Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Multiple types of cutaneous cysts have been described
Cutaneous cysts present as circumscribed dermal or subcutaneous papules or nodules
Histologic features of the cyst lining and the anatomic location determine the type of cyst
Cysts may be lined by either stratified squamous epithelium or non-stratified squamous epithelium; cystic structures without an epithelial lining are better classified as pseudocysts
Treatment of cysts, when indicated, is primarily surgical
Cysts are common cutaneous lesions. Patients with cysts may present to clinicians because of medical or cosmetic concerns, or due to discomfort from mechanical irritation or inflammation of the cyst. The definitive diagnosis of a cyst requires histologic examination, as many other dermal and subcutaneous tumors can form cyst-like nodules. Cysts can be classified by anatomic location (as they may occur in virtually any organ of the body), by embryologic derivation, or by histologic features. As the histologic features determine the definitive diagnosis, that scheme will be used in this chapter, which is limited to cutaneous cysts.
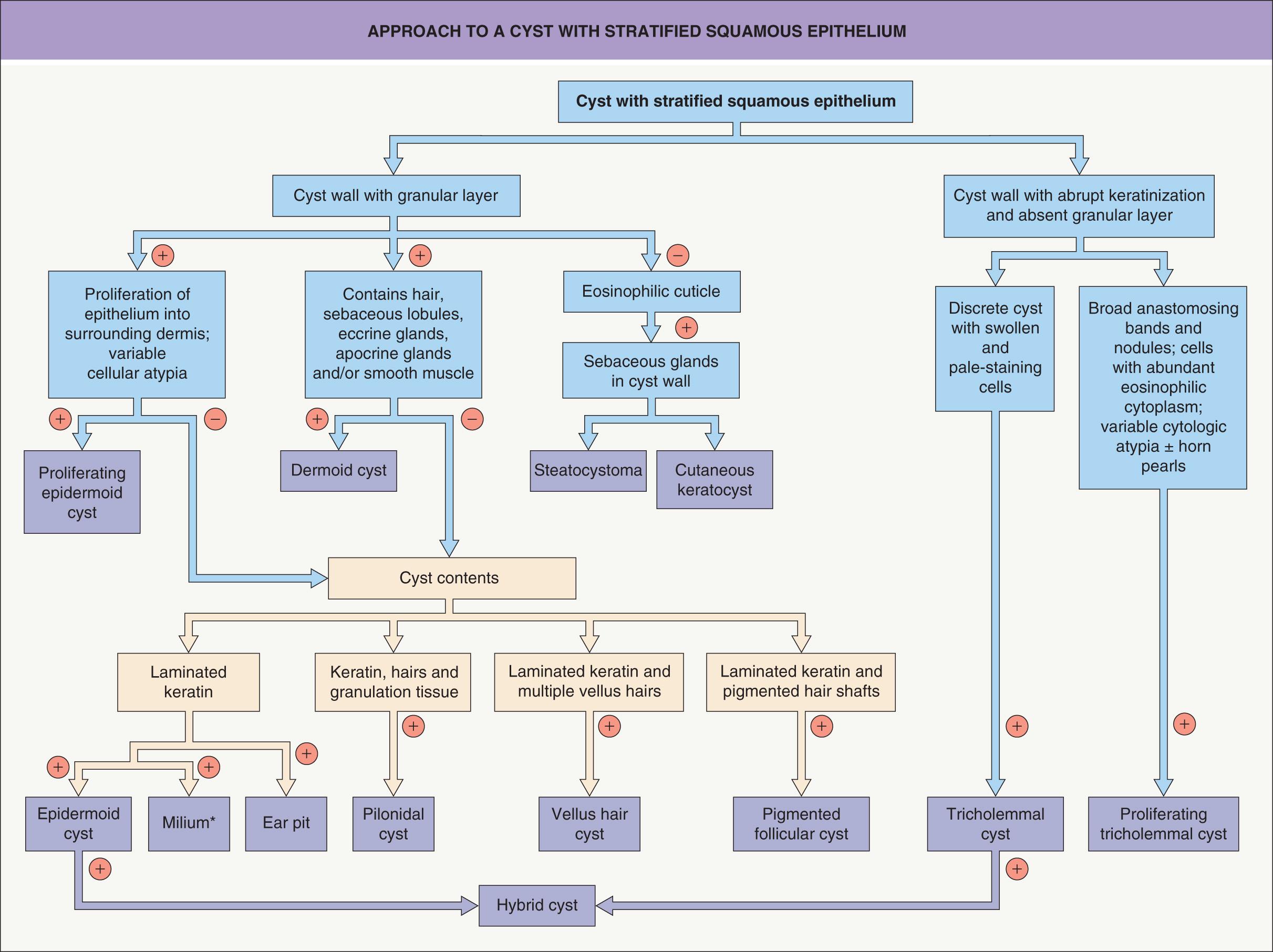
True cysts have an epithelial lining that may be composed of stratified squamous epithelium or other forms of epithelia. Some “pseudocysts” have no epithelial lining at all. Cutaneous cysts can be divided into three main categories based on the presence or absence and composition of the cyst wall ( Table 110.1 ; Fig. 110.1 ). Many non-dermatologists refer to epidermoid and pilar cysts as “sebaceous cysts”, believing erroneously that the hydrated white keratinized contents of many epithelial-lined cysts is of sebaceous origin. The only true sebaceous cyst is the steatocystoma. The term “sebaceous cyst” is best avoided.
