Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Patients with craniofacial microsomia (CFM) require the care of a skilled multidisciplinary clinical team.
Phenotypic features of CFM are highly variable. While the three structures most affected include the ear, mandible, and maxilla, abnormal development can occur in any of the derivatives of the first or second branchial arches.
Clinical evaluation of patients with CFM must include assessment for obstructive sleep apnea (OSA) symptoms, particularly in bilateral cases.
Distraction osteogenesis (DO) of the mandible can be considered in neonates and infants with CFM who exhibit severe respiratory compromise and who may otherwise require a tracheostomy.
Vectors of mandible distraction (vertical, oblique, or horizontal) should be planned according to treatment goals.
In cases of severe mandibular hypoplasia, staged procedures with grafting (non-vascularized or vascularized bone) should be performed, often followed by DO.
If two-jaw surgery is to be performed for CFM, a two-splint (intermediate splint) technique is used and the technique is usually deferred until skeletal maturity.
Orthodontic monitoring is important throughout the years of growth and development. Interventions are especially important during and after the distraction process to prevent undesired movements (i.e., anterior open bite, lateral shift) and in the period surrounding two-jaw surgery.
Craniofacial microsomia (CFM) involves a spectrum of congenital malformations of craniofacial structures that arise from the first and second branchial arches. These include the mandible, maxilla, external and internal ear, orbit, temporal bone, facial soft tissue, and muscles, and the facial nerve. These malformations result in differences in facial aesthetic appearance and various functional difficulties with feeding, hearing, airway anatomy, facial expression, speech, and globe protection. Given the broad phenotypic spectrum of severity ( Fig. 26.1 ), patients with CFM should be cared for by a multidisciplinary craniofacial team consisting of craniofacial plastic surgeons, microsurgeons, otolaryngologists, ophthalmologists, pediatricians, orthodontists, feeding specialists, psychologists, speech therapists, and craniofacial nurses.

Craniofacial microsomia represents one of the most common congenital malformations of the head and neck, second only to cleft lip and palate. CFM has an incidence estimated from 1 : 642 to 1 : 26 000. The majority of CFM cases occur in a sporadic fashion; however, the presence of CFM in successive generations may suggest the presence of various modes of genetic inheritance.
Historically, CFM was thought to primarily involve one side of the face with bilateral involvement noted in 5%–30%. However, upon closer inspection patients diagnosed with unilateral involvement often have more subtle abnormalities on the contralateral side. The greater appreciation of contralateral subtle findings may correspond to a higher ratio of bilateral involvement in more recent reviews. Although many studies have demonstrated a right-sided and male predominance, others have found equivalent right/left and gender distributions. For instance, Grabb reported a male predominance, with a male-to-female ratio of 63 : 39, and Rollnick et al. reported a similar ratio of 191 : 103. The clinical series of Horgan et al . reported an equal sex ratio of 59 males to 62 females.
The first branchial arch (mandibular arch) gives rise to the maxilla, mandible, zygoma, trigeminal nerve, muscles of mastication, connective tissue of the face, and a minority of the external ear (tragus, root of helix, superior portion of the helix). The second branchial arch (hyoid arch) gives rise to the stapes, styloid process, portions of hyoid bone, facial nerve, facial musculature, and most of the external ear (inferior portion helix, antihelix, antitragus, and lobule).
During the first trimester all branchial arches have their own artery arising from the aortic arch. The first aortic branch supplies the first branchial arch and the second supplies the second branchial arch. In the third week of gestation, the internal and external carotid arteries develop from the third branchial arch, while the first and second aortic arch become less necessary. The remnant of the second aortic arch is the stapedial artery, which forms the anastomosis between the internal and external carotid arteries in the fourth week of gestation. During this week the stapedial is the main blood supply for the first and second branchial arches. In the fifth week the stapedial artery atrophies and disappears and around day 40 of gestation the external carotid artery supplies the blood for the first and second branchial arches.
The etiology of CFM remains unclear but is probably heterogeneous among individuals, with variable contributions from extrinsic and intrinsic factors. It has been thought primarily to be associated with vascular perturbation, teratogen exposure, neural crestopathy, or a combination of the three.
