Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]()
Evaluation of change in mental status requires simultaneous efforts towards (1) establishing a diagnosis; (2) identifying potential etiologies and addressing life-threatening contributors; and (3) managing symptoms to ensure patient safety. A careful history should be obtained, not only from the patient but also from a reliable informant who knows the patient’s baseline functional status and can describe the time course of the change. Many features can be used to differentiate among the different potential causes of mental status change ( Table 361-1 ). For example, delirium starts suddenly with symptoms of inattention and confusion that fluctuate throughout the day. In contrast, dementia and Alzheimer disease ( Chapter 371 ) are characterized by an insidious decline in cognitive function, often memory, with symptoms that are chronic and typically slowly progressive over time. An acute exacerbation of a psychiatric condition, such as depression or schizophrenia ( Chapter 362 ), is usually heralded by days or weeks of worsening symptoms. A wide range of infections, traumatic, metabolic, toxic, vascular, and space occupying lesions can cause stupor (see Table 373-2 ).
| FEATURE | DELIRIUM | ALZHEIMER DISEASE | DEPRESSION | PSYCHOTIC DISORDERS |
|---|---|---|---|---|
| Onset | Acute, over days to hours | Insidious, over months to years | Slow | Acute or slow |
| Course | Fluctuating; can be worse at night | Chronic and progressive | Episodic; can occur singly, repeatedly, or chronically | Chronic, with exacerbations |
| Duration | Hours to months | Months to years | Weeks to months | Months to years |
