Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cystic lesions of bone comprise a diverse number of entities, including simple or unicameral bone cyst, aneurysmal bone cyst (ABC), epidermal cyst, and intraosseous ganglion. Simple bone cysts are typically lesions of boys in the long bones and are relatively easy to recognize on conventional imaging and histopathology. They are treated with a combination of curettage, bone grafting, and injection of steroids into the luminal cavity. In contrast, ABCs have a broader age range and affect the sexes equally. Although they also often occur in the metaphysis of long bones, the posterior elements of the spine are also a common site. Radiologically, the presence of internal septation with fluid–fluid levels is a key finding. Histologically, key features include the identification of blood-filled cystic cavities lacking endothelial linings and the presence of fiber osteoid embedded within the walls. Solid forms exist. Separating primary from secondary ABCs is critical and is typically accomplished with the help of molecular genetics identifying a CDH11/USP6 chimeric gene. Epidermal or keratinous cysts occur most commonly on the terminal phalanx or skull as painful masses in middle-aged men. They histologically mimic epidermal cysts found in soft tissue and skin and, although they may generate a large differential diagnosis radiologically, they are easily recognized histologically. Curettage is curative. Lastly, intraosseous ganglia are typically found in a subchondral location adjacent to a knee or hip joint in middle-aged patients. Radiologically, they are oval and have a prominent sclerotic margin. Histologically, they mimic soft tissue ganglion cysts. They, too, are usually easily treated by curettage.
An ABC is a benign cystic lesion of bone composed of multiple, blood-filled cavities separated by reactive connective tissue containing fibroblasts, osteoclast-type giant cells, and woven bone. Synonyms include multilocular hematic cyst and giant cell reparative granuloma.
The term aneurysmal bone cyst was first introduced by Jaffe and Lichenstein in 1942 in their description of solitary bone cysts. In this treatise, there are two reported cases with peculiar “blown-out” distention of the contour of the affected bone. In 1950 these researchers named this lesion aneurysmal bone cyst.
It is difficult to establish the actual incidence of primary ABCs, because many cases go unpublished. The estimated annual incidence is 0.15 per million subjects. The male-to-female ratio is approximately 1 : 1. ABCs occur at any age; however, almost 80% of the lesions are in patients younger than 20 years of age.
Almost any bone may be involved, but the region around the knee, including the distal femur and the proximal tibia, is the most common site. The spine is also frequently involved, most commonly in the cervical region. In the long tubular bones, ABCs tend to involve the metaphysis, whereas in the spine, they predominantly involve the posterior elements. About 5% of ABCs, typically the solid variant, involve the axial skeleton (i.e., the spine or innominate bone).
The presenting symptoms vary according to the affected bone. In the long bones, the most common sign is swelling, and the most common symptom is pain. In the vertebrae, an ABC can compress nerves or the spinal cord, resulting in paresthesias and numbness of the extremities.
Radiographic findings of an ABC are similar to those of a giant cell tumor of bone, enchondroma, giant cell reparative granuloma, brown tumor of hyperparathyroidism, osteoblastoma, and rarely, infection. Specifically, the radiographic findings are usually typical and easily diagnosed on conventional radiographs. The main radiographic findings are osteolysis and ballooned osseous expansion. In tubular bones, ABCs show eccentric and osteolytic lesions with or without a well-defined margin. Sclerosis can also be present. Sometimes, ABCs have a soap-bubble appearance. When ABCs show expansion of the cortical surface, they may be mistaken as being malignant due to the loss of cortical margin as well as the extension into the soft tissue. In short tubular bones, ABCs are located closer to the central portion and undergo symmetric expansion of the metaphysis. The typical site of spinal involvement is in the posterior elements, and the lesion is similar in appearance to that arising from tubular bones.
On magnetic resonance imaging (MRI), ABCs show heterogeneous signal intensity. They show internal septation with fluid–fluid levels that are seen as a high signal on both T1- and T2-weighted images due to uncoagulated blood.
The lesions are frequently curetted, and red-brown, granular, fragmented materials are received. If the lesion is resected, the cut surface shows characteristic hemorrhagic, multilocular, cystic spaces filled with blood, separated by fibrous septa of different thicknesses. More solid areas can also be found.
