Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Because contact lenses are in direct contact with the eye, it stands to reason that physical forces can act to change the shape of both the lens and the eye. Indeed, both types of change have been documented and both can have important clinical sequelae. This chapter shall concentrate on changes in ocular shape induced by contact lens wear. Primary consideration will be given to corneal shape changes because these are critical to vision and lens-fitting techniques. However, contact lenses can also alter the surface topography of the conjunctiva (e.g. indentation rings) and the form of the upper lid (e.g. rigid lens–induced ptosis).
Consideration will be given to the various manifestations of contact lens–induced changes in corneal topography. The chapter title ‘Corneal warpage’ is adopted because this term has been used consistently in the literature for the past 40 years to imply contact lens–induced shape change. The term ‘warpage’ has the connotation of gross distortion, and this term was no doubt deliberately chosen by the early workers in this field to describe the gross changes in corneal topography that could be induced by scleral or polymethyl methacrylate (PMMA) lenses.
Although rigid lenses made from PMMA are rarely fitted today, evidence of corneal shape change resulting from PMMA lens wear represent a ‘worse case scenario’ in view of their high modulus and lack of oxygen permeability. As such, studies of corneal warpage in response to PMMA lens wear provide important lessons in respect of the extent to which corneal shape can be modified by contact lens wear. For this reason, examples of PMMA-induced corneal warpage will be considered through this chapter. A severe case of rigid lens corneal warpage is shown in Figure 28.1 . Interestingly, some authors have used the term ‘warpage’ to describe corneal shape changes in hydrogel lens wearers.
A myriad of terms have been coined by various authors to describe different phenomena relating to lens-induced corneal shape change; these include ‘deformation’, ‘distortion’, ‘warpage’, ‘indentation’, ‘steepening’, ‘flattening’, ‘sphericalization’, ‘imprinting’ and ‘wrinkling’. These terms are generally self-explanatory and shall be used when discussing specific forms of corneal shape change. Wrinkling is a change that seems to occur in the epithelium and anterior stroma and, as such, was dealt with in Chapter 21 (‘Epithelial wrinkling’).
Although most contact lens–induced corneal shape changes are unintentional, one must not overlook the fact that some clinicians have fitted lenses with the deliberate intention of inducing or arresting corneal shape change; the three best-known practices, which have attracted considerable controversy, are:
cone compression in keratoconus – with the aim of flattening the cone with apical bearing to halt or slow its progression;
orthokeratology – with the aim of flattening the cornea to reduce myopia; and
myopia control – with the aim of preventing the development of myopia or arresting the progression of myopia with reverse-geometry (orthokeratology) rigid lenses.
These concepts, in respect of the induced corneal shape changes, will also be reviewed briefly towards the end of this chapter.
The incidence of corneal shape change caused by various categories of lens wear is well known. Finnemore and Korb reported that 98% of PMMA lens wearers develop central corneal clouding (CCC), which will inevitably cause some degree of corneal steepening. More generalised distortion, or ‘warpage’, was noted in 30% of PMMA lens wearers by Rengstorff.
When assessed using conventional keratometric techniques, current-generation rigid lenses of low to medium oxygen transmissibility (Dk/t) induce little or no change in overall corneal shape during daily wear or extended wear. Similarly, keratometry fails to highlight significant corneal shape changes in daily wear and extended wear of hydrogel lenses.
Corneal topography mapping techniques have revealed that all forms of contact lens wear are capable of inducing small but statistically significant changes in corneal topography. Ruiz-Montenegro et al. reported the prevalence of abnormalities in corneal shape to be 8% in a control group of non–contact lens wearers versus 75% in PMMA lens wearers, 57% in daily rigid lens wearers, 31% in daily soft lens wearers and 23% in extended hydrogel lens wearers. These authors attached some clinical significance to their findings because (a) decreases in best corrected visual acuities (BCVAs) of up to one line of Snellen's acuity were noted in many of the PMMA and rigid lens wearers; and (b) correlations were noted between lens de-centration and corneal shape change.
Wang et al. prospectively studied the eyes of 165 consecutive contact lens–wearing patients evaluated for kerato-refractive surgery. Significant contact lens–induced corneal warpage was detected by corneal topography in 20 eyes of 11 patients, representing an overall prevalence of corneal warpage of 12% among this cohort of contact lens wearers.
The results of studies investigating corneal shape changes with silicone hydrogel lenses are equivocal. Various authors failed to observe corneal curvature changes in patients wearing low-modulus and high-modulus silicone hydrogel lenses during observation periods ranging from 1 to 18 months.