| THE THREE MAIN CATEGORIES OF CUTANEOUS CYST | ||
|---|---|---|
| Category | Type | Most common location |
| Stratified squamous epithelium | Epidermoid (infundibular) cyst | Face; upper trunk |
| Milium Tricholemmal cyst Proliferating tricholemmal cyst Proliferating epidermoid (infundibular) cyst |
Face Scalp Scalp (favors elderly women) Pelvic (anogenital) |
|
| Vellus hair cyst Steatocystoma Cutaneous keratocyst Pigmented follicular cyst Dermoid cyst |
Trunk (chest) Trunk; axillae; groin No characteristic location Face (men) Face along embryonic fusion planes, e.g. lateral eyebrow (infants) |
|
| Verrucous cyst | Face, upper trunk (HPV-infected epidermoid cysts) | |
| Ear pit cyst Pilonidal cyst |
Preauricular Upper gluteal cleft; sacrococcygeal area |
|
| Non-stratified squamous epithelium | Hidrocystoma | |
Bronchogenic cyst |
Face (lower eyelid, cheek) Face (eyelid margin) Suprasternal notch (infants) Midline anterior neck Lateral neck; preauricular; mandibular (teenagers, young adults) |
|
| Cutaneous ciliated cyst | Lower extremities (young women) | |
| Ciliated cyst of the vulva Median raphe cyst Omphalomesenteric duct cyst |
Labia majora Ventral glans and penile shaft Umbilical; periumbilical |
|
| Absence of epithelium (pseudocysts) | Mucocele Digital mucous cyst (pseudocyst) |
Oral mucosa (lower labial) Dorsal aspect of distal phalanx of finger (occasionally toe) |
