Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Optic neuritis is an inflammatory or demyelinating process involving the optic nerve. The presentation of optic neuritis is characterized by painful, acute/subacute vision loss with corroborating evidence of an optic neuropathy on examination that may include a relative afferent pupillary defect, visual field dysfunction, dyschromatopsia, and optic nerve edema. Optic neuritis may occur as a clinically isolated syndrome or in association with neurologic/systemic disease. This section examines pediatric optic neuritis in the context of demyelinating and inflammatory disease processes in children. When possible, a careful understanding of the underlying etiology of optic neuritis is critical in order to target the appropriate treatment to protect the child from irreversible vision loss and to address neurologic or systemic disease. Therefore a multidisciplinary approach involving both ophthalmology and neurology is essential to assess visual function and to manage systemic therapy when relevant.
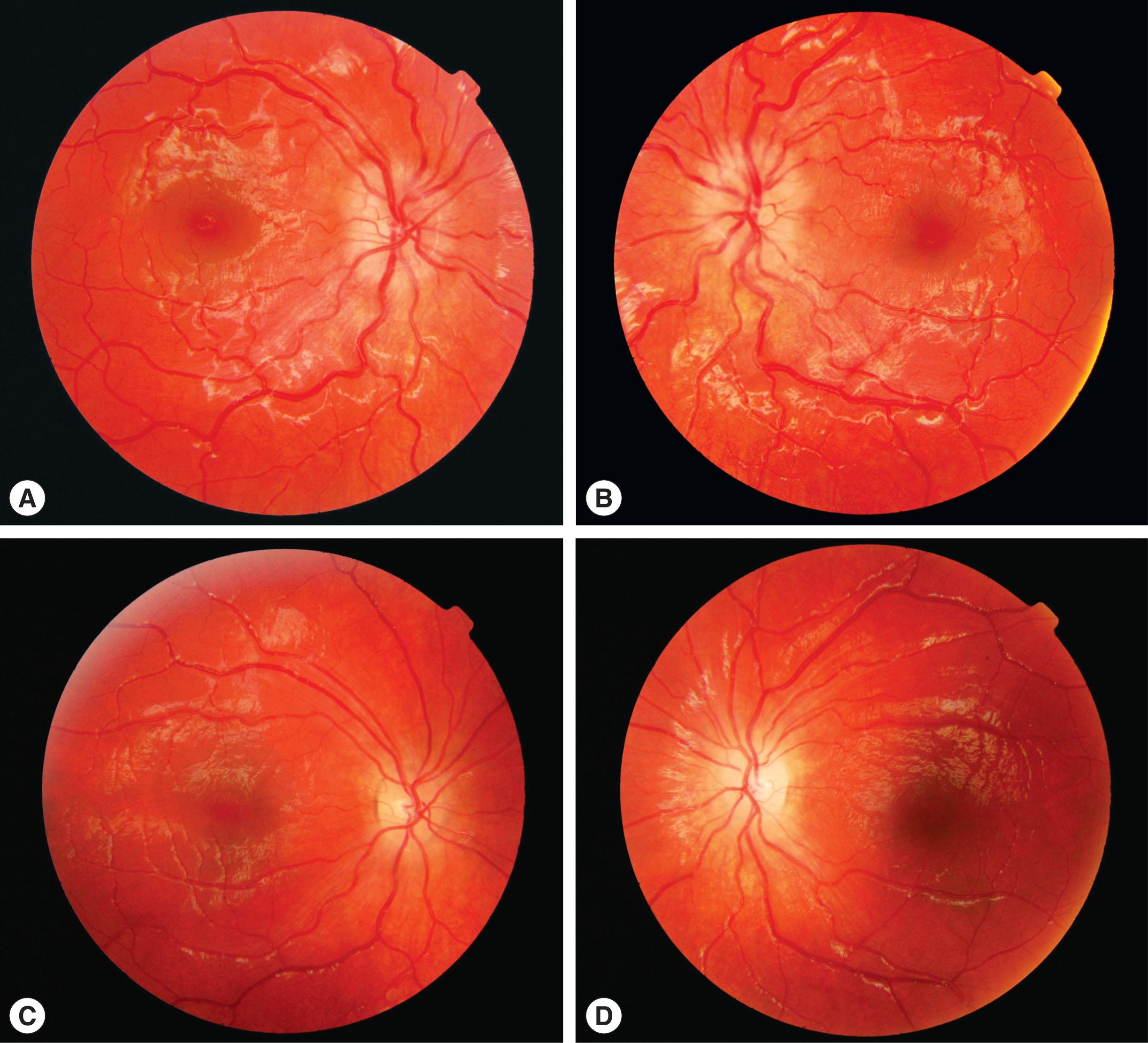
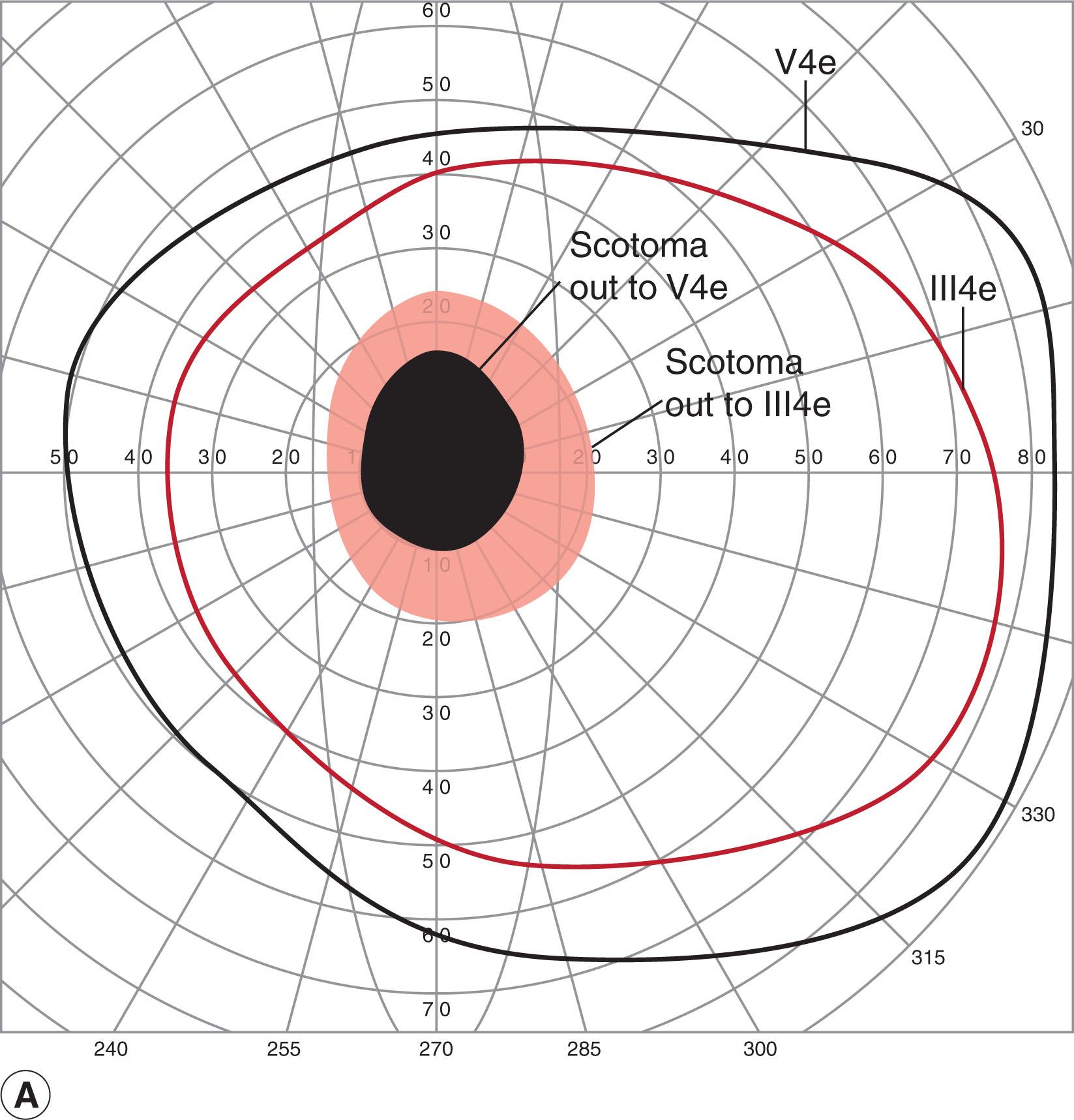
The prevalence of pediatric optic neuritis is unknown. In one retrospective study of all patients presenting with optic neuritis in Olmstead County, Minnesota, pediatric optic neuritis accounted for fewer than 5% of cases, with a higher prevalence in adolescents compared with children. The clinical presentation differs from adult optic neuritis insofar as bilateral optic nerve involvement is more frequent, and occurs in nearly 