed to be 0.8/1000 total births in England. Prevalence rates are becoming harder to compare because of the increasing impact of antenatal diagnosis and termination of pregnancy. The diagnosis of spinal abnormalities is closely linked with observation of anomalies in the head so that there is overlap between this chapter and Chapter 11 , Cranial Abnormalities. However, there are a number of more subtle malformations such as occult spinal dysraphisms, diastematomyelia, lipomeningocoeles and scoliosis that require detailed observation of the spinal anatomy itself if the diagnosis is to be made prenatally. These anomalies have a potentially huge impact on neurological and orthopaedic services as well as family life. It is to this end that considerable resources have been devoted to their prenatal detection, both through biochemical tests and ultrasound.
The human embryo passes through 23 stages of development after conception, each stage lasting approximately 2–3 days ( Table 12-1 ).
| Days of Gestation | Disruption at this Stage: Resulting Fetal Malformation |
|---|---|
| 0–18 | Death or unclear effect |
| 18 | Anterior midline defects |
| 22–23 | Hydrocephalus (18–60 d) |
| 24–26 | Anencephaly |
| 26–28 | Cranium bifidum, spina bifida cystica, spina bifida occulta |
| 32 | Microcephaly (30–130 d), migration anomalies |
| 33–35 | Holoprosencephaly |
| 70–100 | Agenesis of the corpus callosum |
Two different processes form the CNS:
The first stage in which the neural structures are formed into a tube is called primary neurulation, and this results in the formation of the brain and the spinal cord.
In the next stage, called secondary neurulation, there is formation of the lower spinal cord, which gives rise to the lumbar and sacral elements.
The neural plate is formed at stage 8, the neural fold occurs at stage 9 and then fusion of the neural folds occurs at stage 10.
The current role and future potential of prenatal ultrasound in the diagnosis of cranial and spinal dysraphisms is discussed below.
The normal examination of the fetal brain is covered very systematically in Chapter 11 and the reader is advised to review this anatomy before embarking on this chapter.
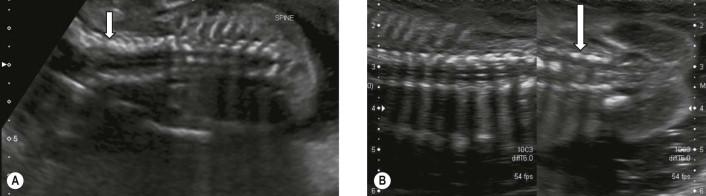
On two-dimensional ultrasound, the views of interest for initial screening and diagnosis of spina bifida and other neural tube defects are the transventricular and the transcerebellar views ( Figure 12-1 A, B ).
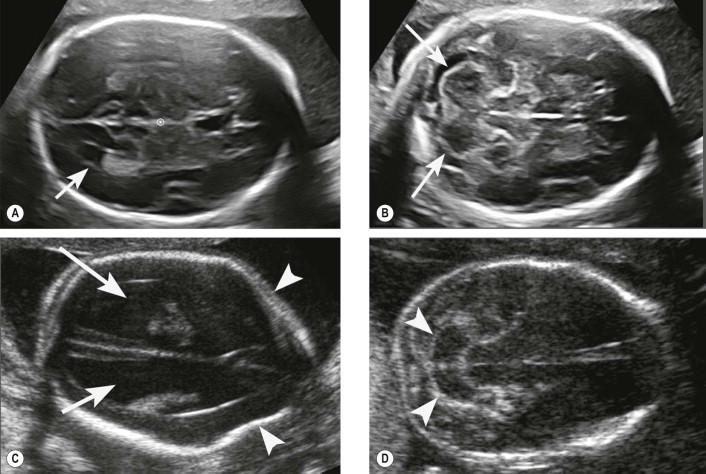
On the transventricular view, the secondary ventriculomegaly often associated with spina bifida and the frontal bone scalloping (‘lemon sign’) ( Figure 12-1C ) are diagnosed with the Arnold–Chiari II malformation (‘banana sign’) recognized on the transcerebellar view ( Figure 12-1D ). The degree of descent of the cerebellum may be significant, and due to shadowing from the occipital bones, the cerebellar abnormality may only be seen with a transvaginal (TV) scan ( Figure 12-2 ).