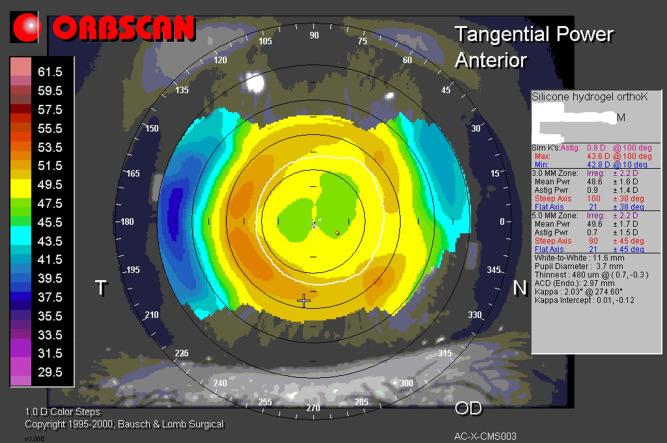
However, Dumbleton et al. observed a small degree of central corneal flattening in both major meridians of 0.35 diopter (D) in patients wearing high-modulus silicone hydrogel lenses over a 9-month period. Gonzalez-Meijome et al. noted a similar phenomenon in silicone hydrogel lens wearers over a 12-month wearing period; specifically, they observed an almost homogeneous increase in corneal radius of curvature for all corneal locations, being statistically significant for the 4-mm cord diameter area. Figure 28.2 shows an example of this phenomenon, where a person with high myopia wore a high-modulus silicone hydrogel lens for 30-day continuous wear, and 3 months after entering this mode of wear, central corneal flattening and 1.00 D of decreased myopia were detected.
Maldonado-Codina et al. noted that over a 12-month period of continuous wear, corneal curvature of subjects wearing high-Dk rigid lenses (Z-alpha; Menicon Co. Ltd., Nagoya, Japan) became flatter by 0.13 mm compared with 0.04 mm for subjects wearing high-Dk silicone hydrogel lenses (Focus Night & Day, Ciba Vision, Duluth, Georgia, USA) (F = 14.7; p = 0.0003). The refractive findings in subjects wearing these lenses mirrored the corneal curvature changes.
Lens binding is known to occur with daily and extended wear of rigid lenses, the clinical evidence of which is an indentation of the cornea that can be seen in white light and with the aid of fluorescein. As indicated by subject reports, lens binding occurred in 29% of patients using daily-wear rigid lenses and 50% of those using extended-wear rigid lenses, respectively.
Tyagi et al. investigated changes in anterior and posterior corneal topography after short-term use of rigid contact lenses in 14 participants who wore 9.5-mm-diameter PMMA lenses, 9.5-mm-diameter rigid lenses, 10.5-mm-diameter rigid lenses and soft silicone hydrogel lenses for 8-hour periods. The PMMA lenses caused flattening in both the central (0.09 ± 0.05 mm, p < 0.001) and peripheral (0.04 ± 0.03 mm, p = 0.006) cornea, whereas the rigid and silicone hydrogel lenses caused no significant changes.
Vincent et al. examined the influence of short-term (3 hours) mini-scleral contact lens wear on corneal shape using Scheimpflug imaging on 10 young (mean 27 years) healthy participants. Small but significant anterior corneal flattening was observed immediately after lens removal (overall mean 0.02 ± 0.03mm, p < 0.001), which returned to baseline levels 3 hours after lens removal. During the 3-hour recovery period, significant posterior surface flattening (0.03 ± 0.02 mm) was also observed (p < 0.01). An increase in lower-order corneal astigmatism Z(2,2) was noted after lens wear. In a separate experiment, Vincent et al. observed posterior corneal topography to remain stable after 8 hours of mini-scleral contact lens wear (− 0.01 ± 0.07 mm steepening over the central 6 mm, p = 0.60).
Most other forms of lens-induced corneal shape change are either rare or are known to be associated with specific types of poorly designed or ill-fitting lenses. Phillips suggested that some patients may be prone to corneal warpage because of previous adverse lens wearing experiences or because of a hereditary predisposition to keratoconus. It is not possible to assign specific incidence figures to such rare phenomena.
The clinical presentation of lens-induced corneal shape change – characterised by time course and precise topographical alterations – can manifest in a variety of forms and will depend primarily on the material, design and fit of the lens. In general, adverse signs and symptoms of corneal shape change include reduced and variable vision, changes in refraction and monocular diplopia. The specific effects of lens-induced shape change shall be considered in the context of the various forms of topographical alterations that have been described.
Much of the earlier literature concentrated on overall changes in curvature, that is, steepening or flattening of the anterior corneal surface as measured by keratometry. Results have been expressed as changes in corneal curvature (in millimetres), surface corneal power (in dioptres) or refraction (in dioptres).