| Descriptive features | Confusion and inattention | Memory loss | Sadness, anhedonia | Loss of contact with reality |
| Consciousness | Altered | Clear | Clear | Clear |
| Attention | Impaired | Normal, except in late stages | May be impaired | May be impaired |
| Orientation | Fluctuates | Poor | Normal | Normal |
| Speech | Incoherent | Mild errors | Normal, slow | Normal, pressured |
| Thinking process | Disorganized | Impoverished | Normal | Disorganized |
| Illusions and hallucinations | Common (often visual) | Rare, except in late stages | Not usually | Common |
| Perceptions | Altered | Altered or normal | Normal | Altered |
| Psychomotor changes | Yes | No | Yes | Yes |
| Reversibility | Usually | Rarely | Possibly | Rarely |
| Electroencephalogram | Moderate to severe background slowing | Normal or mild diffuse slowing | Normal | Normal |
A careful mental status examination, including an assessment of mood, affect, and cognition, can help establish a diagnosis. A targeted additional evaluation ( Table 361-2 ) can help identify potential causes of acute deterioration in mental status and guide further diagnostic and therapeutic interventions.
| Perform cognitive testing and determine baseline cognitive functioning |
| Obtain a comprehensive history and perform a physical examination, including a careful neurologic examination for focal deficits and a search for occult infection |
| Review the patient’s medication list: check the side effects of all medications |
| Perform a laboratory evaluation (tailored to the individual): complete blood count, electrolytes, blood urea nitrogen, creatinine, glucose, calcium, phosphate, liver enzymes, oxygen saturation |
| Search for occult infection: physical examination, urinalysis, chest radiography, selected cultures (as indicated) |
