Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Fecal incontinence (FI) is the inability to maintain voluntary control of the passage of gas, liquid, or solid stool through the anus. Although FI is not a life-threatening condition, it is certainly a life-altering condition. The associated embarrassment, subsequent coping mechanisms, and behavioral changes can lead to a dramatic decrease in quality of life (QoL) and social isolation. The prevalence of FI is difficult to determine because of potential misdiagnosis, underdiagnosis, or variations in definition and the population under study. Community prevalence has been estimated to range from 0.5% to 11%. A Wisconsin telephone survey reported that 2.2% of the general population experienced FI of varying degrees. The prevalence increases to 13.4% in outpatients seeing their primary care physicians and 26% in outpatients seeing their gastroenterologist. The highest rates of incontinence are seen in institutionalized individuals; a survey of 18,000 Wisconsin nursing home residents found that 47% had FI. Overall, the prevalence is much higher in women, the elderly, and nursing home residents.
The underlying cause of FI can be from a variety of mechanisms and can be divided into three main categories: anatomic, neurologic, or mechanical. Examples of anatomic causes of FI include obstetric injury to the sphincter or iatrogenic injury from sphincterotomy. Neurologic causes include nerve injury, diabetes, and spinal cord injury. Mechanical etiologies of FI may be related to a normal mechanism being overwhelmed by high-output liquid stool (e.g., secretory tumors or diarrhea) or prolapsing tissue through the anal canal leading to constant seepage. Oftentimes, the underlying cause of FI may be related to a combination of factors ( Box 148.1 ).
Diarrheal states
Infectious diarrhea
Inflammatory bowel disease
Short gut syndrome
Laxative abuse
Radiation enteritis
Overflow
Impaction
Encopresis
Rectal neoplasms
Neurologic conditions
Congenital anomalies (e.g., myelomeningocele)
Multiple sclerosis
Dementia, strokes, tabes dorsalis
Neuropathy (e.g., diabetes)
Neoplasms of brain, spinal cord, cauda equina
Congenital anorectal malformation
Trauma
Accidental injury (e.g., impalement, pelvic fracture)
Anorectal surgery
Obstetric injury
Aging
Vaginal delivery
Chronic straining at stool
Rectal prolapse
Descending perineum syndrome
Initial evaluation should consist of a detailed history and physical examination. This is usually sufficient to diagnose FI, and occasionally special testing is needed to identify the underlying cause. This can include imaging, laboratory tests, stool testing, colonoscopy, or anal physiology testing.
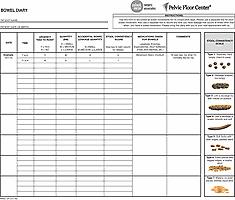
History taking is a vital step in the diagnosis of FI. Embarrassment and shame from these symptoms can make the history difficult to obtain. Oftentimes, it may be beneficial to conduct the history face-to-face and sitting down with the patient. Patients may downplay frequency or severity of symptoms or even be reluctant to admit that they have problems with bowel control. For example, patients may present with complaints of “diarrhea” when they actually are experiencing involuntary passage of liquid stool. Questions should be focused on understanding when and if the patient gets an urge or warning before passing gas or stool and how frequently this occurs. It is important to ask about stool consistency and if there is a change in bowel habits. The Bristol Stool Scale can be helpful in objectively understanding stool consistency. Asking the patient to keep a diary to record stool frequency, urgency, and consistency allows for a better understanding of FI severity ( Fig. 148.1 ). During the history taking, the past medical history should be focused on specific risk factors for FI, such as previous anorectal procedures ; vaginal deliveries, particularly with episiotomies, tears or difficult extractions; pelvic radiation ; diabetes mellitus; chronic diarrhea; congenital conditions, such as imperforate anus and spina bifida; urinary incontinence; or complaints of rectal prolapse or anal protrusion.