| Ganglion Pseudocyst of the auricle Cutaneous metaplastic synovial cyst (pseudocyst) |
Wrist Scaphoid fossa of the ear (adult men) Sites of surgical trauma |
|
▪ Infundibular cyst ▪ Epidermal cyst ▪ Epidermal inclusion cyst
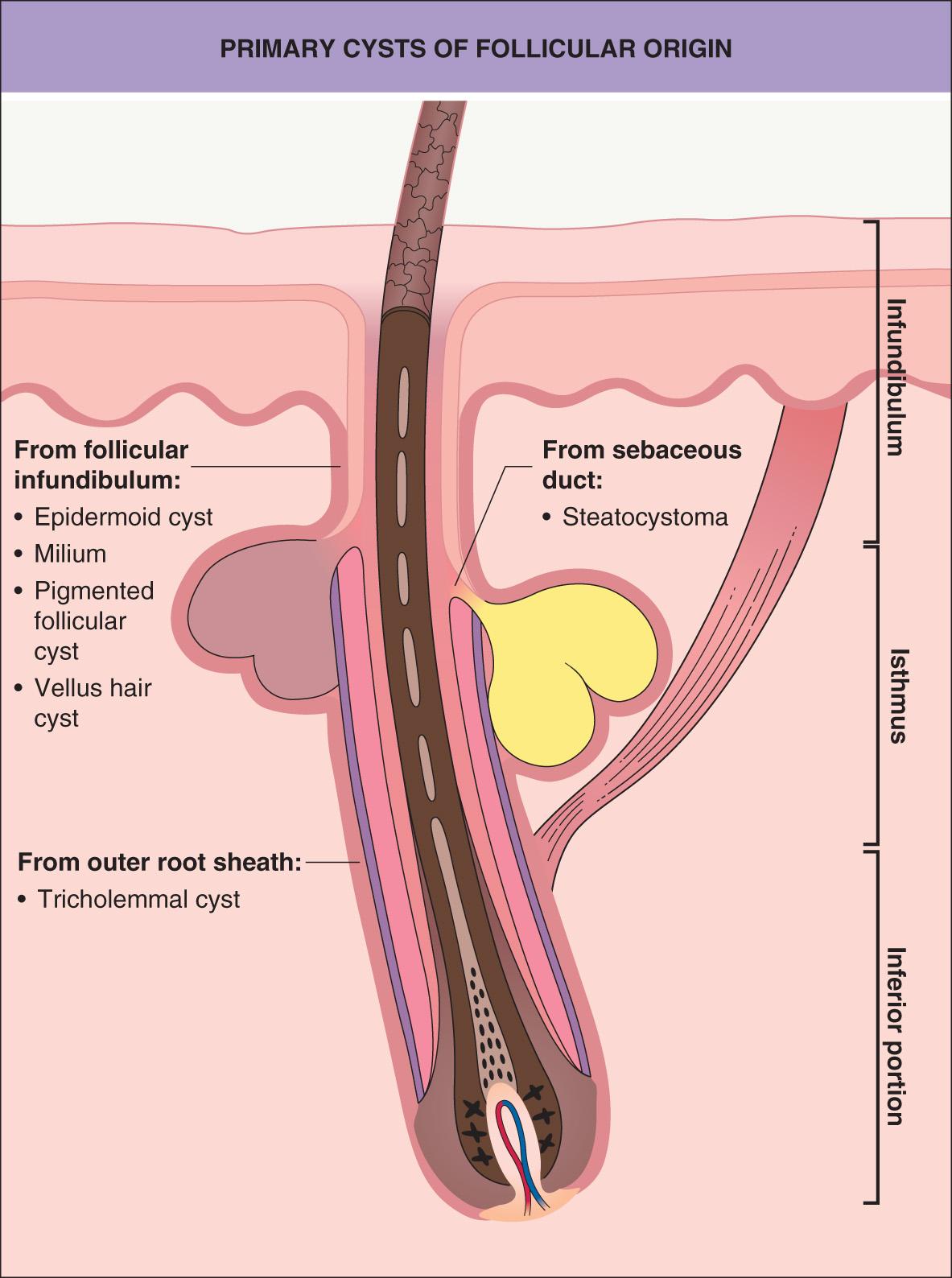
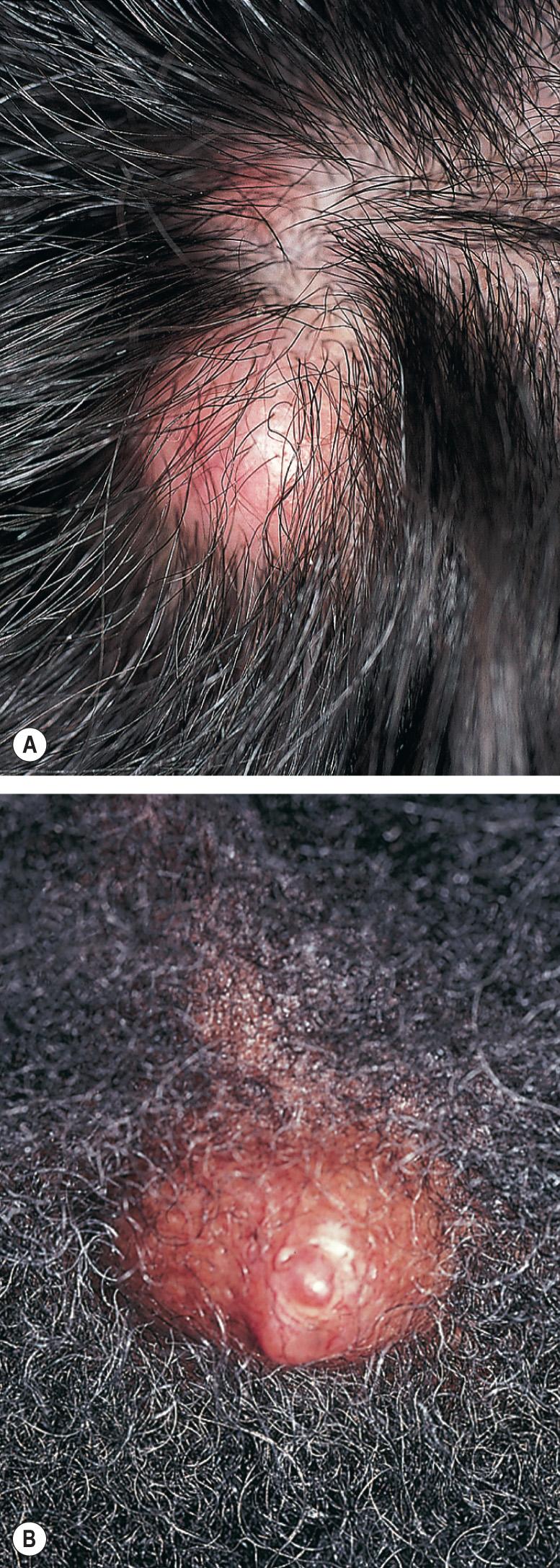
Epidermoid cysts are the most common cutaneous cysts. They can occur anywhere on the skin, but are most common on the face and upper trunk. These lesions are well-demarcated, skin-colored to yellowish dermal nodules, and they may have a clinically visible punctum representing the follicle from which the cyst is derived ( Fig. 110.2 ). Epidermoid cysts range from a few millimeters to several centimeters in diameter. Tiny superficial epidermoid cysts are known as milia (see below). These cysts derive from the follicular infundibulum, hence the synonym infundibular cysts ( Fig. 110.3 ). They may be primary, or they may arise from disrupted follicular structures or traumatically implanted epithelium (hence the synonym epidermal “inclusion” cyst).

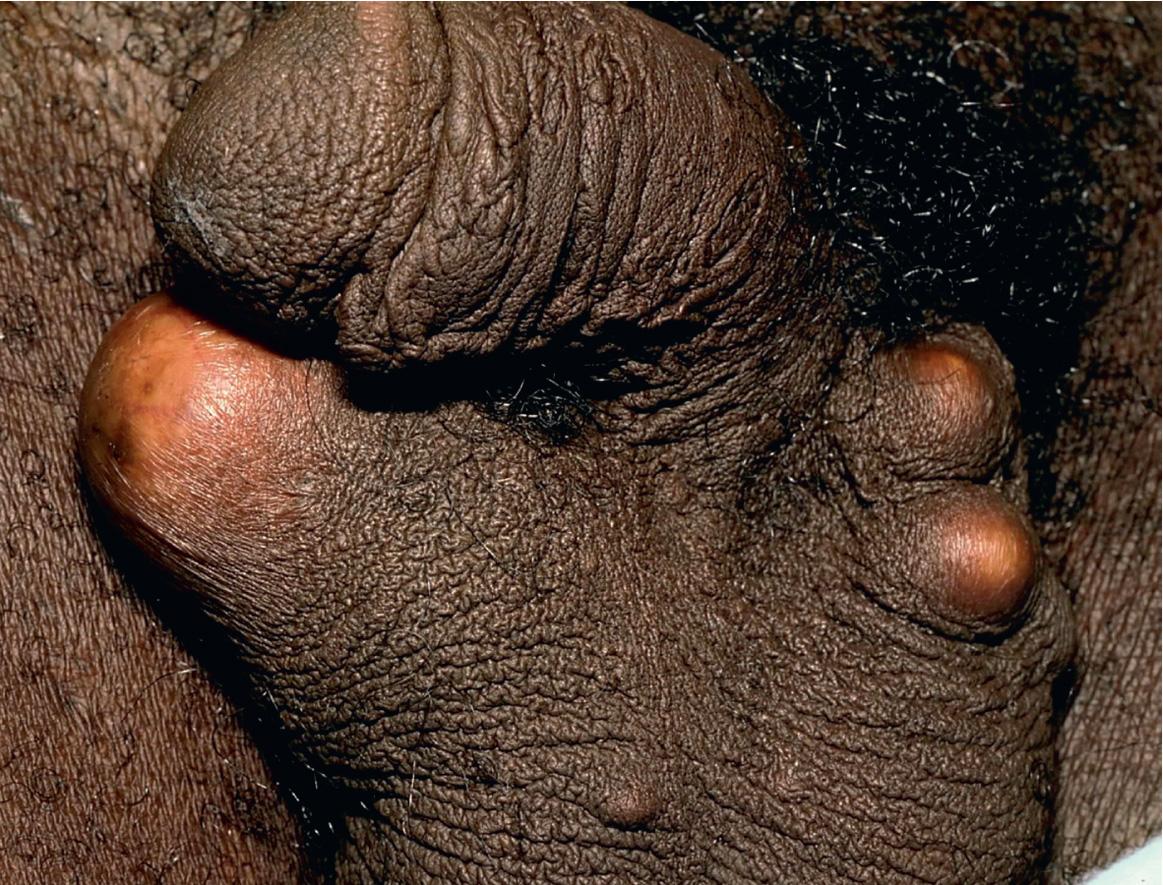
As follicular disruption is important in the pathogenesis of many epidermoid cysts, multiple epidermoid cysts may occur in individuals with a history of significant acne vulgaris. Multiple cysts may also occur in the setting of Gardner syndrome (familial adenomatous polyposis) and in basal cell nevus