When no obvious cause is revealed after these steps, further targeted evaluation is considered in selected patients, as follows:
|
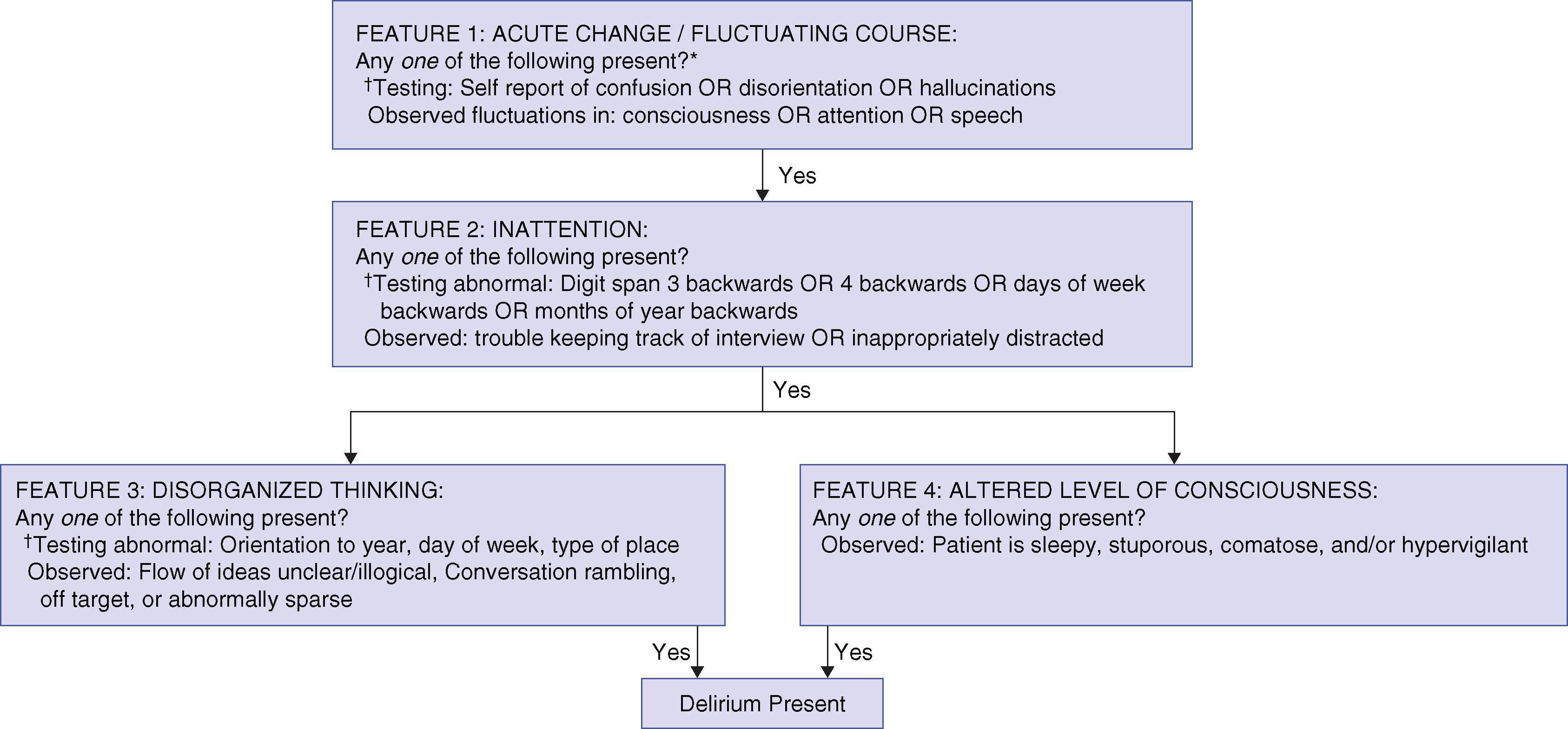
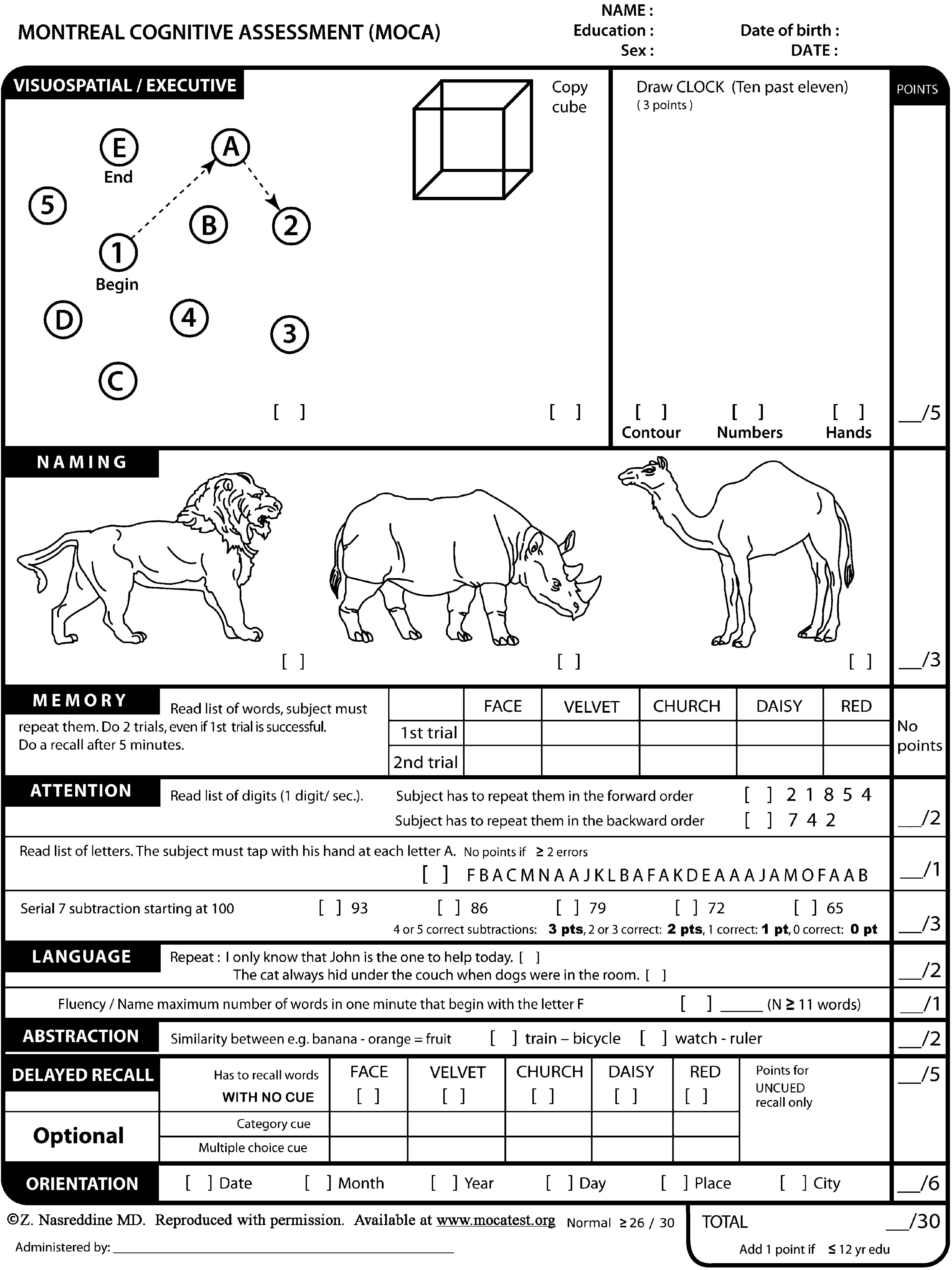
Ideally, cognitive testing should evaluate at least the general domains of attention, orientation, language, memory, visuospatial ability, and conceptualization. Attention should be assessed first by asking the patient to perform a task, such as repeating digits (normal span: more than five forward or more than three backward) or reciting the months backward (allow one error maximum); the remainder of cognitive testing would not be useful in an inattentive or delirious patient. If delirium is suspected ( Table 361-3 ), specific instruments can be used to confirm a diagnosis ( Fig. 361-1 ). If delirium is excluded, many brief, practical screening instruments are available for further cognitive testing. Historically, the most widely used instrument has been the Mini-Mental State Examination, a 19-item, 30-point scale that can be completed in 10 minutes. This copyrighted instrument now requires a per-use fee if the official version is used. Useful, brief alternative instruments include the Mini-Cog test ( Table 361-4 ), which can be completed in less than 5 minutes, or the Montreal Cognitive Assessment ( Fig. 361-2 ), which provides more detailed testing but which requires 15 to 20 minutes to complete; scores less than 26 indicate cognitive impairment. If dementia is suspected, further evaluation is required ( Chapter 371 ). The 15-item short-form Geriatric Depression Scale ( Table 361-5 ) can identify depressive symptoms requiring further evaluation ( Chapter 362 ).