Validated scoring systems and questionnaires are helpful to objectively measure frequency and severity of FI. Various scoring systems or severity indices exist and are widely used, although no one scoring system is universally accepted. An ideal instrument will measure the frequency of accidents and nature of the leakage (gas, liquid, solid) at minimum. Use of devices (i.e., pad or tissue paper), coping methods, or urgency are also included in some measurement tools. Commonly used scoring systems include Fecal Incontinence Severity Index (FISI) and Wexner. The FISI is increasingly being used because its scores were derived from both patient- and colorectal surgeon-based weighting of severity.
Measurement of QoL is an important tool for understanding how a disease process impacts an individual's health. In patients with FI, the impact of the disease on QoL is used to guide clinical decision-making and determine efficacy of treatment. Use of QoL instruments in managing patients with FI is especially important because FI is fundamentally a QoL issue. General QoL scales may be used, as well as more specific QoL scales, in the FI population. Specific FI scales often include questions on overall health and well-being, behavioral modifications related to FI episodes or fear of loss of control, use of devices, ability to perform usual daily activities, social activities, and urgency. However, studies have shown that the scales may not always be applicable for certain patient populations or have undergone standardized rigorous psychometric testing to be deemed “reliable.” In addition, these QoL instruments may be cumbersome for the patient to fill out and for the physician to interpret. Various scales have attempted to create a single summary score, but these may not accurately capture the disease severity and impact on a patient's QoL. There is no one preferred scale for measuring FI and various testing and reformulation of existing scales is ongoing. One validated scale that is frequently used in the literature is the FI-specific QoL (FIQL) score, although studies have shown it is not the most sensitive to change and it does not include a specific urgency component.
After a thorough history, physical examination is the next step in diagnosis of FI. Exam begins with external inspection of the perianal area. Signs of moisture or bowel leakage can be evident upon examination of the area. Use of a pad or diaper can also be noticed. Excess moisture from leakage or soilage can lead to irritation and excoriation of perianal skin. Presence of external skin tags or hemorrhoids may also be a clue to factors that may be contributing to FI or leakage. The examiner should also look for any scars from trauma or previous surgery. If the patient has had previous anorectal surgery for an anal fissure or fistula, special attention should be paid to evaluate for presence of a “keyhole deformity” in the anal canal, particularly in the posterior midline. This defect can lead to seepage of stool or mucus from a previous sphincterotomy, fissurectomy, or fistulotomy. Female patients with previous obstetric injury may have a thin perineal body, rectovaginal fistula, or cloaca visible on exam. Visualization of the anus may reveal an asymmetric appearance from potential sphincter defects or previous trauma. This appearance may be exaggerated when eliciting the anocutaneous reflex. This spinal reflex results in contraction of the anal sphincter, commonly referred to as “anal wink,” when the perianal skin is stroked and is mediated by afferent and efferent pathways in the pudendal nerve. It will be absent in patients where S4 has been transected.
A patulous anus can be seen in patients with rectal prolapse and may be more evident with traction of the buttocks. Additional physical exam findings may be evident if the patient is asked to bear down. A full-thickness rectal prolapse, mucosal prolapse, or hemorrhoidal prolapse may be visible. This can be done with the patient in the left lateral or prone position. However, the best position to assess presence and severity of prolapse is with the patient bearing down while seated on a commode.
Digital exam is useful for assessing resting sphincter tone, strength of squeeze, abnormal masses, and appropriateness of relaxation of the pelvic floor musculature with Valsalva. Presence of hard stool in the rectal vault can be suggestive of fecal impaction, leading to overflow incontinence. The examiner should palpate for defects or holes in the anterior rectum consistent with rectovaginal fistula, particularly in patients with history of obstetric trauma. Female patients who have had an obstetric injury may have a small perineal body due to retraction of the sphincter muscle posterolaterally. Redundancy or a bulge anteriorly may be detected in patients with rectocele or weakening of the rectovaginal septum. A large rectocele may cause the posterior wall of the vagina to be pushed out of the introitus.