syndrome . Patients receiving BRAF inhibitors, both non-selective (e.g. sorafenib) and selective (e.g. vemurafenib) can develop multiple epidermoid cysts or milia, often on the face . Multiple scrotal cysts ( Fig. 110.4 ) may lead to scrotal calcinosis via dystrophic calcification .
Non-inflamed epidermoid cysts are usually asymptomatic, but with pressure, cyst contents may be expressed that may have an objectionable odor. Rupture of the cyst wall can result in an intensely painful inflammatory reaction, and this is a common reason for presentation to a physician ( Fig. 110.5 ). Development of a basal cell carcinoma (BCC) or squamous cell carcinoma (SCC) within an epidermoid cyst is a very rare event.

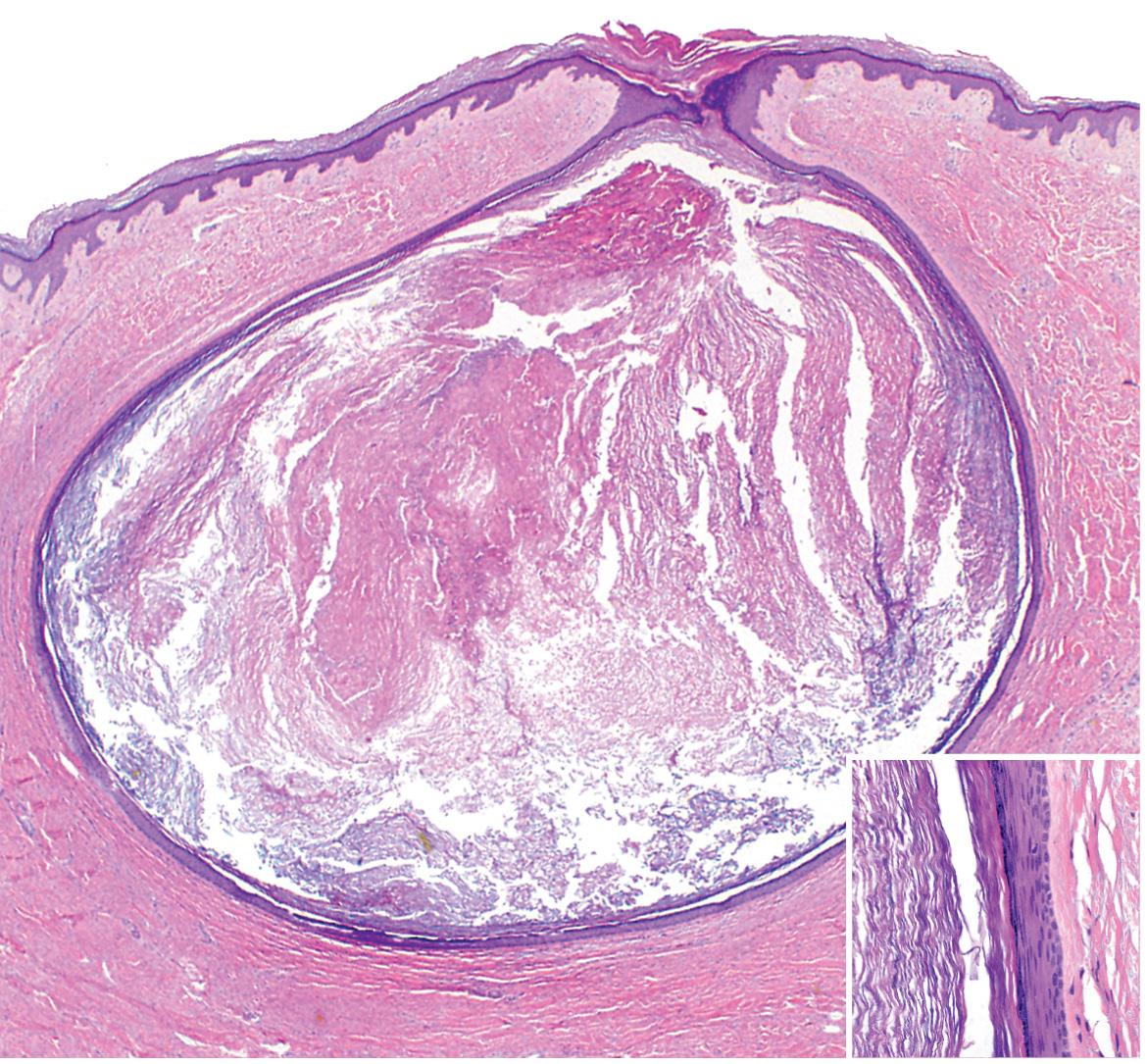
Histologic examination shows a cystic cavity filled with laminated keratin lined by a stratified squamous epithelium that includes a granular layer ( Fig. 110.6 ). A surrounding inflammatory response with both acute and chronic granulomatous inflammation as well as variable fibrosis may be seen as evidence of prior rupture. In individuals with Gardner syndrome, some cysts have, as a characteristic feature, columns of pilomatricoma-like shadow cells projecting into the cyst cavity . Infection of the cyst's epithelium with human papillomavirus can lead to irregular acanthosis with a verrucous appearance of the cyst wall (“verrucous cyst”).