50% of childhood optic neuritis. The anterior part of the optic nerve is commonly involved, resulting in papillitis ( Fig. 56.1 ). In a meta-analysis of 223 published cases, bilateral optic nerve involvement was associated with younger age at presentation, with 72% of children <10 years experiencing bilateral disease and 70% of children ≥10 years with unilateral involvement. Also in contrast with adult disease, pain with eye movements is not a universal presenting symptom in pediatric optic neuritis. Several retrospective studies have reported on varied levels of initial vision loss from minimal to severe with excellent visual recovery of high contrast acuity, although these reports also highlight that good recovery is not universal. In one retrospective study of a large pediatric cohort with first episode optic neuritis, the primary risk factor for a poor high contrast acuity at 1 year of <20/40 was lack of recovery to 20/20 vision at 3 months after the initial presentation. Low contrast acuity has been demonstrated to be a more sensitive metric to assess persistent visual disability in optic neuritis in spite of good recovery of high contrast visual function. Vision loss may be accompanied by visual field defects including but not limited to central or paracentral scotomas ( Fig. 56.2 ). Results from the first, prospective natural history study on pediatric optic neuritis (PON1) were recently published with the primary outcome measure of high and low contrast visual acuity at 6 months. This study represented a significant collaborative effort among the enrolling clinicians from the Pediatric Eye Disease Investigator Group (PEDIG) and the Neuro-Ophthalmology Research Disease Investigator Consortium (NORDIC). Children between ages 3 and 15 years who presented within 2 weeks of onset of optic neuritis in a previously unaffected eye were enrolled. For high contrast visual acuity, the mean vision at presentation was 20/200 which improved to a mean of 20/25 at 6 months. For low contrast visual acuity, mean vision at presentation was 20/640 which improved to 20/100 at 6 months. Visual recovery therefore was favorable, and future prospective work will be aimed at a determination of visual outcomes at 2 years. In addition, the study may be able to provide evidence regarding the risk of poor visual recovery, the relationship of neuroimaging and onset of neurologic disease, and relationship between pubertal status and visual outcomes. Further, this study will be formative towards the possibility of the first prospective pediatric optic neuritis treatment trial.
Using optical coherence tomography (OCT), damage to both the retinal nerve fiber layer (rNFL) as well as the ganglion cell layer (GCL) is detected after an episode of optic neuritis and these changes appear to correlate well with visual function as measured by low contrast acuity. Data on OCT findings at presentation were included in PON1. This study among others may inform how anatomic changes on OCT may potentially be considered as a useful metric in clinical studies of treatment efficacy of optic neuritis and demyelinating disease.
