Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Several treatment options exist for the management of massive acetabular bone loss encountered during acetabular component revision. These include column plating in conjunction with porous metal shells, structural allografts, impaction grafting, distraction technique with jumbo porous metal acetabular components with or without porous metal augments, acetabular reconstruction cages, cup-cage constructs, and custom triflange acetabular components (CTACs). However, in the setting of massive bone loss with chronic pelvic discontinuity, the success of each of these treatment options varies significantly. Challenges faced include loss of fixation and aseptic failure, implant fatigue failure, prosthetic hip instability, and structural allograft resorption. CTACs were developed as a potential solution for massive acetabular bone defects, with the goal of overcoming some of these challenges. Premise: CTACs are designed to span areas of massive acetabular bone loss and pelvic discontinuity, allowing for potential osseointegration in areas of contact with host bone and potential healing of a chronic pelvic discontinuity over time. Furthermore, the implants are designed to resist fatigue failure, which is not uncommon with non-custom stand-alone reconstruction cages.
Following a complete and thorough history and physical exam, an initial plain film evaluation must be performed to identify a possible pelvic discontinuity in the setting of acetabular component revision. This is comprised of an anteroposterior (AP) view of the pelvis, along with Judet iliac and obturator oblique views to assess the posterior and anterior columns, respectively. These views are useful in the radiographic assessment of existing cup stability, and the extent of osteolysis, pelvic bone loss, and the likelihood of pelvic discontinuity ( Fig. 19.1 ).
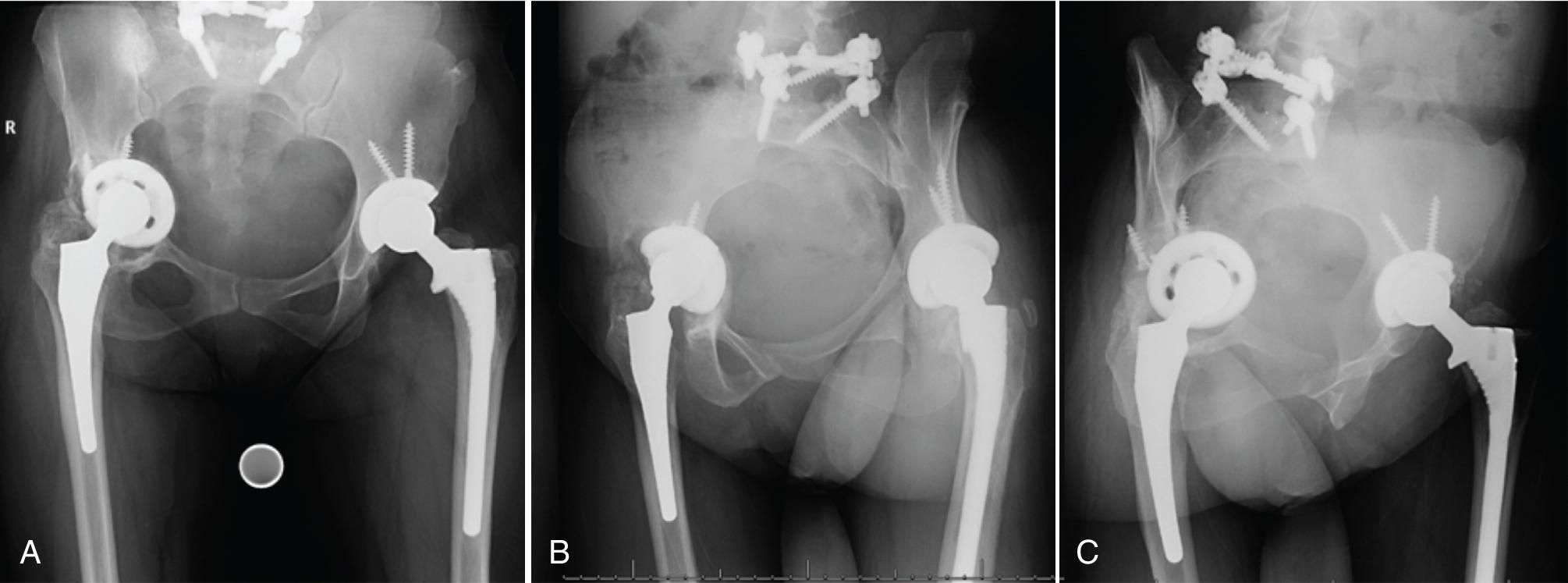
Thin-cut (2-mm) pelvic computed tomography (CT) imaging with 3D image reconstruction is a valuable tool and a requisite for the workup of a suspected pelvic discontinuity on plain films ( Fig. 19.2 ). CT imaging, often enhanced by metal-subtraction, minimizes intraoperative surprises with more accurate quantification of the extent of bone loss and severity of associated osteolysis and effectively guides intraoperative surgical dissection and planning. In cases with a significant breach of Köhler’s line and medial migration of the existing acetabular component, it is important to consider obtaining CT angiography for mapping of the proximity of the iliac vessels to the acetabular component. This is critical in guiding vascular surgery consultation and avoiding the potential for catastrophic vascular injury during acetabular component removal.