The first hypothesis raised involves a vascular disruption in the development of the first and second branchial arches during the first 6 weeks of gestation. Poswillo reproduced in mice some of the phenotypic anomalies seen in CFM phenotype by administering teratogens (triazine) that caused a hematoma of the stapedial artery and resulted in local and regional necrosis ( Fig. 26.2 ). The wide spectrum of resulting facial anomalies was felt to be caused by the vascular injury, the resulting tissue necrosis, and its inability to regenerate. Although a “stapedial artery hemorrhage etiology” is attractive because the vessel is a second branchial arch derivative, a causative association between the bleeding and the deformities has not been made. The hemorrhages occurred 14 days after administration of the teratogen, and there was no clear temporal relationship between the hemorrhage appearance and the associated phenotypic deformity. When mice are exposed to triazine later in development (10 days of gestation), all animals developed deformities; however, only a third showed evidence of a hematoma. The authors concluded that triazine has a direct teratogenic effect and the stapedial artery findings were simply a side effect. In contrast to those described by Poswillo, these animals demonstrated more evidence of bilateral deformities and inner-ear anomalies. Moreover, rats exposed to etretinate, a retinoic acid derivative, show deformities comparable to the first and second branchial arch syndromes. This finding is consistent with the finding that neural crest cells express large amounts of retinoic acid-binding proteins. Furthermore, when retinoic acid is administered early in development, it interferes with cell migration. When administered later in gestation, however, retinoic acid kills ganglionic placodal cells, resulting in a deformity similar to mandibulofacial dysostosis (Treacher Collins).
On the other hand, intermittent occlusion of the internal carotid system of fetal sheep late in gestation has been shown to result in deformities similar in appearance to CFM. The vascular disruption hypothesis, therefore, cannot be excluded.
To evaluate associations between the individual deformities associated with CFM in a large cohort of patients, Tuin et al . 's study revealed significant associations between deformities of the orbit, mandible, and soft tissue. Nerve involvement and ear deformity were significantly associated as well as nerve involvement and soft-tissue deficiency. A higher degree of deformity of the individual OMENS (Orbital Mandible Ear Nerve Soft tissue – see later) components demonstrated in the mandible, orbit, and soft tissue on the ipsilateral side were associated with the presence of macrostomia. Thus, they hypothesized that the embryologic origin of the structures involved in CFM could explain the findings in this study. The degree of deformity of the different structures derived from the first branchial arch are significantly associated. These first arch abnormalities include orbital deformity (since the lower orbital rim is formed by the zygoma and maxilla), mandibular deformity, and macrostomia, resulting from the incomplete fusion of the mandibular and maxillary process of the first branchial arch. However, the facial nerve and most of the ear (85%) develop from the second branchial arch. Their findings demonstrate that these structures, mainly derived from the second branchial arch, are also significantly associated. Additionally, the degree of facial nerve involvement as well as the severity of the ear deformity are also correlated.
Studies have suggested a fundamental role for genetic transmission in some patients. Autosomal dominant and recessive transmission patterns have been described in families with features of CFM, and a positive family history of 50% has been observed in a large series of cases. This etiologic heterogeneity, along with variability in penetrance and expression, could account for the wide phenotypic spectrum seen in CFM. Recently, studies in mice showed inactivation or the allelic reduction of Edn1 , Ednra , Dlx5 , Dlx6 , Gsc , Pitx1 , and Gbx2 , all of which result in a proximal defect of the developing mandible or of the middle and external ear, which is also characteristic of CFM. Support of a genetic etiology of CFM has come from both animal and human studies. A transgenic mouse model for CFM with an insertional deletion on mouse chromosome 10 has been described with an autosomal-dominant mode of transmission and 25% penetration. The affected animals display low-set ears, unilateral microtia, and jaw asymmetry, without evidence of middle-ear abnormality.
Various human genetic studies have documented a positive family history in 9.4% of 32 probands, 21% of 57 probands, 26% of 88 probands, and 44% of 82 probands. Kaye et al . performed segregation analysis on 74 families of probands with CFM and rejected the hypothesis that genetic transmission is not a causative factor. The evidence favored autosomal dominant inheritance; however, recessive and polygenic models were not distinguishable. Despite the suggestion of autosomal dominant transmission, they found only a 2%–3% overall recurrence rate in first-degree relatives. This figure compares to the 10% recurrence risk in first- and second-degree relatives reported by the same group in an earlier study of 294 individuals with CFM.
Studies on the incidence and expression of craniofacial anomalies in twins have provided insight into the etiology of CFM. Werler et al . described 10 twin pairs with CFM. Only one of the pairs, who were monozygotic, was concordant for the anomaly. Other twin studies have noted a high level of discordance of CFM among monozygotic twins. Further confounding the issue, recent multicenter research studies have found non-craniofacial anomalies such as vertebral, cardiac, and renal in 35% of patients with CFM, indicating involvement of tissues outside of the first and second branchial arch.
To summarize, the exact etiology of CFM is still a matter of debate. This clearly heterogeneous entity is likely to involve multiple factors, including genetic anomalies with various intrinsic modifiers to extrinsic insults such as teratogens or vascular events.
