Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Organ transplantation is the only viable lifesaving option for many patients with end-stage organ failure. The progress in transplant procedures and post-transplant care has resulted in decreased morbidity and mortality after transplantation. More patients with end-stage organ failure are now being placed on the waiting list, resulting in more need for lifesaving organs.
The sources of organs are either from living donors, which are discussed in another chapter, or deceased donors, defined as donation from those with neurologic criteria or brain-dead donors (DBD), and donation with cardiocirculatory criteria or donation after cardiac death donors (DCD). In this section we discuss organ recovery from deceased donors and focus on the process and procedures to safely recover abdominal organs for transplantation.
After the initial evaluation of the donor and confirmatory tests for brain death, and after obtaining consent for donation, the donor is brought to the operating room for recovery of assigned organs.
A long midline incision is made from the suprasternal notch to the symphysis pubis. The sternum is split with a sternal saw. After control of sternal bleeding, a sternal retractor is placed to open the sternum, and a Balfour retractor is placed to open the abdominal cavity. At this point, thoracic and abdominal recovery teams can work simultaneously on both sides of the diaphragm ( Fig. 24.1A and B ) .
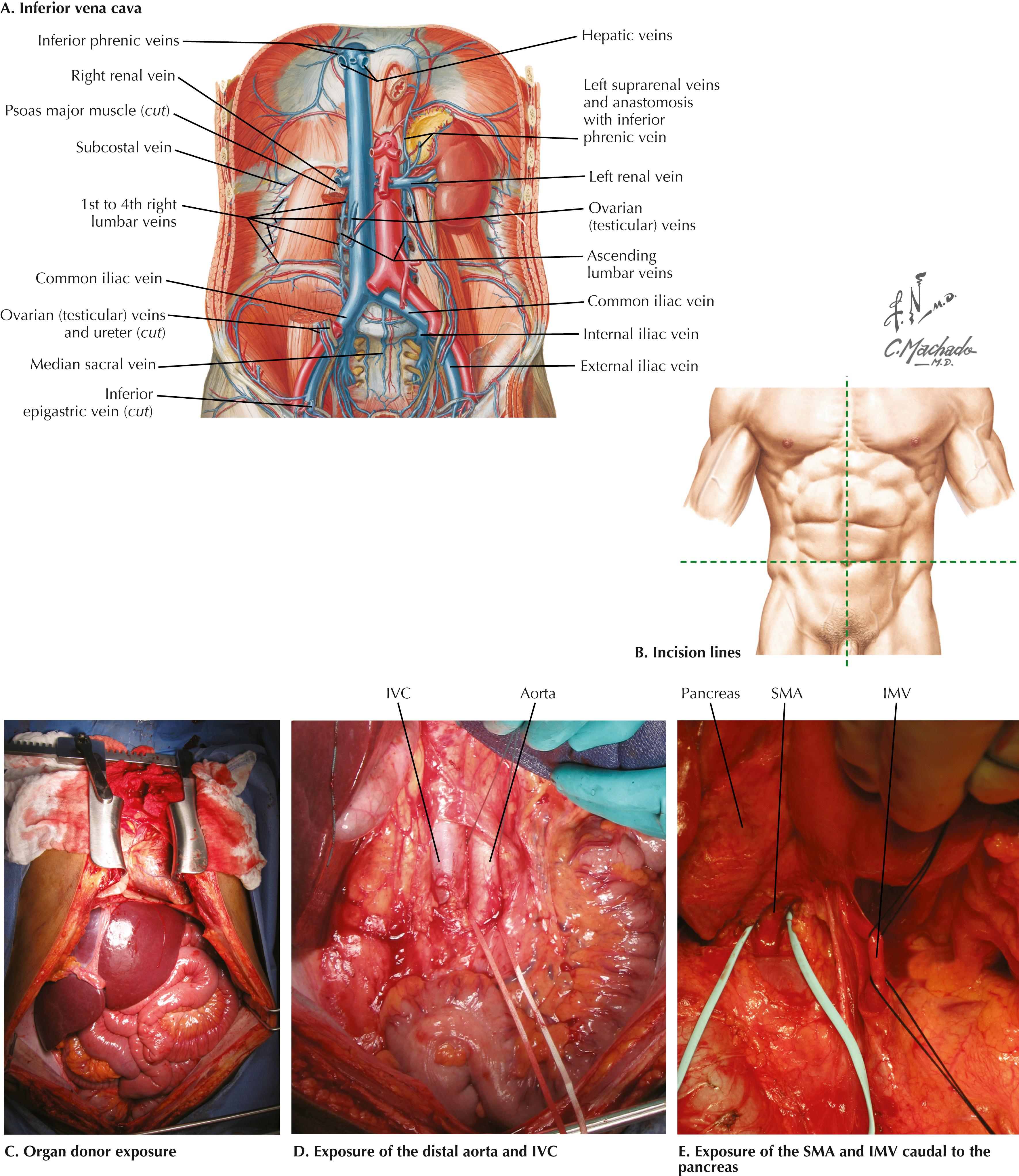
After the initial exploration for possible pathology, the umbilical ligament is divided between 0-silk ties, and the falciform ligament is divided to the level of the suprahepatic inferior vena cava (IVC). The left triangular ligament is divided to the level of left hepatic vein and IVC, taking care not to injure the stomach. The right triangular ligament is divided and the attachments between the right lobe of the liver and retroperitoneum are divided to the level of right hepatic vein. At this point, the retrohepatic IVC and adrenal gland can be visualized.
It is good practice to dissect the lower abdominal aorta and prepare it for cannulation (see Fig. 24.1A, C–E ). In cases of donor instability, there may be a need to cannulate and flush the organs in an immediate fashion. It is also important to dissect and isolate the supraceliac aorta because it may not be possible to cross-clamp the thoracic aorta at the time the organs are flushed with the preservative solution. For isolation of the supraceliac aorta, the diaphragmatic muscles of the crura are divided longitudinally and the aorta is visualized. After dissection, the aorta can be isolated with umbilical tape should the need arise to clamp the aorta below the diaphragm.
The practice of recovery of abdominal organs can be different in transplant programs. Accordingly, the two methods of initial dissection of the recovery are called classic/standard, or rapid, technique.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here