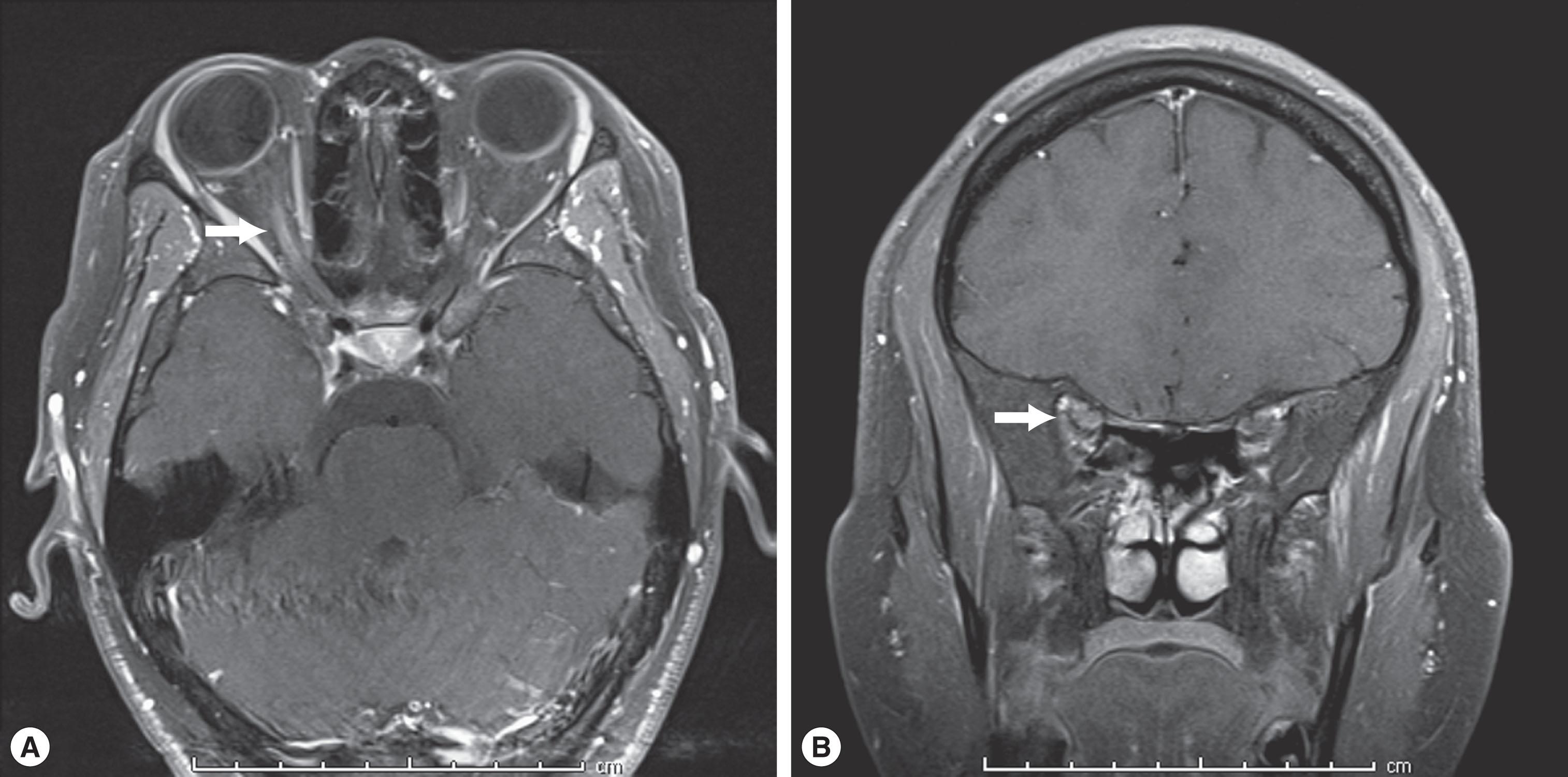
The diagnosis may be made from the clinical symptoms and signs coupled with findings on magnetic resonance imaging (MRI) of contrast enhancement of the optic nerve on T1-weighted MRI images or hyperintensity of the optic nerve on T2-weighted MRI images ( Fig. 56.3 ).