Since its earliest descriptions by Canton and Von Arlt in 1861 and 1881, respectively, a variety of terms have been applied to this anomaly. These include craniofacial microsomia, hemifacial microsomia, first and second branchial arch syndrome, otomandibular dysostosis, auriculobranchiogenic dysplasia, intrauterine facial necrosis, lateral facial dysplasia, hemignathia and microtia syndrome, necrotic facial dysplasia, otomandibular-facial dysmorphogenesis, mandibular laterognathism, oculoauriculovertebral spectrum, and facioauriculovertebral malformation complex. This extensive list attests to the difficulty of satisfactorily labeling the breadth of malformations defining this syndrome. Indeed, as Longacre et al . noted: “The prominent feature of these dysplasias is their variability.”
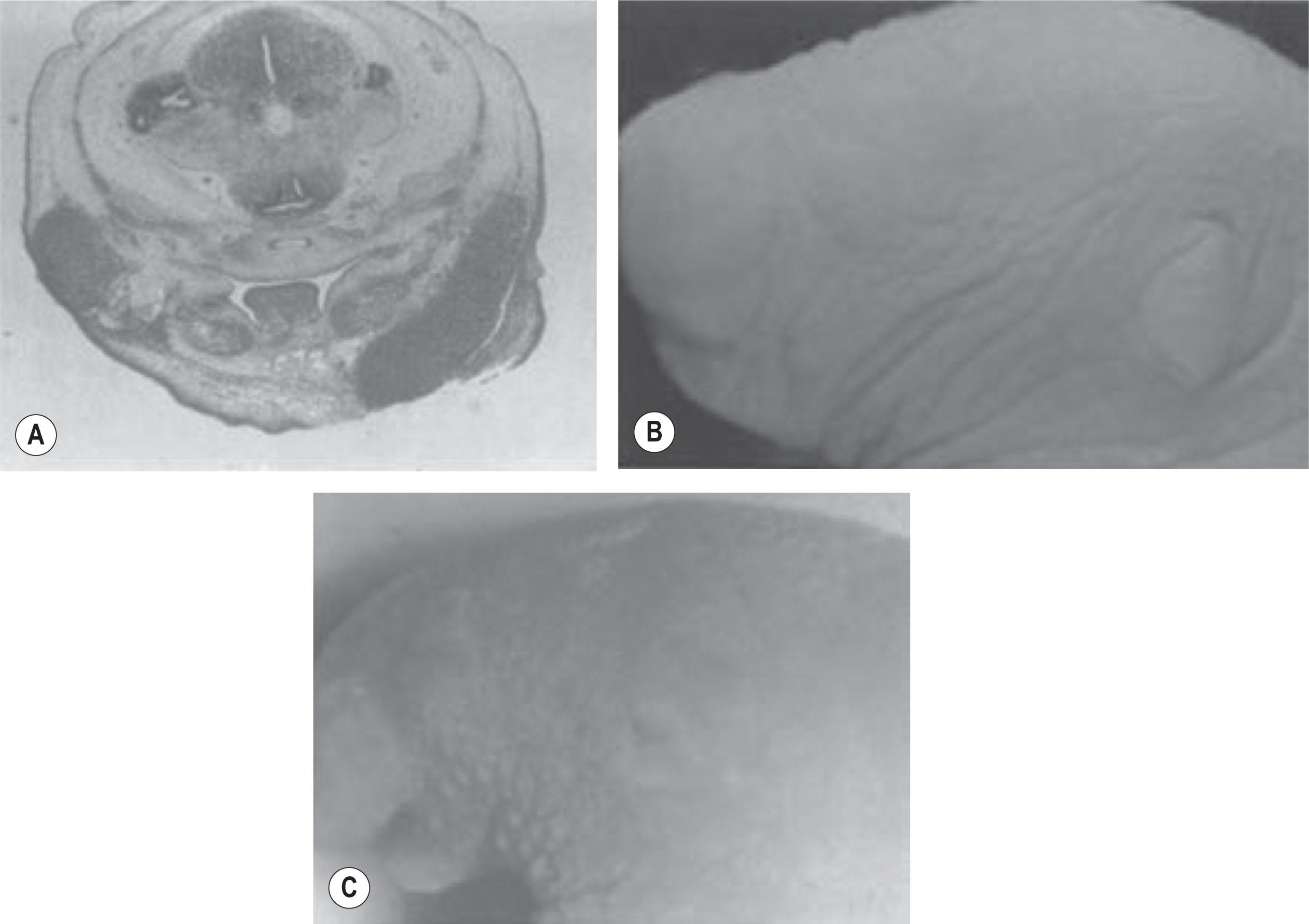
Variable abnormalities of the ipsilateral zygomatico-orbital region are common. The orbit can be small and/or can have an abnormal position which can lead to orbital dystopia (see Fig. 26.1A ). Moreover, periocular abnormalities may range from mild inferior displacement of the lateral canthus and/or palpebral fissure to microphthalmia/anophthalmia ( Fig. 26.1B ). In some instances, colobomas of the iris or upper lid with absence of the eyelashes may also be noted, as can epibulbar dermoids.