| DSM-5 CRITERIA |
|
|
|
yes/ NO |
|
YES /no |
|
YES /no |
|
YES /no |
|
yes/ NO |
|
YES /no |
|
yes/ NO |
|
YES /no |
|
YES /no |
|
YES /no |
|
yes/ NO |
|
YES /no |
|
yes/ NO |
|
YES /no |
|
YES /no |
Delirium, which can occur at any age, is one of the most common presenting symptoms in acutely ill elders, in whom it is estimated to account for 30% of emergency evaluations. Mental status change often serves as a barometer of the underlying health of an older patient and is commonly the only symptom of serious underlying disease. A broad range of medical, neurologic, and psychiatric conditions can lead to delirium ( Chapters 362 and 371 ). A systematic approach aids in the evaluation of suspected delirium at all ages ( Fig. 361-3 ).
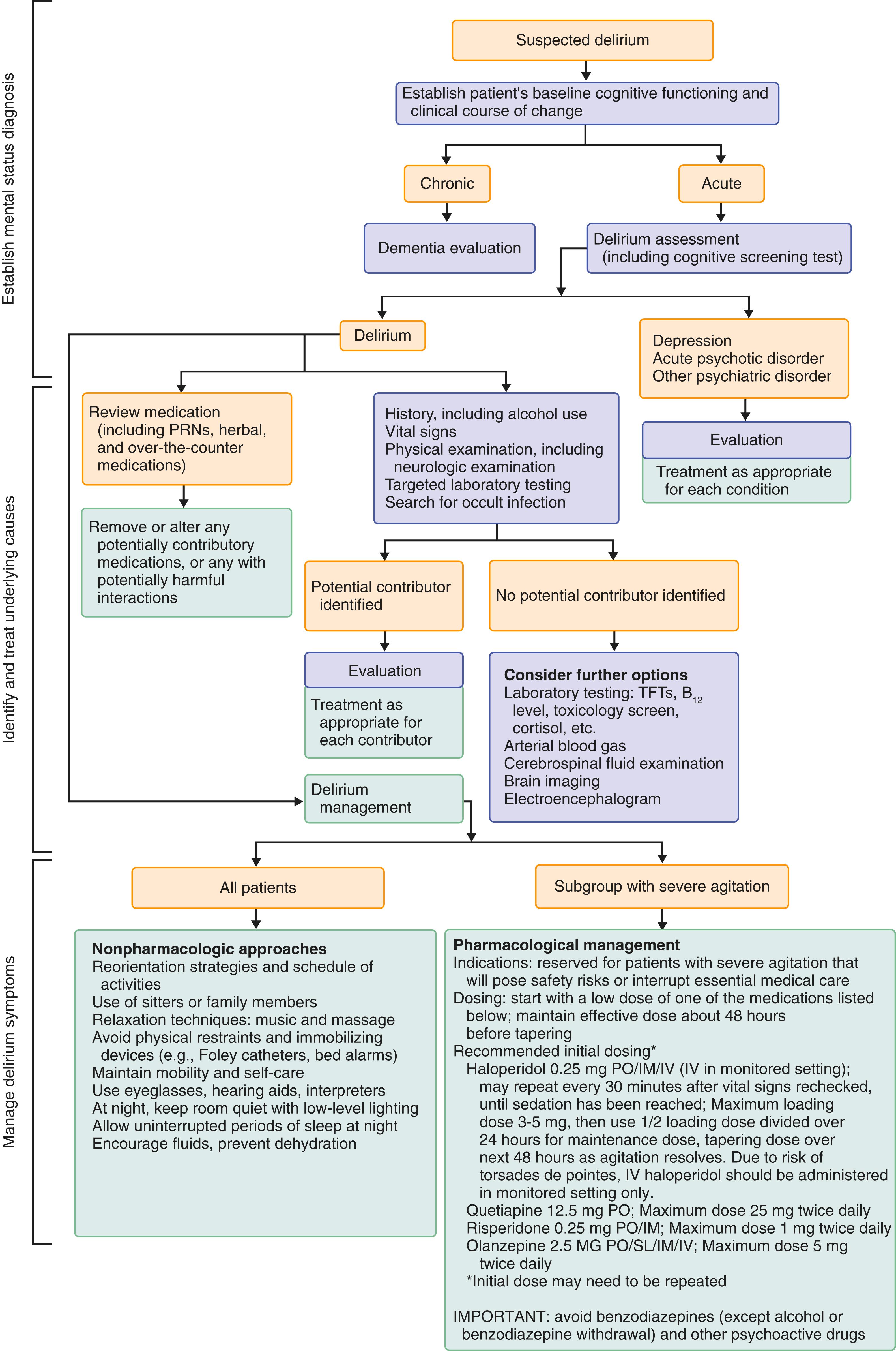
Delirium is a clinical syndrome (see Table 361-3 ) that is characterized as an acute disorder of attention and cognitive function. Delirium is the most frequent complication of hospitalization for elders, is a potentially devastating problem at any age, and is often unrecognized despite sensitive methods for its detection. The Confusion Assessment Method and abbreviated versions of it (see Fig. 361-1 ) can provide quick, simple, operationalized diagnostic approaches for delirium. The Confusion Assessment Method algorithm has a sensitivity of 94%, a specificity of above 85%, and high interrater reliability. Complications of delirium may be preventable, so rapid and accurate diagnosis is critical.
The prevalence of delirium varies widely by settings and age. For older adults in a general medical setting, the prevalence of delirium is estimated to be 23%, with higher rates when frequent surveillance is performed in older, surgical, and intensive care populations. For example, delirium occurs in 8 to 58% of postoperative patients, 50 to 70% of mechanically ventilated patients, and up to 82% of patients in medical intensive care units. Delirium is also noted in up to 38% of nursing home patients and in up to 88% of patients at the end of life.