Treatment of pediatric optic neuritis is institution-dependent but typically involves intravenous (IV) methylprednisolone followed by an oral prednisone taper. This strategy has been informed by the corticosteroid regimen used in the landmark adult Optic Neuritis Treatment Trial in which IV methylprednisolone followed by an oral prednisone taper was shown to hasten visual recovery. This consideration is particularly relevant in children when bilateral disease is present. To date, prospective data on the efficacy of corticosteroid treatment in pediatric optic neuritis are lacking and are greatly needed. In patients with refractory vision loss, a multimodal approach including plasma exchange (PLEX) or administration of intravenous immunoglobulin (IVIG) is often used.
The management of a child with optic neuritis should involve both ophthalmology and neurology. Although pediatric optic neuritis occurs as a clinically isolated syndrome, optic neuritis often occurs in the context of demyelinating disease and indeed may be the initial presenting sign of a demyelinating condition. The underlying disease phenotypes for demyelinating optic neuritis have expanded during this decade. In addition to consideration of pediatric optic neuritis associated with multiple sclerosis (MS), acute disseminated encephalomyelitis (ADEM), and neuromyelitis optica or Devic’s disease (NMO), recent advances in testing have identified optic neuritis associated with myelin oligodendrocyte glycoprotein (MOG-IgG+) as a distinct clinical phenotype of demyelinating disease.
In general, the reported incidence of an acquired demyelinating condition of the CNS (including transverse myelitis) in children is 0.9 per 100,000 person-years in Canada and 1.66 per 100,000 person-years in a multi-ethnic California-based cohort. There is a higher proportion of optic neuritis in adolescents compared with younger children and an equal incidence in boys and girls compared with 2:1 female predominance in post pubertal children. Each condition is associated with a unique prognosis and treatment plan and therefore a careful evaluation for these conditions is essential in a child with optic neuritis.
The incidence of MS specifically in US children has been reported at 0.51 per 100,000 person-years. The relapsing–remitting form of MS is much more common than the primary progressive form in pediatric patients. In addition to optic neuritis, children presenting with MS may have accompanying ataxia, brainstem involvement, and encephalopathy, making it difficult to distinguish MS from other acquired demyelinating syndromes such as ADEM. Many important studies have evaluated the risk of conversion to MS in children who present with first time optic neuritis, a question that understandably is of great concern to the parents. The conversion rate to multiple sclerosis in children has not been prospectively evaluated. However, as with adults, T2 lesions on MRI scan outside the visual system at presentation are associated with an increased risk of developing MS. In addition, older age at presentation of optic neuritis has been found to be an independent risk factor for increased likelihood of conversion to MS.
Demyelination in ADEM is polyfocal and may include optic neuritis, encephalopathy, and irregular, large MRI lesions involving the white matter and potentially deep gray matter. Clinically the child may present rapidly, often after an illness, with change in mental status, irritability, fever, and neurological findings consistent with multifocal brain inflammation. ADEM is considered classically to be a monophasic condition, although multiphasic ADEM has been described. Distinguishing ADEM from other demyelinating syndromes may be difficult at presentation. Recent studies have demonstrated that a high proportion of children with ADEM may be positive for antibodies to myelin oligodendrocyte glycoprotein (MOG) which become undetectable at follow-up. Presence of MOG-Ig antibodies may be associated with a more favorable prognosis.
Neuromyelitis optica (NMO) or Devic’s disease is a central nervous system inflammatory disorder that predominantly affects the optic nerves and spinal cord with the typical presentation of loss of vision or symptoms of transverse myelitis such as weakness in the arms or legs which may occur simultaneously, sequentially, or in isolation. The pathogenesis of NMO is distinct from MS, and in about 70% of cases it is associated with an NMO-IgG autoantibody which targets aquaporin-4 water channels (AQP4) expressed in astrocytes. The NMO-IgG antibody is not present in patients with MS.