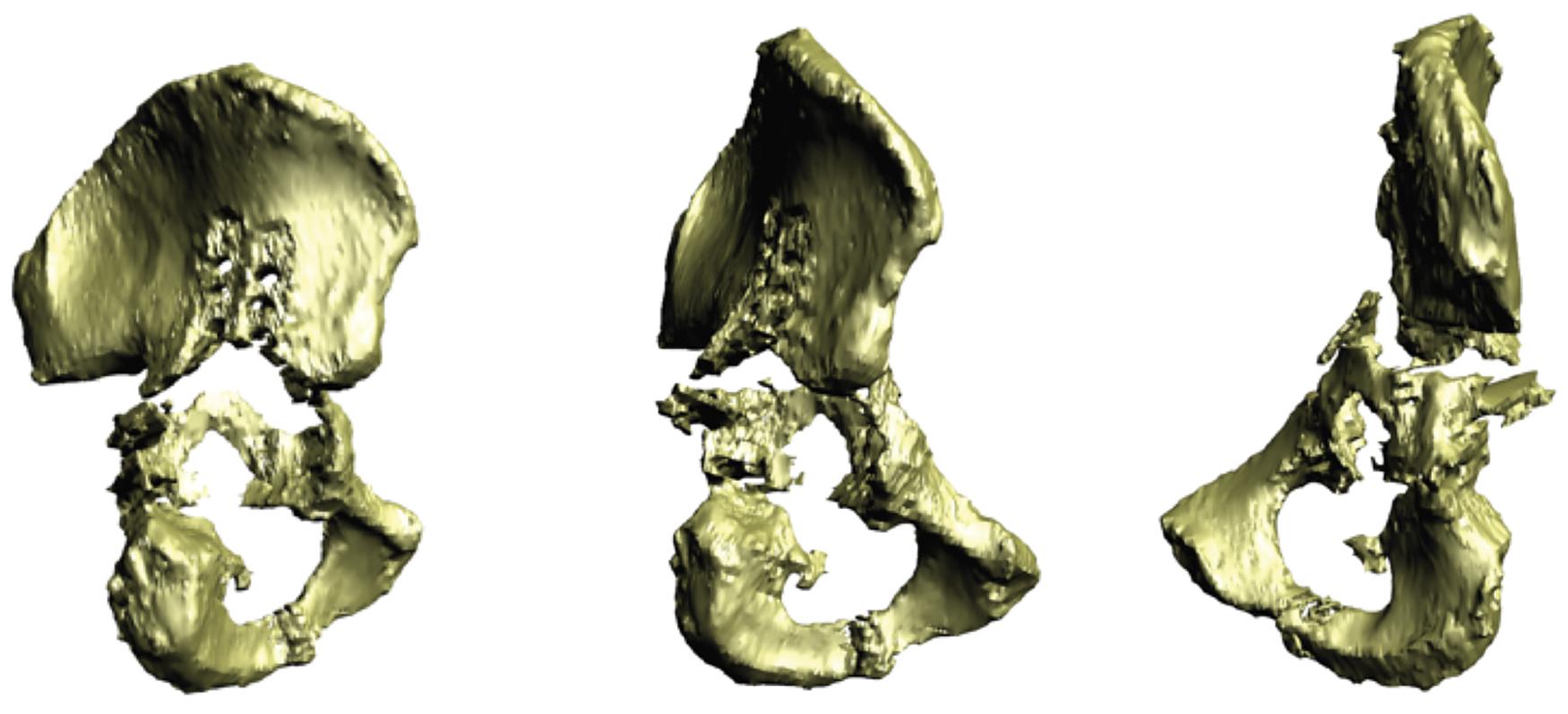
In cases of severe acetabular bone loss with or without an associated chronic pelvic discontinuity, CT imaging can be used with modeling software to develop an accurate acrylic model of the hemipelvis. This allows assessment of the degree of bone loss to determine whether the defect could be managed with conventional implants or the need for a triflanged implant. Once the need for a custom implant has been made based on the evaluation of the acrylic model, implant manufacturing engineers are engaged to develop a CTAC implant ( Fig. 19.3 ). This allows the surgeon to collaborate with the engineers to optimize cup abduction and anteversion orientation, hip center position, liner options, and the number, length, and trajectory of flange screws. Critical aspects of design that must be addressed by the surgeon include assessment of an adequate number of ischial screws and ensuring that the iliac flange is not in close proximity to the sciatic notch . This limits the risk of injury to the superior gluteal neurovascular bundle. Additionally, the length of the iliac flange should be minimized to avoid stretching of the superior gluteal nerve during implant and screw insertion, ensuring that the iliac flange and screws have purchase in robust, residual iliac bone . Directin g the iliac screws superiorly helps accomplish these goals. If retaining the femoral component, the surgeon must estimate the ability to reduce a proximally migrated femoral head into a triflange implant that recreates the normal hip center . If this is felt to be impossible, adjustments in the CTAC center of rotation must be made. Communication with the designing engineers is critical during this process as it is not unusual to redesign the trial model multiple times before final approval and manufacturing of the CTAC implant.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here