If treatment is desired, excision is curative. Removal may be accomplished by simple excision, or incision and expression of the cyst contents and wall through the surgical defect. If the entire cyst wall is not removed, the cyst may recur. Excision is preferred when the cyst is non-inflamed (“cold”). Inflamed epidermoid cysts may require incision and drainage, and occasionally, antibiotic therapy. Intralesional injections of triamcinolone may speed resolution of the inflammation.
Dilated pore of Winer presents as a single dilated comedo, primarily occurring on the face of adults.
A dilated follicular opening, filled with keratinous debris and lined by squamous epithelium with a granular layer, is seen. The lining is acanthotic with finger-like projections pushing into the surrounding dermis.
Although there is usually a more papular component, an obvious pore can be seen in a pilar sheath acanthoma, trichoepithelioma, and large-pore BCC.
If treatment is desired, excision is curative.
Pilar sheath acanthoma, which presents as a papule with a central comedo-like opening, is discussed in Ch. 111 . While pilar sheath acanthomas are not true cysts, some lesions may have a partly cystic architecture.
If treatment is desired, excision is curative.
Milia are small superficial cysts and are quite common, occurring in individuals of all ages. They may originate from the infundibulum of hair follicles or from eccrine ducts, and in the mouth from minor salivary gland ducts or from epithelium entrapped within embryologic fusion planes. Milia present as 1–2 mm, firm, white to yellow, subepidermal papules ( Fig. 110.7 ).

Between 40% and 50% of infants will have milia, most commonly on the face. Most milia in newborns will resolve spontaneously during the first 4 weeks of life. Milia in newborns may also occur on the hard palate (Bohn nodules) or on the gum margins (Epstein pearls). These also resolve spontaneously. Milia may occur as a primary phenomenon, especially on the face, or as secondary phenomena following blistering processes (e.g. porphyria cutanea tarda, epidermolysis bullosa acquisita) or superficial ulceration from trauma or cosmetic procedures. Milia may also occur in areas of topical corticosteroid-induced atrophy and in follicular mycosis fungoides.
Milia en plaque is characterized by multiple milia within anerythematous edematous plaque, and the most common location is the postauricular area. Numerous milia in an infant may be a sign of oral–facial–digital syndrome type 1, an X-linked disorder that is lethal in males, in which milia are associated with facial and skull malformations, cleft lip and palate, a lobulated tongue, mental retardation and polycystic kidneys; the associated alopecia follows the lines of Blaschko on the scalp. Milia are also seen in the setting of a number of other syndromes, including the BCC-associated syndromes, Rombo syndrome and Bazex–Dupré–Christol syndrome, as well as atrichia with papular lesions, Loeys–Dietz syndrome, basaloid follicular hamartoma syndrome, Basan syndrome, and a subset of Brooke–Spiegler syndrome (Rasmussen syndrome).
Histologic features are those of a small epidermoid cyst with a stratified squamous epithelial lining that includes a granular layer. The cyst contents consist of laminated keratin.
Milia may be removed by incising the epidermis over the milium with a needle, scalpel or lancet and expressing the milium. The latter can be aided by the use of a comedo extractor. Laser ablation and electrodesiccation are also reported options. For multiple facial milia, topical retinoid therapy may be helpful in reducing the number of new milia and aiding in the ease of removal.
▪ Trichilemmal cyst ▪ Pilar cyst ▪ Wen▪ Isthmus–catagen cyst
Tricholemmal cysts are clinically indistinguishable from epidermoid cysts, but they are fourfold to fivefold less common. Ninety percent of tricholemmal cysts are located on the scalp ( Fig. 110.8A ). They may be solitary, but frequently are multiple, and they may be inherited as an autosomal dominant trait.