NMO appears to affect predominantly female patients and NMO-optic neuritis is associated with more profound, irreversible vision loss. OCT reveals more severe rNFL thinning and evidence of microcystic macular edema in NMO-optic neuritis compared with MS-optic neuritis. NMO should be considered in any case with severe bilateral optic neuropathy, particularly with evidence of transverse myelitis, although optic neuritis may precede the onset of transverse myelitis. The term NMO spectrum disorder (NMOSD) is used for those cases with some, but not all, of the disease-defining features and includes patients in whom NMO overlaps with autoimmune conditions such as lupus. The diagnostic criteria for adult NMOSD have been updated recently by international consensus, with several caveats that distinguish the adult from the pediatric disease presentation.
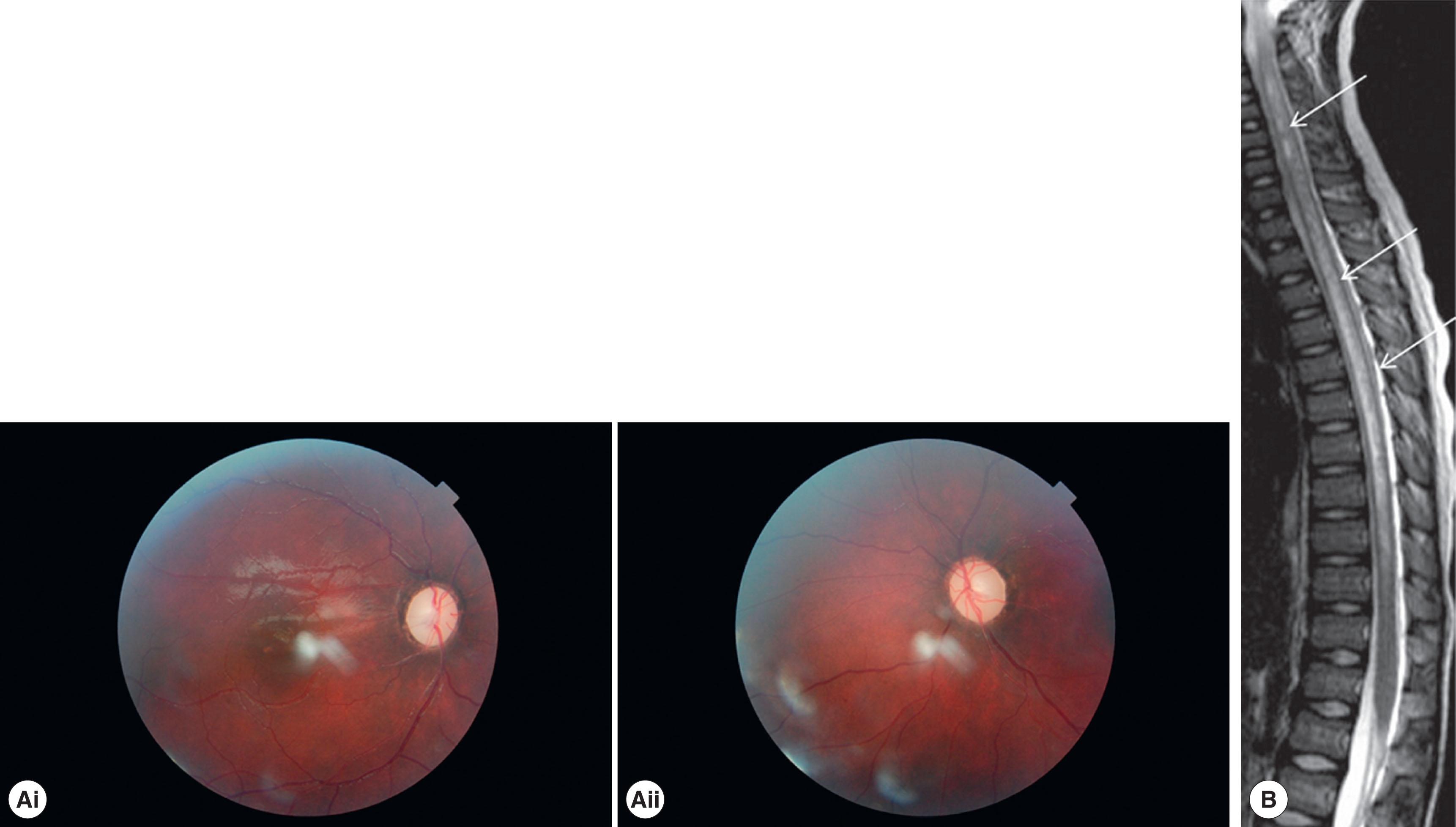
On MRI, NMO-optic neuritis may involve longer segments of the optic nerve which extend more posteriorly towards the optic chiasm compared with MS-optic neuritis. Importantly brain findings may be present in NMO, including large tumefactive lesions, but the periventricular white matter lesions seen in typical MS are generally not present. Spinal cord involvement is classically characterized by longitudinally extensive transverse myelitis involving three or more vertebral segments ( Fig. 56.4 ).