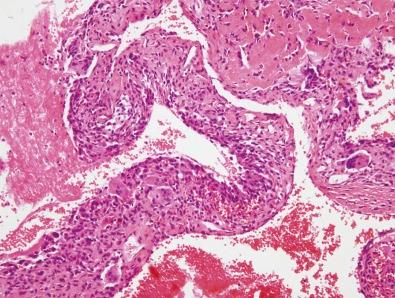
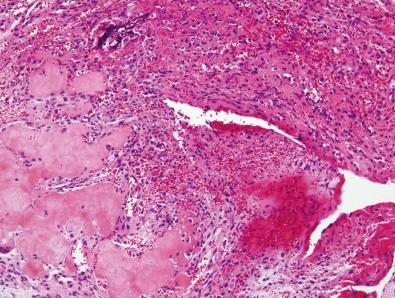
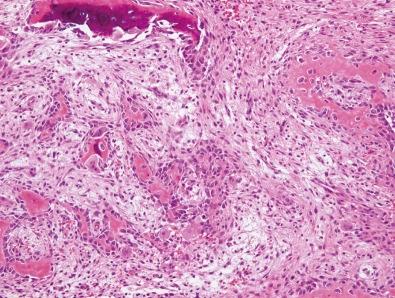
On low-power examination, the characteristic histologic feature is multiple blood-filled cavities of varying sizes ( Fig. 15-1 ). The cystic walls lack an endothelial lining and consist of spindle cells, giant cells, capillaries, and varying amounts of matrix. The stromal cells sometimes show abundant mitotic figures; however, the stromal cells are uniform, and atypical mitoses are lacking. Osteoid and bony matrix may be prominent ( Fig. 15-2 ). Often, a thin layer of osteoid (so-called fiber osteoid) is found in the septa. The reactive woven bone, rimmed by osteoblasts, is found in these septa ( Fig. 15-3 ). In approximately one half of cases, the bone is basophilic and termed blue bone . Sometimes a peculiar calcification called a chondroid aura is present. This is not seen in any other bone lesions. Necrosis is rare unless there is a pathologic fracture. The solid portions may be predominantly fibrous and present a lacework of osteoid or newly formed bony trabeculae. The bony trabeculae tend to anastomose and to have prominent osteoblastic rimming.
The term secondary ABC is applied to ABCs that are superimposed on preexisting conditions. Neoplasms most frequently encountered with ABCs are chondroblastoma, giant cell tumor of bone, chondromyxoid fibroma, and fibrous dysplasia. However, ABC-like changes are also found in association with various malignant tumors such as osteosarcoma and metastatic prostate carcinoma. The prognosis and behavior mirror those of the underlying condition.
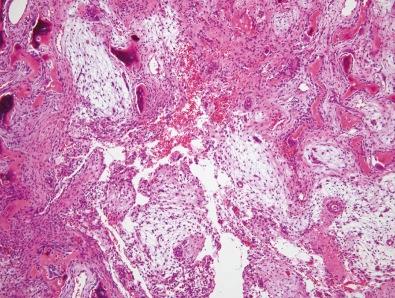
The term solid variant of ABC was first introduced by Sanerkin et al. in 1983. This variant has the same components as the septa of conventional ABC and is also identical to the histology of giant cell reparative granuloma. Histologically, the lesion shows a spindle cell proliferation with a loose arrangement of embedded cells. Also found is abundant reactive new bone formation with prominent osteoblastic activity ( Fig. 15-4 ).
Primary aneurysmal bone cysts may be confused with giant cell tumors, low-grade osteosarcomas, and telangiectatic osteosarcomas. Before a diagnosis of primary ABC is made, every effort must be made to rule out an underlying condition to confirm that the lesion is not a secondary ABC. Less frequently, large numbers of giant cells may be present similar to a giant cell tumor of bone. However, giant cell tumors occur in skeletally mature patients and typically involve the ends of bones, whereas ABCs occur in skeletally immature individuals and are metaphyseal in location. Low-grade osteosarcomas are much less cellular and show greater mitotic activity than conventional ABCs.
The most difficult problem is to differentiate an ABC from a telangiectatic osteosarcoma. Histologically, the septa in telangiectatic osteosarcoma are composed of very pleomorphic anaplastic cells, whereas those in ABC reveal no cytologic atypia.
Panoutsakopoulos and colleagues reported three cases with clonal chromosomal aberrations, two with a t(16;17)(q22;p13) translocation and one with a del(16)(q22) deletion, providing support for a clonal basis for this lesion. This was followed by several other studies suggesting that a rearrangement of the chromosome band 17p13 was the characteristic genetic feature of an ABC, with t(16;17)(q22;p13) being the most frequently observed chromosomal aberration. This t(16;17) translocation generates a fusion gene in which the strong promoter of the osteoblast cadherin 11 gene ( CDH11 ) at 16q22 is fused to the entire ubiquitin-specific protease 6 ( USP6 ; also known as Tre2 ) coding sequence at 17p13. The result is a CDH11/USP6 chimeric gene that is transcriptionally up-regulated.
The fusion genes of the variant translocations t(1;17)(p34;p13), t(3;17)(q21;p13), t(9;17)(q22;p13), and t(17;17)(q12;p13) have been reported in ABCs. In each translocation, the entire USP6 coding sequence is subsequently fused downstream to the promoter region of the partner gene: THRAP3 (also known as TRAP150 ) at 1p34, CNBP (previously ZNF9 ) at 3q21, osteomodulin ( OMD ) at 9q22, and collagen 1A1 ( COL1A1 ) at 17q21. In a series of 18 ABCs, only a single case of these chimeras was detected. USP6 and CDH11 oncogenes have been identified only in primary ABCs and are absent in secondary ABCs. In solid variant ABCs, a novel (X;9) translocation has also been reported.
The preferred treatment is surgical removal of the entire lesion and if possible, bone grafting of the resulting defect. Prognosis in ABCs is excellent. In extremely rare cases, ABCs have been reported to have healed spontaneously. Recurrence is typical within 6 months, and reoperation results in a complete cure. Malignant transformation has been reported by Kyriakos and Hardy, but such incidents are extremely rare.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here