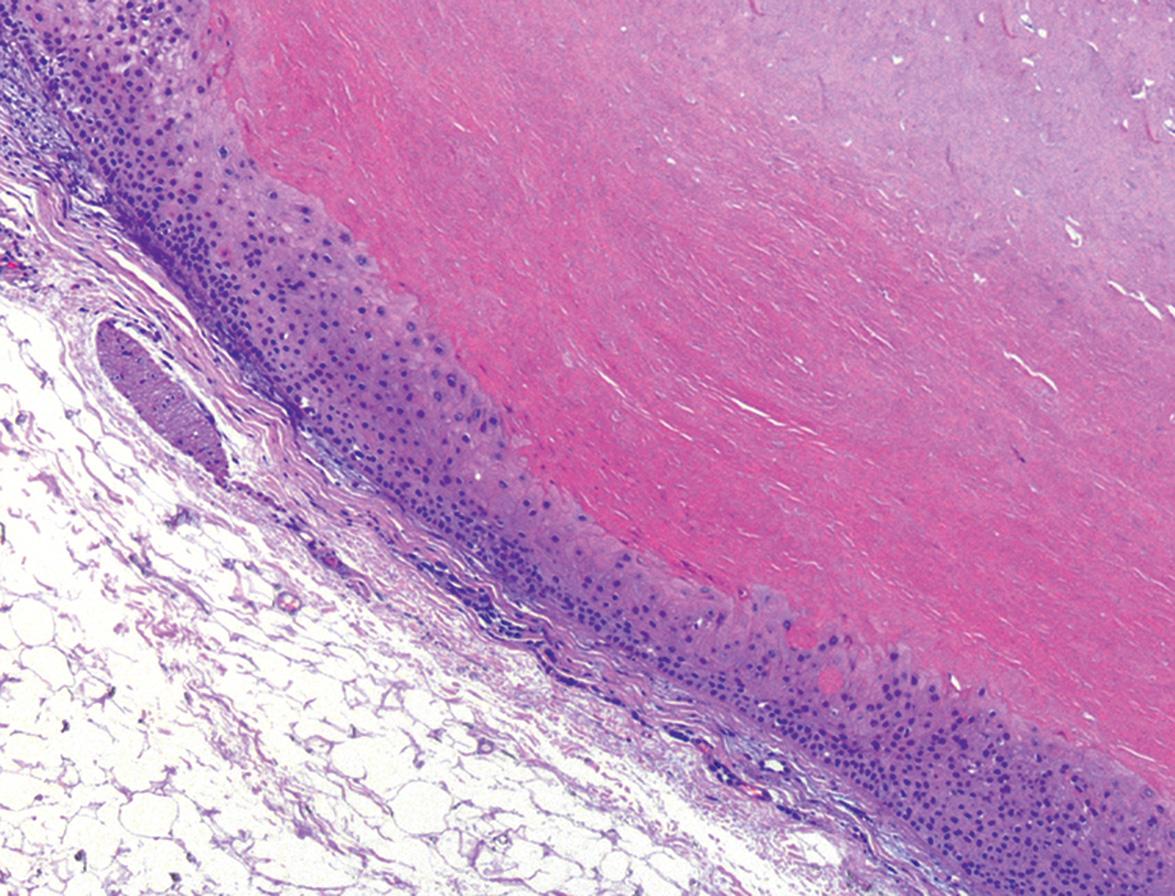
The walls of tricholemmal cysts show keratinization analogous to that of the outer root sheath of the hair follicle at the isthmus and the sac surrounding catagen and telogen hairs (hence the synonym isthmus–catagen cyst). Tricholemmal cysts are lined by stratified squamous epithelial cells without visible intracellular bridges that become swollen and pale close to the cystic cavity and show abrupt keratinization without an intervening granular layer ( Fig. 110.9 ). The cyst contents consist of homogeneous, eosinophilic, compact material that can contain foci of calcification. A foreign body giant cell response may surround the cyst if prior wall rupture has occurred.
Treatment is by excision. Tricholemmal cysts typically “deliver” themselves through an incision without rupture more easily than do epidermoid cysts, and, therefore, the distinction between a tricholemmal cyst and an epidermoid cyst can often be correctly made at the time of excision.
▪ Proliferating trichilemmal cyst ▪ Proliferatingtricholemmal tumor ▪ Proliferating pilar tumor ▪ Proliferatingfollicular cystic neoplasm
A proliferating tricholemmal cyst classically occurs as a slow-growing nodule on the scalp (see Fig. 110.8B ). Ninety percent occur on the scalp and ~85% occur in women, with a median age of 63 years . Proliferating tricholemmal cysts vary in size from a few millimeters to up to 25 cm in diameter. These tumors generally behave in a benign fashion, although on occasion, aggressive local growth with recurrences and metastases has been observed . Extremely rarely, spindle cell carcinomas may develop within a proliferating tricholemmal cyst . Distant metastases are rare in proliferating tricholemmal cysts, but over 30 such cases have been reported .
