Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Myocardial cell contraction and relaxation are aerobic processes that require oxygen. Determinants of myocardial oxygen demands include preload, afterload, heart rate, contractility, and basal metabolic rate. Other than basal metabolic rate, these are factors that influence stroke volume. Systolic wall tension uses approximately 30% of myocardial oxygen demand. Wall tension itself is affected by intraventricular pressure, afterload, end-diastolic volume, and myocardial wall thickness.
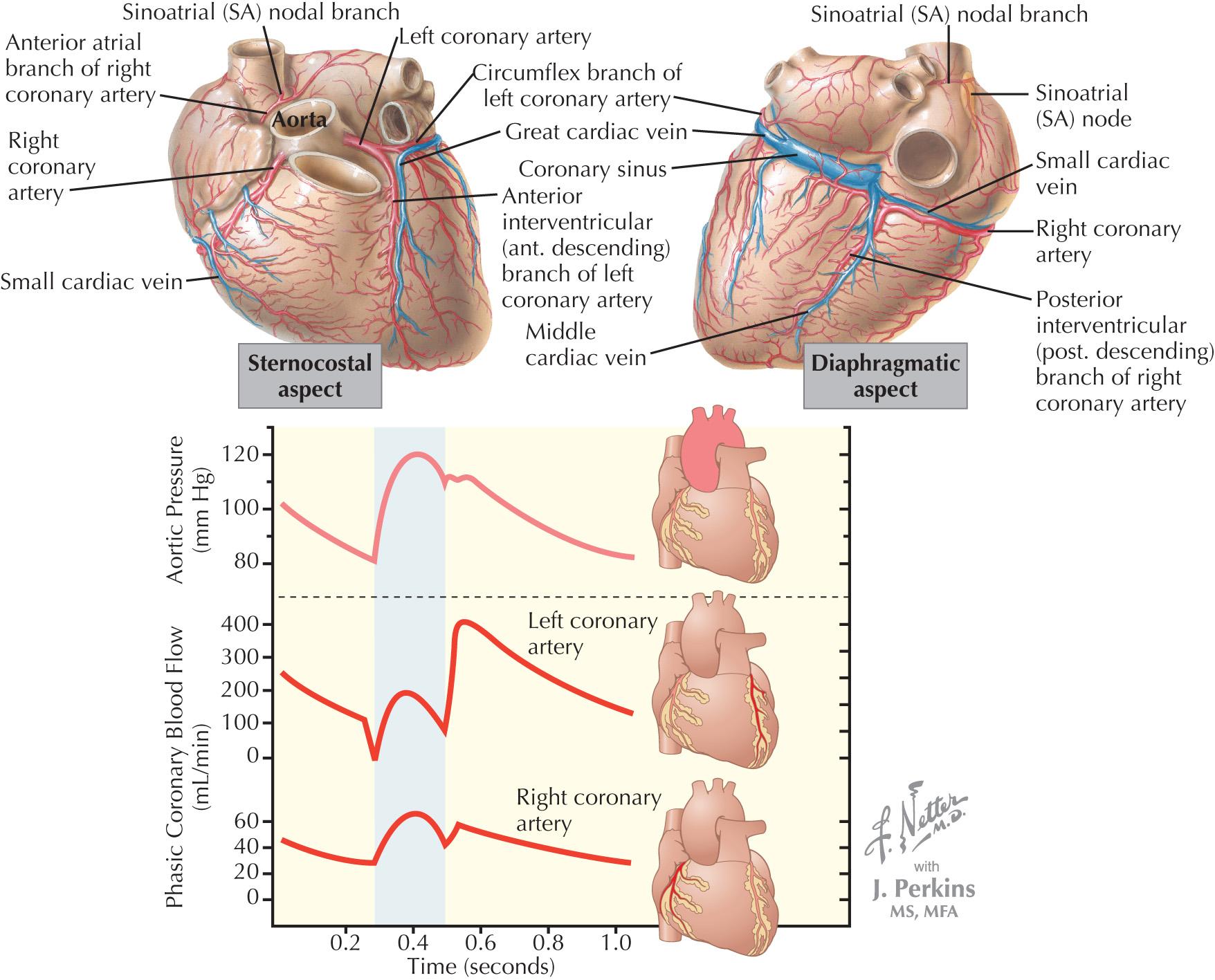
The coronary arteries are the first vessels to branch off the aorta, and through them the heart receives approximately 5% of the cardiac output when the body is at rest, or 250 mL/min. Under basal conditions, the myocardium extracts approximately 75% of delivered oxygen ( Fig. 26.1 ). The myocardium has a basal metabolic requirement that is approximately 15 to 20 times that of resting skeletal muscle and approximately equal to that of skeletal muscle under severe acidotic conditions. The heart has the highest oxygen consumption per tissue mass of all human organs and the highest arterial-venous difference in oxygen concentration of any major organ. The oxygen saturation in the coronary sinus is one of the lowest in the body.
Because there is minimal ability for the heart to increase oxygen extraction, and the heart has limited capacity for anaerobic metabolism, increased metabolic demands of the heart are met primarily via increases in coronary blood flow. In the absence of obstructive epicardial coronary artery disease (CAD), coronary blood flow is primarily controlled by changes in resistance in the small arteries and arterioles (microvasculature) that play an important role in myocardial perfusion in general and in regional and transmural distribution. The presence of hemodynamically significant epicardial disease leads to a reduction in microvascular resistance at baseline so that coronary blood flow is maintained and thus limits the ability of the myocardium to increase flow in response to increased demand.