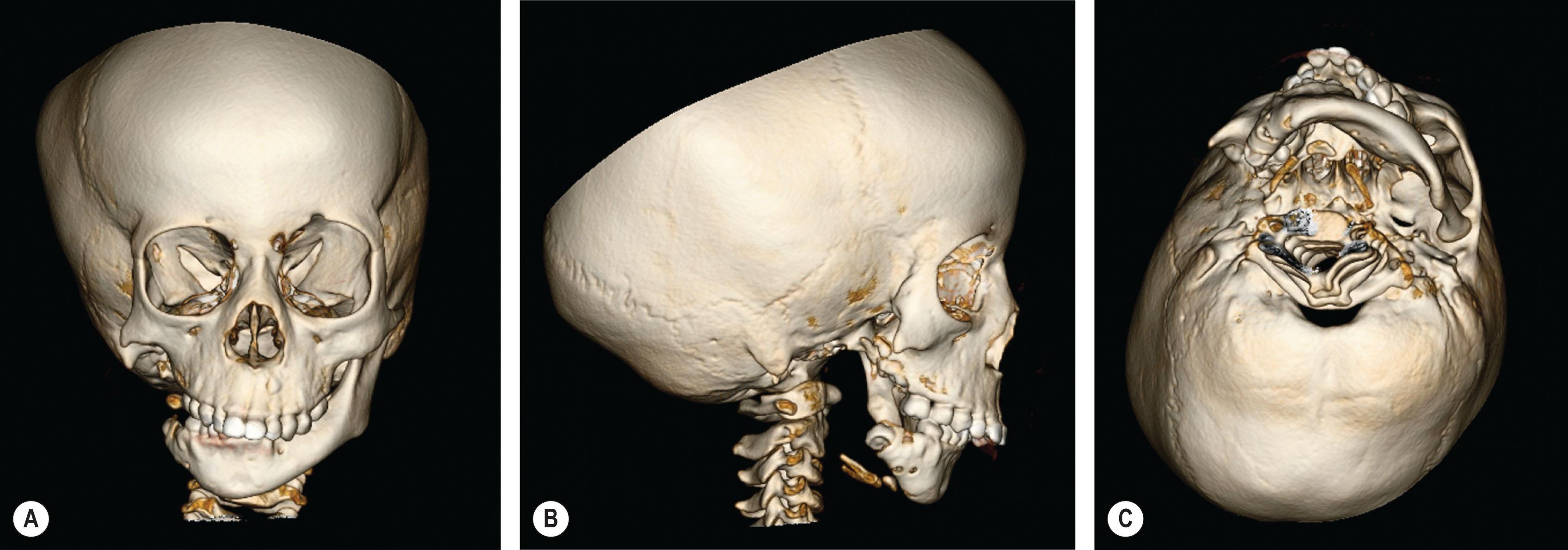
The mandible has long been considered the “cornerstone” of craniofacial microsomia and is generally involved to some degree. Mandibular hypoplasia may range from mild hypoplasia of the condylar head to complete agenesis of the condyle, ramus, and glenoid fossa ( Fig. 26.3 ). A wide array of temporomandibular joint abnormalities results from the variable mandibular hypoplasia, leading to deformities from mild malpositioning with aberrant cranial base articulation to complete obliteration. The mandibular body may also be reduced in all dimensions, frequently with an increase in the size of the gonial angle. Steinbacher et al . sought to volumetrically evaluate and characterize the mandible in CFM compared with controls, and to assess for Pruzansky score correlation. As expected, with increasing Pruzansky severity, hemi-mandibular and proximal segment volumes declined. The hemifacial dentate segment also proved significantly diminished, corresponding to the degree of proximal volume loss. Recent research has demonstrated a high rate of dental anomalies in patients with CFM.