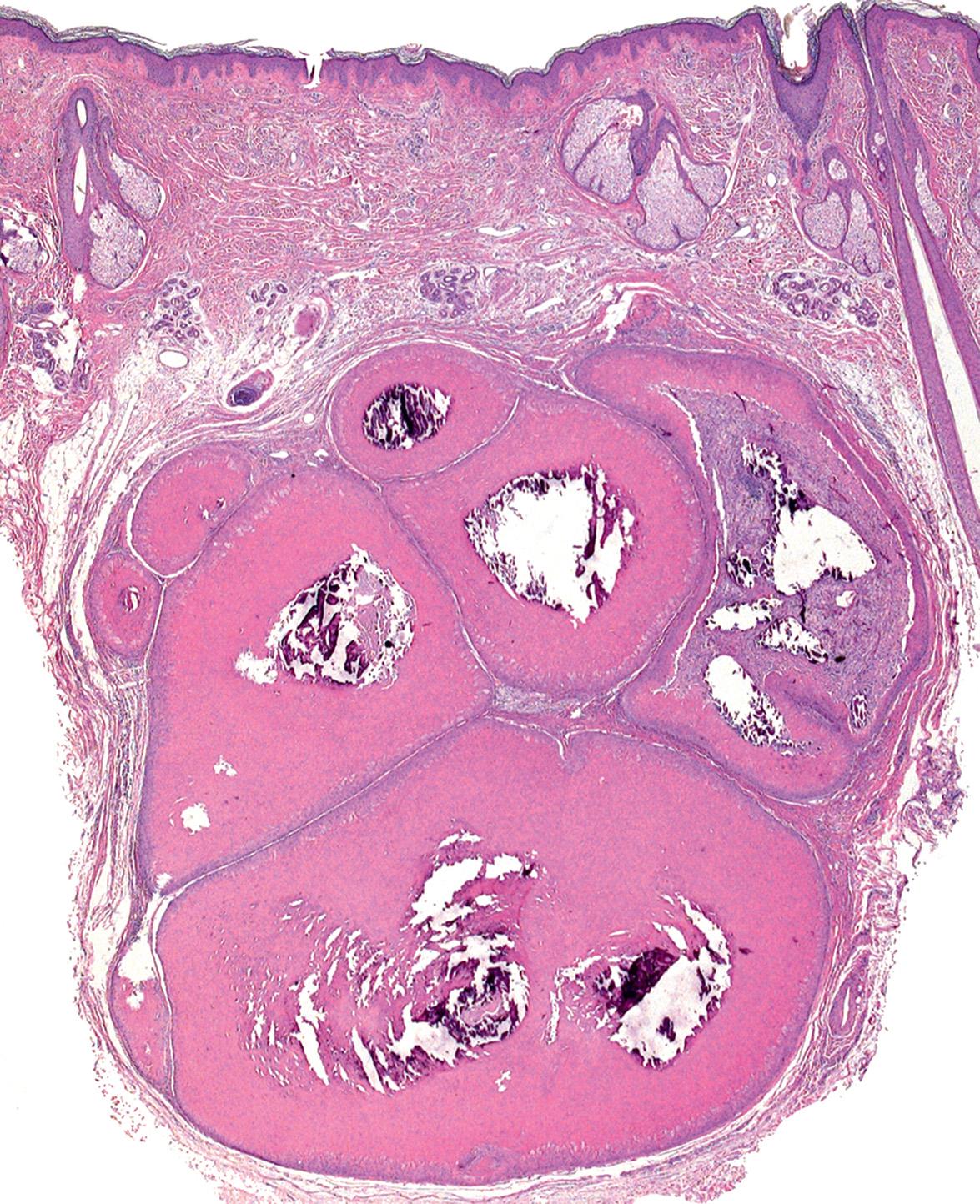
The histologic features of a proliferating tricholemmal cyst consist of broad anastomosing bands and nodules of squamous epithelium ( Fig. 110.10 ). The epithelium consists of a proliferation of cells with abundant eosinophilic cytoplasm; the cells undergo abrupt keratinization and form dense homogeneous keratin that fills cystic spaces. There may be areas of epidermoid keratinization with formation of horn pearls as well as areas of foreign body giant cell reaction. One-quarter of cases show an epidermal connection . Cytologic atypia can vary markedly. Most tumors show well-circumscribed, pushing borders surrounded by compressed collagen. The lack of infiltrative growth into the surrounding stroma and abrupt tricholemmal keratinization helps to differentiate these cysts from SCC. Areas of marked atypia and infiltrative borders are features associated with a potential for aggressive behavior .
Treatment is by complete surgical excision.
▪ Proliferating epithelial cyst ▪ Proliferatinginfundibular cyst
Proliferating epidermoid cysts were first described in detail in 1995 . Unlike proliferating tricholemmal cysts, proliferating epidermoid cysts are observed more commonly in men and only 20% occur on the scalp. They range in size from 0.4 to 15 cm. In the 30 patients reported by Sau et al. for whom follow-up was available, 20% of the cysts recurred, some multiple times, and one patient died of intractable local disease. None of the patients developed metastatic disease.
Histologically, almost half of cases show an epidermal connection, usually with a narrow opening or connection to a dilated follicle. Most tumors show areas of typical epidermoid cyst wall. In addition, areas of squamous proliferation with squamous eddy formation are seen, with formation of a granular layer and production of loose laminated keratin. The epithelium tends to proliferate peripherally into the surrounding dermis, rather than centrally as seen in proliferating tricholemmal cysts. Degrees of cellularity and atypia are variable, and frank carcinomatous change with an infiltrative growth pattern may be seen.
Treatment is by complete surgical excision.
Vellus hair cysts, described by Esterly, Fretzin and Pinkus in 1977 , most commonly present as numerous, small, dome-shaped papules, ranging from skin-colored to darkly pigmented ( Fig. 110.11 ). These cysts are most commonly located on the trunk, and they may be inherited in an autosomal dominant pattern. Multiple lesions are known as “eruptive” vellus hair cysts; occasionally, solitary cysts are seen. Although some lesions may resolve via transepidermal elimination of cyst products, most lesions persist indefinitely. Vellus hair cysts may become inflamed, but in general, they are asymptomatic except for cosmetic concerns.

Eruptive vellus hair cysts may be seen in conjunction with steatocystoma multiplex, and both types of cysts have been reported in the setting of pachyonychia congenita (most frequently PC-17; see Ch. 58 ). Since steatocystomas arise from the sebaceous duct and vellus hair cysts arise from the infundibulum, overlapping features may occur when there is cyst formation at the junction of the sebaceous duct and follicular epithelium.