Coronary blood flow primarily occurs during diastole. Flow in the left coronary artery has a greater diastolic predominance than the right coronary artery because the compressive forces of the right ventricle (underlying a portion of the right coronary artery) are less than those of the left ventricle ( Fig. 26.1 ). At least 85% of coronary flow in the left anterior descending artery occurs in diastole, whereas right coronary artery blood flow is more or less equal in systole and diastole. The predominance of flow during diastole exacerbates myocardial ischemia during tachycardia. With increased heart rates, oxygen supply is reduced (because diastole is shortened), whereas demand increases.
The heart has the ability to maintain coronary blood flow in the presence of varying perfusion pressures (termed autoregulation). Autoregulation maintains consistent coronary flow over a range of perfusion pressures from 60 to 150 mm Hg. In the setting of maximum vasodilation of coronary resistance vessels, coronary blood flow is no longer autoregulated and varies linearly with perfusion pressure. The ability of autoregulation to maintain flow when perfusion pressures are decreased is especially important in the presence of epicardial coronary stenoses.
The ratio of maximal coronary flow to resting coronary blood flow is termed coronary flow reserve (CFR) ( Fig. 26.2 ). Coronary blood flow is primarily controlled by release of local metabolites (e.g., adenosine or nitric oxide). Hypoxia is a more potent coronary vasodilator than either hypercapnia or acidosis. Neural influences on coronary blood flow are relatively minor. In clinical medicine, maximal coronary blood flow is achieved by intracoronary or intravenous administration of the potent microcirculation vasodilator, adenosine. Other agents that have been used to increase coronary flow include papaverine, regadenoson, nitroglycerin, and contrast dye.
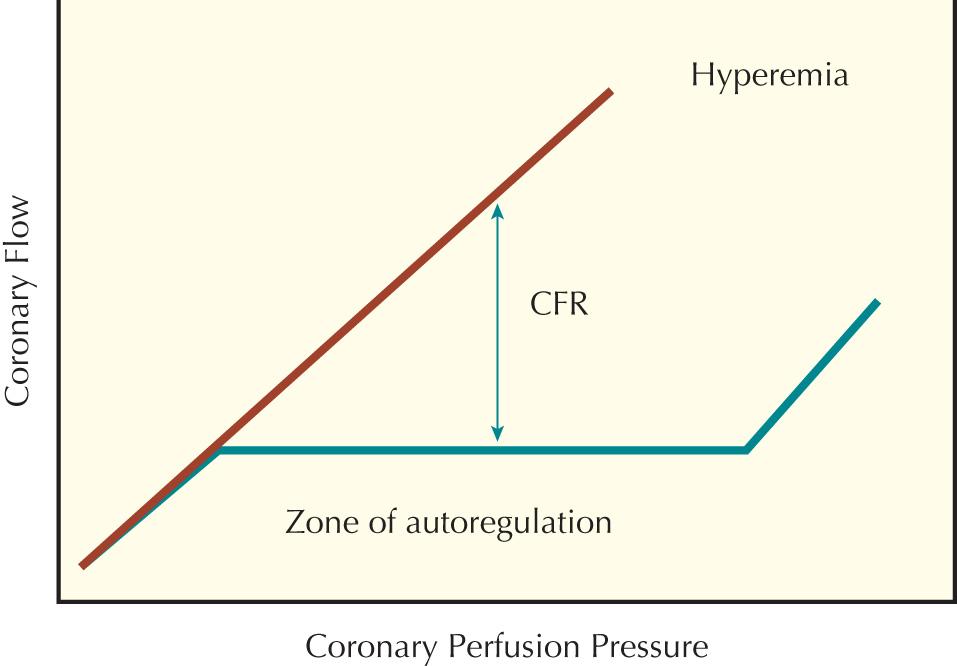
The physiological principle underlying the clinical use of CFR is that the ratio of maximal blood flow to basal blood flow will decrease with progressive obstruction of the lumen of an epicardial coronary artery by atherosclerosis. CFR can be measured using an 0.014-inch guidewire with a 12-MHz piezoelectric transducer mounted on its tip. A wire is placed in the coronary artery of interest distal to the lesion, and phasic spectral blood flow velocity is measured. It is assumed that there are minimal changes in coronary diameter, thus enabling velocity to be used in place of flow (flow = velocity × area). Measurements of blood velocity under basal conditions are taken, and then the patient is given a hyperemic stimulus (generally adenosine), velocity is remeasured, and CFR is calculated.
Although the Doppler wire has great theoretical advantages, it is not widely used because of several important limitations. First, conditions other than atherosclerosis can affect CFR. These include factors that raise basal coronary blood flow (e.g., fever, hypoxia, tachycardia, anemia, or ventricular hypertrophy) and factors that impair vasodilatory responses of the microvasculature (e.g., ventricular hypertrophy or diabetes mellitus). Second, accurate measurements are dependent upon correct positioning of the Doppler flow wire. The transducer should be pointing away from the vessel wall and into the flow stream to avoid vessel wall artifacts. Gray-scale signal amplitude and peak velocity can be used as indicators of proper positioning. Third, there is a lack of consensus on what value of CFR is consistent with a hemodynamically significant lesion. In various clinical studies, CFR cutoff values between 1.6 and 2.5 were used to determine ischemia-causing lesions.
Because CFR cannot discriminate between epicardial lesions and microvascular dysfunction, the concept of “relative CFR” (rCFR) was developed. This approach requires that CFR be measured in a coronary artery without epicardial disease to interpret the value of CFR in an artery with epicardial disease. If CFR is abnormal in the artery without disease, this result implies an impaired microvasculature. The use of rCFR has several caveats, including the requirement for a vessel without significant epicardial disease and the assumption that microvasculature function is consistent across different vascular beds (an obvious problem in cases of previous myocardial infarction [MI]).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here