The patient should be asked to squeeze on the examiner's finger during digital rectal exam, as if trying to hold in a bowel movement, then relax, and then push, as if having a bowel movement. Patients with diminished tone or weak pelvic floor muscles may try to compensate with strong contraction of the gluteal muscles. The external sphincter should fatigue to basal level after maximal contraction within 3 minutes. Patients with a weakened sphincter may have a more rapid fatigue. On digital exam, the puborectalis muscle can be examined by hooking one's finger posteriorly. With contraction of the puborectalis, the examiner's finger should be lifted or should feel tightening at the top of the anal canal. Conversely, when asked to push, the puborectalis should relax allowing the anorectal angle to widen.
Anoscopy should be included in the physical examination of a patient with FI. Prolapsing polyps or hemorrhoids, scarring in the anal canal from previous surgery or trauma, internal fistula openings, keyhole deformities, or mucosal inflammation may be seen during anoscopy. Further examination with a flexible sigmoidoscopy can also reveal evidence of proctitis, malignancy, or other neoplasm. Full colonoscopy may be indicated if the patient has symptoms of diarrhea.
The appropriate medical and/or surgical treatment can be determined for the majority of patients with FI with just a thorough history and physical exam. Additional anorectal physiology testing may be helpful in patients with unusual symptoms or an unclear diagnosis or those who have failed initial medical or surgical treatment. This testing can document the degree of anorectal dysfunction, clarify anatomy, and identify certain pathology. The most frequently used tests include anal manometry, rectal distention testing, electromyography (EMG), ultrasound, and defecography.
Anal manometry measures pressure zones in the anal canal and distal rectum, providing an assessment of internal and external anal sphincter strength and function. There are multiple techniques of manometry, some using microtransducers, water-perfused catheters, or solid-state catheters. The pressure or resistance of flow of fluid from the catheters is measured either in a continuous pull-through method or at various predetermined spots within the anal canal (“stationary” technique). Measurements obtained from anorectal manometry include resting pressure, squeeze pressure, length of the high-pressure zone, rectal sensation, and the rectoanal inhibitory reflex. Resting pressure is a good reflection of internal anal sphincter tone because it is responsible for 55% to 85% of the resting pressure. The external anal sphincter contributes less to resting pressure. Typical resting pressure in a healthy volunteer is 40 to 60 mmHg. A patient with low resting pressure may have an underlying problem with the internal anal sphincter.
Squeeze pressure can be measured by asking the patient to maximally squeeze, as if holding in a bowel movement. This is under voluntary control and reflects the external anal sphincter function. If a patient is unable to comply with directions, this pressure reading may be inaccurate. The resting and squeeze pressures are typically higher in males compared with females, and pressures decrease with age. The length of the high-pressure zone is measured during anorectal manometry and is defined as the area where pressures are greater than half of the maximal resting pressure. This zone is typically shorter in women (2 to 3 cm) compared with men (2.5 to 3.5 cm).
To measure rectal sensation, a balloon is inserted in the rectum and slowly inflated with air to distend the rectum. The volume at which the patient first feels the balloon, feels the urge to defecate, and feels a maximum tolerable volume are measured. Patients with lower than expected values during rectal distention testing have hyperacute sensation. This can be seen in patients with urge FI or those with poor rectal compliance. Poor compliance can be secondary to chronic inflammation, radiation changes, or postoperative changes. In such conditions the rectum cannot distend appropriately, thus leading to problems with FI, as the reservoir function of the rectum has been lost. Conversely, patients with higher than expected volumes during rectal distention measurements are felt to have blunted sensation in the rectum. This can result in overfilling and stretching of the rectum and subsequent overflow incontinence. This can be seen in patients with chronic constipation or neurogenic problems.
The rectoanal inhibitory reflex, also known as the “sampling” reflex, is a contraction of the external sphincter with subsequent internal anal sphincter relaxation in response to rectal distention. This relaxation of the internal anal sphincter allows exposure of the anal canal sensory mucosa to the distal rectal contents. Through this “sampling” of the rectal contents, the patient is then able to distinguish if the cause of the distention is gas, liquid, or solid stool and react accordingly. It is a normal reflex and is notably absent in patients with Hirschsprung disease, Chagas disease, dermatomyositis, and scleroderma. It may also be absent in patients immediately after rectal resection with coloanal anastomosis or reduced in patients with megarectum or very low resting pressures.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here