It is only with three-dimensional ultrasound that the prenatal assessment of cranial bones, in the normal and abnormal fetus, has become reproducible and adequate ( Figure 12-3 ). This imaging modality allows:
detailed evaluation of the fetal brain;
neat characterization of cranial bones, sutures and fontanelles.
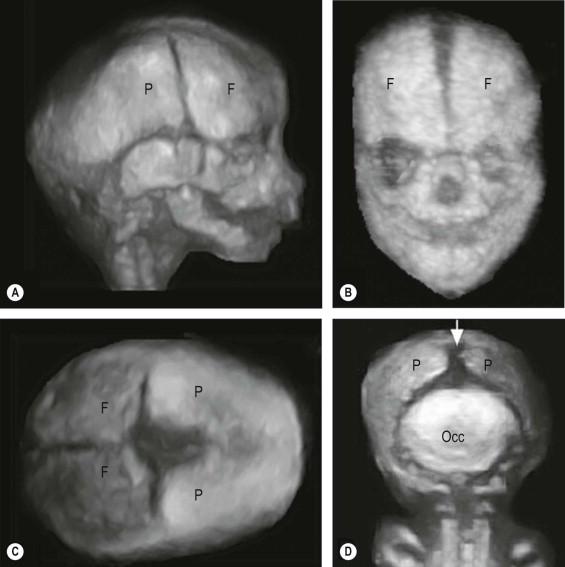
In this way, both delayed ossification or premature closure of the fontanelles and/or sealing of the sutures (synostosis) has become readily recognizable in utero. This modality can therefore be advantageously employed to also characterize the bony component in encephalocoeles.
The sonographic assessment of the fetal spine depends on the visualization of the ossification centres of the fetal vertebral bodies in the coronal, sagittal and transverse planes.
Each vertebral body has three ossification centres: one in the body and one at the base of each transverse process ( Figure 12-4 ).

Ossification of the vertebral body (also known as the centrum) begins at the thorocolumbar junction and progresses in cephalic and caudad directions.
There may be at least three initial centres of ossification for the neural arch with ossification progressing cranially and caudally from each. Within the lumbar region ossification progresses in a caudad direction, possibly more quickly in females.
Within the neural arches of the lumbosacral region ossification progresses caudally at a rate of one vertebral level every 2 to 3 weeks after 16 weeks ( Figure 12-5 A and B ; Table 12-2 ).

| Vertebral Body Level | Gestational Age at which the Degree of Ossification is Similar to the Iliac Wings |
|---|---|
| L5 | 16 weeks |
| S1 | 19 weeks |
| S2 | 22 weeks |
| S3 | 24 weeks |
| S4 | 25 weeks |
| S5 | 27 weeks |
The importance of recognizing this normal evolution is that too early a scan may not be able to exclude a neural tube abnormality in fetuses at high risk for a neural tube defect. The technique for examination must take into account fetal gestational age as discussed and fetal position.
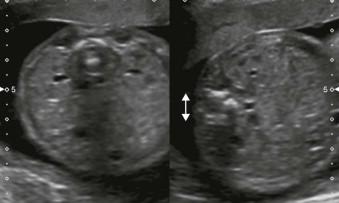
The three ossification centres will appear as three dots of bone. The two posterior elements should converge towards each other to form an arch. However the normal arching of the posterior ossification centres is far better appreciated in the prone fetus with its back to the transducer ( Figure 12-6 ). This view also allows for assessment of the integrity of the overlying skin.

The fetus lying decubitus will appear to have posterior elements that are in parallel to each other ( Figure 12-7 ).
Splaying of the posterior elements in the lumbosacral region will be produced by angling too obliquely when attempting to image axially ( Figure 12-8 ). This effect may be exaggerated by side lobe artefact producing an apparent meningocoele.
In this view the three ossification centres give a three line appearance. The inter-pedicular distance is essentially constant throughout the spine ( Figure 12-9 ). This view also allows the level of a defect to be determined as the 12th rib will be seen.

There is a normal physiological widening in the upper spine before the cranio-occipital junction and at the lumbosacral spine just prior to the normal tapering towards the sacrum ( Figure 12-10 A and B ).
This view demonstrates two bony structures: the ossification centre of the vertebral body and also the junction of the posterior ossification centres. The all-important integrity of the overlying skin covering will be visualized.
This view will also demonstrate the normal hypo-echoic spinal cord tapering to the level of the upper sacrum and its continuity with the echogenic cauda equina ( Figure 12-11 ).
A true sagittal view of the lower sacrum may only demonstrate the ossification centre of the body due to an insufficiently ossified neural arch.
Splaying in the thoracic region will be mimicked by imaging the ribs and not the ossification centre of the transverse process.
The sacrum may show incomplete ossification prior to 25 weeks' gestational age ( Figure 12-12 ).