Standard corticosteroid treatment may not be effective and plasma exchange or IVIG may be required for an acute attack. Long-term immunosuppression to prevent relapse is the goal of therapy using agents such as rituximab, mycophenolate mofetil, and azathioprine and avoiding those MS agents thought to exacerbate NMO such as fingolimod. Further, in a recent retrospective review of 60 patients with NMO spectrum disorder, the authors found that complete recovery from a severe attack was facilitated by earlier use of plasma exchange as part of the treatment regimen distinguishing treatment strategies for this condition from other demyelinating conditions.
A new demyelinating disease phenotype in the context antibodies to the myelin oligodendrocyte oligoprotein (MOG-IgG+) has been defined with the advent of commercially available testing. The clinical presentation may include features that overlap with other demyelinating conditions such as ADEM in younger children, optic neuritis, and transverse myelitis, which highlights the critical role that antibody testing now has in establishing the correct diagnosis. The neuroimaging findings include extensive lengths of optic nerve enhancement, perineural enhancement, ADEM, and transverse myelitis ( Fig. 56.5 ). In a cohort of 87 MOG-IgG+ patients from the Mayo clinic, one of the largest studies of this disorder, approximately one-third of the patients were under the age of 18 years, with the youngest affected patient being 2 years of age. The clinical manifestations of optic neuritis included pain at presentation in 86%, and optic nerve edema in 86%. The average visual acuity at its nadir was counting fingers (CF) and final visual acuity was 20/30. In the evaluation of these patients, none had oligoclonal bands, and many developed recurrent attacks. In a separate study of 110 patients of whom 58 were children the authors found that visual outcomes were better in patients under 18 years of age compared with older patients. In a cohort study of children comparing visual outcomes of seronegative optic neuritis, MOG-IgG+ optic neuritis, and NMO-associated optic neuritis, the visual recovery in seronegative and MOG-IgG+ optic neuritis was better than 20/25 in the vast majority of patients compared with aquaporin 4-associated optic neuritis, but that both MOG-IgG+ and aquaporin-4-associated optic neuritis resulted in more significant retinal nerve fiber layer thinning on OCT. Treatment recommendations include IV corticosteroid followed by a long oral steroid taper, plasma exchange, IVIG, and consideration of steroid-sparing agents for chronic immunosuppression, including mycophenolate mofetil and rituximab.

Para-infectious optic neuritis may follow a febrile illness both in children and in adults. In children, symptoms of optic neuritis generally present 1–2 weeks after the febrile illness with either unilateral or bilateral visual loss and the presence of optic nerve edema. Para-infectious optic neuritis has been reported in association with Mycoplasma pneumoniae , varicella, rubeola, mononucleosis, and influenza B infection. This form of optic neuritis is often robustly responsive to corticosteroid treatment and the presumed pathogenesis is an autoimmune process rather than primary infection of the optic nerves. Although visual recovery is favorable, many children will have residual optic atrophy after an episode.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here