The problem of delirium in hospitalized elderly patients has assumed particular prominence because patients aged 65 years and older currently account for more than 50% of all inpatient days of hospital care. Based on U.S. vital health statistics, delirium complicates hospital stays for at least 2.6 million adults age 65 and older and accounts for more than $164 billion in health care expenditures annually. For postoperative delirium, the estimated costs are $33 billion in the United States annually. Thus, delirium holds extensive economic and health policy implications.
Similar to other common geriatric syndromes ( Chapter 24 ), delirium usually has multiple causes. A search for the many potential underlying contributors requires clinical astuteness and a thorough medical evaluation, especially because many of these factors are treatable but may result in substantial morbidity and mortality if left untreated. The process is made more challenging by the frequently nonspecific, atypical, or muted features of the underlying illness in older persons. Delirium is commonly the only initial sign of an underlying life-threatening illness, such as pneumonia ( Chapter 85 ), urosepsis ( Chapter 263 ), or myocardial infarction ( Chapter 58 ), in the older population.
The basic pathogenesis of delirium remains unclear. Recent evidence suggests that interacting biologic factors result in disruption of large-scale neuronal networks in the brain, thereby leading to acute cognitive disruption and delirium. Some of the leading proposed mechanisms include disruption in neurotransmitter systems, systemic inflammation, neuronal inflammation, neuronal injury, physiologic stressors, metabolic derangements, and genetic factors. Many neurotransmitter systems are potentially involved, but relative cholinergic deficiency and dopamine excess are the most frequently linked. Inflammation may play an important role, with peripheral inflammation triggering neuroinflammation and microglial activation. Whether underlying factors such as preclinical dementia impart a vulnerability for the brain to “lose” the ability to protect itself in the face of infection or trauma, with the end result being an episode of delirium, or if delirium itself causes neuronal injury and death is unknown, but both of these potential links are supported by emerging data.