Histologically, one sees a small cystic structure lined by stratified squamous epithelium with epidermoid (infundibular) keratinization. The cysts contain loose laminated keratin and numerous vellus hairs( Fig. 110.12 ). A follicle may be found entering the lower portion of the cyst.
Visualization of the vellus hairs via microscopic examination of expressed cyst contents allows for a bedside diagnosis.
Vellus hair cysts may be treated by a number of modalities, including incision and drainage, needle evacuation, puncture followed by forceps-assisted extraction, topical retinoic or lactic acid, and laser ablation.
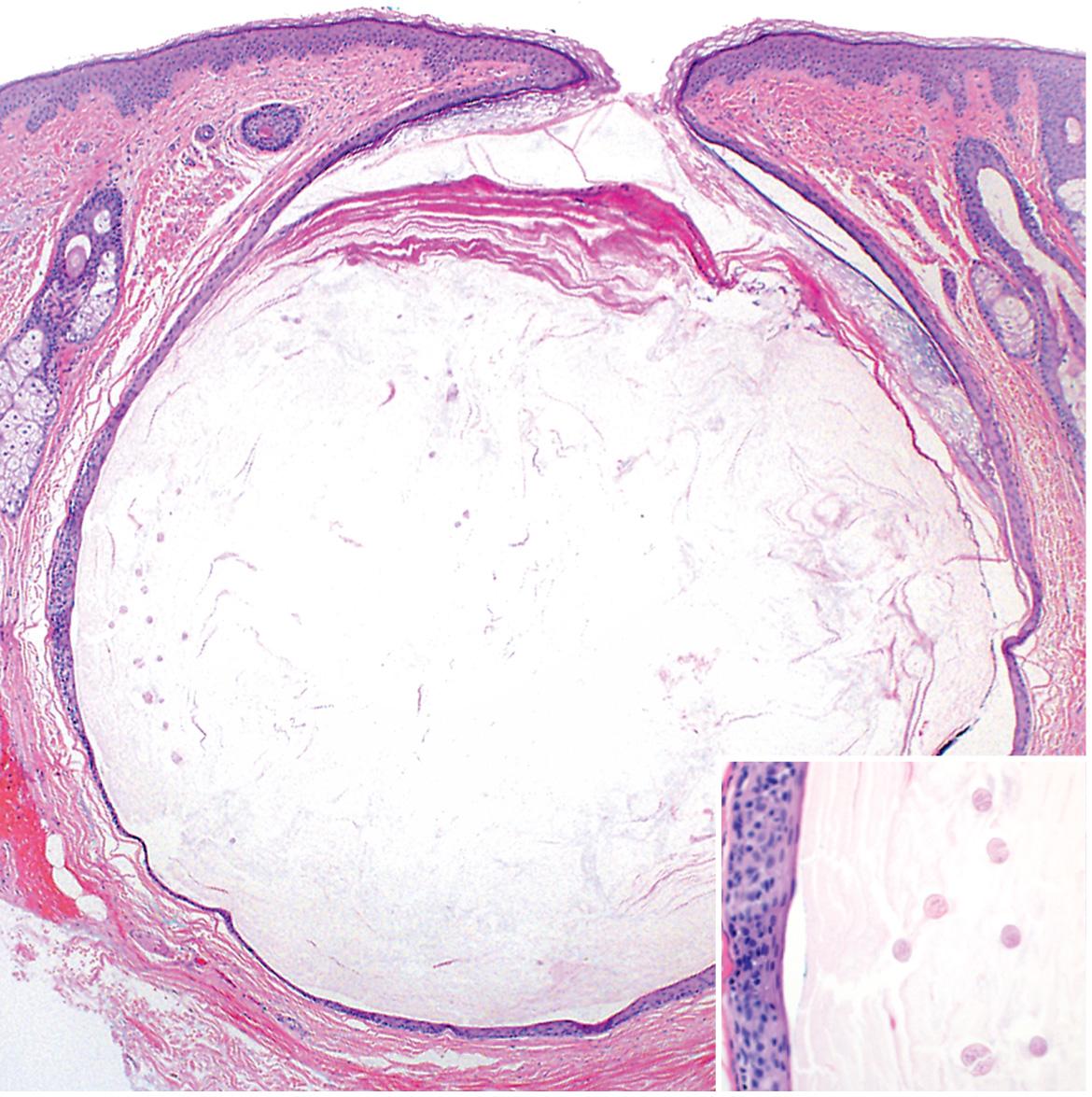
Steatocystomas occur as single (steatocystoma simplex) or multiple (steatocystoma multiplex) lesions. They tend to be a few millimeters to a centimeter in diameter and appear as cysts within the dermis that drain oily fluid if punctured ( Fig. 110.13A,B ). Steatocystomas are most numerous on the chest and in the axillae and groin. There are unusual facial and acral variants as well as a rare congenital linear form. Steatocystomas persist indefinitely, and they are usually asymptomatic except for cosmetic concerns.

Steatocystoma multiplex can be inherited as an autosomal dominant condition, and is due to mutations in the KRT17 gene. It may occur in association with eruptive vellus hair cysts and pachyonychia congenita, most frequently PC-17 (see Fig. 58.11 ) .
Biopsy specimens show a dermal cyst lined by a thin stratified squamous epithelium without a granular layer. The epithelium is surmounted by a thin, irregular, corrugated eosinophilic cuticle( Fig. 110.13C ). Small sebaceous lobules are found in or immediately adjacent to the cyst wall. Cysts with the typical corrugated eosinophilic lining of steatocystoma, but with no adjacent sebaceous glands, have been termed cutaneous keratocyst or sebaceous duct cyst.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here