Historically, it was believed that the mandibular deformity was associated with a maxillary hypoplasia. It was accepted that the maxillary hypoplasia in combination with mandibular deficiency frequently results in dental malocclusion and, depending on the severity of the maxillomandibular deficiency, an upward occlusal cant to the affected side. Wink et al . shed new light on the maxillary deformity in CFM by evaluating volumetric differences and linear measurements in the “affected” side vs. the “unaffected” side, finding little or no relationship between the mandibular and maxillary deformity. The results demonstrated an absence of any notable midface bone and sinus volume loss in patients with CFM and analyses of the maxillary segmentation models also showed no statistically significant differences between the mean values for maxillary width, depth, and height within all severity groups.
These findings suggest that the maxillary anomaly is not a true volumetric deficiency. The maxillary cant observed is more likely secondary to vertical growth inhibition by the pathologically small mandible.
Those findings were confirmed by Song et al ., who demonstrated that the occlusal disharmony is due to an anomaly of the alveolus and teeth, with no differences noted between the affected and unaffected sides with regards to maxillary shape and volume.
It is not surprising that auricular and/or preauricular malformations are frequent features of CFM since portions of the external/middle ear and mandible share a common embryologic origin. Auricular malformations seen in CFM are as diverse as those demonstrated by the syndrome's other component features. The ear anomalies associated with CFM can be categorized into external ear malformations (e.g., microtia), middle ear malformations and atresia, and the presence of branchial remnants and sinus tracts. Although the presence of branchial remnants in isolation is generally not considered part of the CFM spectrum, the existence of isolated microtia is often considered a component of CFM as the risk factors and affected tissues are similar.
Hypoplasia of the external ear can range from mild effacement of auricular architecture to complete auricular agenesis and external auditory canal atresia. In severe cases, the only observable evidence of external ear development is represented by a primitive auricular remnant and located caudally and ventrally ( Fig. 26.4 ), while in very rare instances, no remnant is observable. Variable hypoplasia of middle ear structures is also a common feature. External and middle ear dysplasia may result in hearing loss, predominantly conductive in nature, in up to 75% of patients. The severity of the external ear deformity may predict the degree of middle ear involvement.

A wide variety of cerebral anomalies exist in CFM and may include ipsilateral cerebral hypoplasia, hypoplasia of the corpus callosum, hydrocephalus of the communicating type and obstructive type, intracranial lipoma, and hypoplasia and malformation of the brain stem and cerebellum. Other associated abnormalities include cognitive delay, epilepsy, and encephalographic findings suggestive of epilepsy.
The most common cranial nerve anomaly is facial paralysis secondary to agenesis of the facial nerve in the temporal bone or hypoplasia of the intracranial portion of the facial nerve and facial nucleus in the brainstem. The facial nerve (CN 7) can be affected in craniofacial microsomia to varying degrees. Upper nerve function, lower nerve function, or total nerve function can be compromised. In rare instances, the hypoglossal nerve (CN 12) and trigeminal (CN 5) can also be affected.
Variable deficiency of facial soft tissues contributes significantly to the phenotypic spectrum of craniofacial microsomia. The deficiencies may involve the skin, subcutaneous fat, and neuromuscular tissues. It is most evident in the malar and masseteric region of the face as well as in the region of the external ear, orbit, and the temporal region (see Fig. 26.1A,B,C ). Lack of soft-tissue bulk contributes to a characteristic malar flattening and temporal hollowing that is best appreciated when viewed from a submental perspective.
Moreover, this appearance may be accentuated by hypoplasia involving the muscles of mastication including the temporalis, masseter, and medial and lateral pterygoids, leading also to an impairment of the masticatory muscle function on the affected side.
Macrostomia, or clefting through the oral commissure (Tessier number 7 cleft), and hypoplasia of the parotid gland may also be present. This may vary from a minor deformity ending medial to the anterior border of the masseter, to a severe cleft through all structures, and terminating in the external auditory canal.
Studies have found notable correlation between cranial base and facial asymmetry, with several authors documenting that cranial base asymmetry contributes to facial asymmetry. This association was based on the anterior and middle cranial fossae of the cranial base articulating with the face and, as such, may affect, or be affected by, alterations in facial morphology.
Paliga et al . used craniometric measurements to characterize the endocranial morphology of the anterior and middle cranial fossae in patients with CFM. The results of their study indicate that there is minimal to no deviation of the anterior cranial base angle, and absent or minor asymmetry of the endocranium in patients with CFM, implying that endocranial asymmetry is not the origin of facial dysmorphology seen in CFM.
Tongue dysmorphologies in CFM, although usually mild, are frequently overlooked. Tongue dysmorphogenesis, ranging from mild asymmetry to severe hypoplasia, may contribute to the feeding and speech difficulties encountered in this patient population. Chen et al . reported a positive correlation of the tongue, soft tissue, and mandible anomalies, pointing to a common error early in gestation or an interdependence of adjacent growth centers.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here