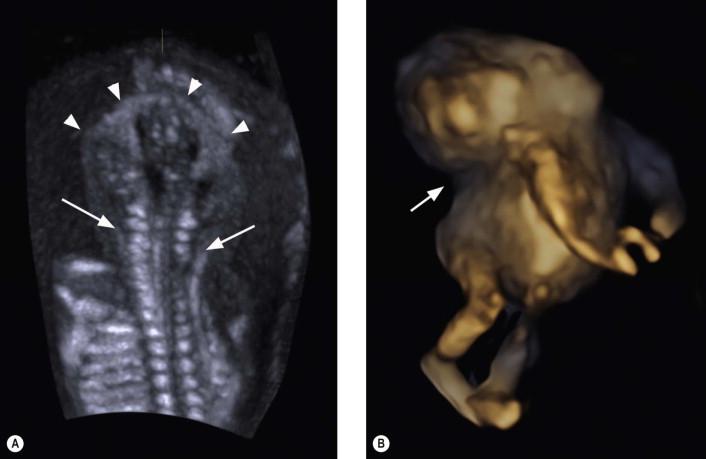
Three-dimensional imaging is able to provide the sonologist with even more self-explanatory images of the fetal spine and rib-cage. In most cases a transabdominal approach suffices, but in obese women and in those in which a breech fetal lie is obscuring a more direct approach to the spine, transvaginal scanning is able to provide dramatic images of spinal anatomy, especially if three-dimensional ultrasound is used.
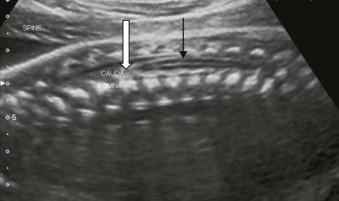
The main difference between two and three-dimensional ultrasound is that with three-dimensional ultrasound a volume dataset of the whole spine is acquired. After acquisition, the operator can choose to navigate through this volume, applying in post-processing a series of rendering modalities to highlight the skin contour, the bony skeleton and to render the coronal plane. This, in turn, determines a higher degree of accuracy in reaching the final diagnosis and in its characterization both from a diagnostic and a prognostic standpoint ( Figure 12-13 ).
Iniencephaly is included here as it has features of both a cranial and a spinal lesion.
This is a rare abnormality with a prevalence of 0.1–10:10,000 births. It has a pronounced female predilection F9: M1.
This is a rare dysraphic malformation which has three major primary defects: a deficient occiput and inion combined with rachischisis of the cervical and thoracic spine with retroflexion of the head.
The exact aetiology is unknown, but seasonal and yearly variations exist. Other contributing factors include low parity and low socioeconomic status.
The diagnostic criteria for iniencephaly are:
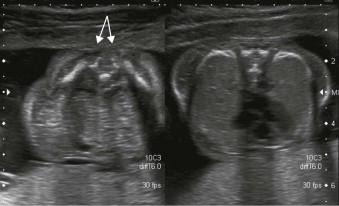
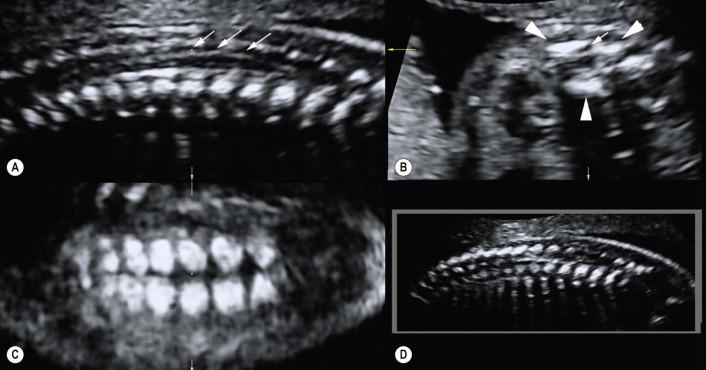
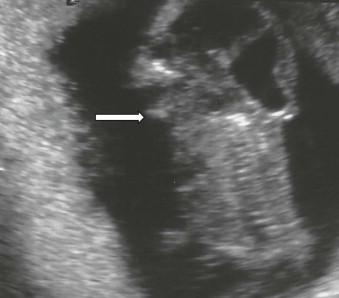
A variably sized deficit of the occipital bones resulting in an enlarged foramen magnum ( Figure 12-14 ).

Partial or total absence of several cervical and thoracic vertebrae with incomplete closure of the vertebral arches and/or bodies. Any vertebrae that are visible are often abnormally fused to each other.
Significant shortening of the spinal column due to marked lordosis and hyperextension of the malformed cervical–thoracic spine.
The profound fixed hyperextension and lack of a neck will result in an upward-turned face and mandibular skin directly in continuity with the skin of the chest ( Figures 12-15 and 12-16 ) and the fetal occiput will be adjacent to the thoracic spine ( Figure 12-16 ).
There are almost always (84% of cases) additional abnormalities in this invariably fatal defect.
Spinal cord malformations are collectively referred to as spinal dysraphisms. They are generated from defects occurring in the early embryologic stages of gastrulation (weeks 2–3), primary neurulation (weeks 3–4), and secondary neurulation (weeks 5–6).
Incidence: 1 in 1000 at birth. There is a higher prevalence in Whites and in Hispanics than in African-Americans and Asians. The birth prevalence of spina bifida is slowly decreasing due to the increased prenatal detection rate.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here