The development of delirium usually involves a complex interrelationship between a vulnerable patient with pertinent predisposing factors and exposure to noxious insults or precipitating factors. Delirium may develop in vulnerable patients, such as cognitively impaired or severely ill patients, after a relatively benign insult, such as a single dose of sleeping medication. Conversely, in patients who are not vulnerable, delirium may develop only after exposure to multiple noxious insults. The effects of these risk factors may be cumulative. Recognition of this multifactorial causation is important to the clinician because the removal or treatment of one factor in isolation usually is not sufficient to resolve the delirium. The full spectrum of vulnerability and precipitating factors should be addressed.
Factors that predispose patients to delirium include preexisting cognitive impairment or dementia ( Chapter 371 ), history of delirium, functional impairment, visual ( Chapter 391 ) or hearing impairment ( Chapter 396 ), multiple comorbid conditions, severe underlying illness, depression ( Chapter 362 ), history of a stroke or transient ischemic attack ( Chapter 376 ), alcohol use disorder ( Chapter 364 ), and advanced age. Dementia is an important and consistent risk factor for delirium; persons with dementia have a two-fold to five-fold increased risk for delirium, and 30 to 50% of delirious patients have underlying dementia.
Medications, which are the most common remediable causes of delirium, contribute to delirium in 40% of cases (Chapter 361). Insufficiency or failure of any major organ system, particularly renal or hepatic failure, can precipitate delirium. Surgical procedures are leading risk factors for delirium. Hypoxemia and hypercarbia have been associated with delirium. Clinicians must be attuned to occult respiratory failure, which in the elderly often lacks the usual signs and symptoms of dyspnea and tachypnea and can be missed by the measurement of oxygen saturation alone. Acute myocardial infarction ( Chapter 58 ) or heart failure ( Chapter 45 ) can be manifested as delirium in an elderly patient without the usual symptoms of chest pain or dyspnea. Occult infection is a particularly notable cause of delirium. Older patients frequently fail to mount the febrile or leukocytotic response to infection, and clinicians must assess them carefully for signs of pneumonia ( Chapter 85 ), urinary tract infection ( Chapter 263 ), endocarditis ( Chapters 61 ), abdominal abscess ( Chapter 128 and 137 ), or infected joints ( Chapter 251 ). Studies in older adults presenting to the emergency department with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection ( Chapter 336 ) found that delirium is a frequent presenting symptom, in some cases without typical SARS-CoV-2 symptoms or signs, such as fever or shortness of breath. A variety of metabolic disorders may contribute to delirium, including hypernatremia and hyponatremia ( Chapter 102 ), hypercalcemia ( Chapter 227 ), acid-base disorders ( Chapter 104 ), hypoglycemia ( Chapter 211 ) and hyperglycemia ( Chapter 210 ), and thyroid ( Chapter 207 ) or adrenal disorders ( Chapter 209 ). Immobilization and immobilizing devices (e.g., indwelling bladder catheters, physical restraints, bed alarms) are important factors in precipitating delirium. Dehydration and volume depletion and nutritional decline during hospitalization (e.g., weight loss, fall in serum albumin concentration) are well-documented factors contributing to delirium. Drug and alcohol withdrawal are important and often unsuspected causes of delirium in the elderly. Environmental factors, such as unfamiliar surroundings, sleep deprivation, deranged schedule, frequent room changes, sensory overload, and sensory deprivation, may aggravate delirium in the hospital. Psychosocial factors, such as depression, psychological stress, pain, and lack of social supports, also may precipitate delirium.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here