CCC often occurred during the initial period of adaptation to PMMA lens wear and was generally associated with a myopic shift (see ‘Aetiology’ ). Thus, patients newly fitted with PMMA lenses would complain of hazy vision because of the excess oedema and resultant reduced vision upon removing their lenses and putting on spectacles. Some patients would complain of mild ocular discomfort, but this probably relates more to the underlying cause (excessive oedema) rather than to the actual change in corneal shape.
This problem of blurred vision with spectacles after contact lens wear was termed ‘spectacle blur’, and this posed a significant clinical problem because many patients could only wear PMMA lenses for a limited period and needed to wear spectacles at the end of the lens-wearing period.
As the patient adapts and the central corneal oedema subsides, there is a reversal of the induced myopia and the corneal curvature and refraction return to pre-fitting levels. After 12 months of PMMA lens wear, the cornea often displays central flattening, resulting in a hyperopic creep, or reduction in myopia.
Rigid lenses can also induce changes in overall curvature, whereby the extent of change is inversely proportional to the Dk/t and flexibility of the lens. The higher the Dk/t and the more flexible the lens, the less likely are lens-induced changes, assuming a well-fitting lens. Changes in corneal curvature of more than 0.25 D can apparently occur with high-modulus silicone hydrogel lenses but are rare with flexible rigid lenses, low-modulus silicone hydrogel lenses and conventional low-Dk hydrogel lenses.
Clinical evaluation of corneal curvature has traditionally been achieved by using the optical keratometer. This instrument is still of limited use in clinical practice and can generally be relied upon to detect overall compromise to corneal shape. The difficulty arises when attempting to assess asymmetrical or localised regions of corneal distortion because most keratometers are based on an optical configuration that relies upon corneal reflections emanating from a 3-mm-diameter circle on the corneal surface. Thus, localised swelling entirely within or outside this ‘circle’ will go undetected.
Numerous corneal topography instruments are currently available, and all have computerised algorithms for quantifying the degree of irregularity of corneal surface shape. Ruiz-Montenegro et al. used a corneal topography device which computes a function known as the Surface Asymmetry Index (SAI). Specifically, the SAI provides a quantitative measure of the radial symmetry of the four central videokeratoscope mires surrounding the vertex of the cornea. The higher the degree of central corneal symmetry, the lower is the SAI. A high degree of central radial symmetry is characteristic of normal corneas.
Ruiz-Montenegro et al. reported SAI mean values (± standard error of mean) associated with the following forms of lens wear:
non-lens-wearing controls – 0.35 ± 0.03
PMMA – 0.86 ± 0.22
daily-wear rigid – 0.48 ± 0.09
daily-wear hydrogel – 0.48 ± 0.11
extended-wear hydrogel – 0.46 ± 0.08
The SAI was statistically significantly greater than the control group for all forms of lens wear except for daily-wear hydrogel lenses.
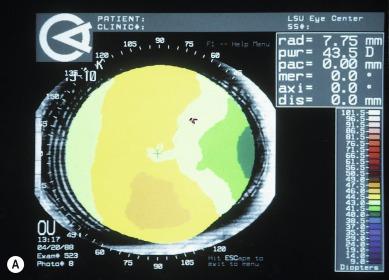
The clinical significance of this finding was highlighted by the fact that the authors observed a correlation between the nature of corneal deformation and the fit of the lens. For example, a superior riding rigid lens was associated with superior flattening, thus explaining the increase in SAI in that case. Such correlations were only observed in PMMA and rigid lens wearers, and an example is depicted in Figure 28.3 .
Obvious corneal asymmetry can be detected by using a keratometer whereby the mires will not be perfectly circular; that is, they make take on an elliptical, pear or egg-shaped appearance. A sequence of progressively increasing levels of keratometer mire distortion is shown in Appendix A ; this can be used as a grading scale for recording the level of severity of lens-induced corneal distortion when using a keratometer.
In addition to SAI, the instrument used by Ruiz-Montenegro et al. also computes a function known as the Surface Regularity Index (SRI). The SRI is a quantitative measure of central and paracentral corneal irregularity derived from the summation of fluctuations in corneal power that occur along semi-meridians of the 10 central photokeratoscope mires. The more regular the anterior surface of the central cornea, the lower is the SRI. The SRI is highly correlated with BCVA.
Ruiz-Montenegro et al. reported SRI mean values (± standard error of mean) associated with the following forms of lens wear:
non-lens-wearing controls – 0.41 ± 0.04
PMMA –1.17 ± 0.34
daily-wear rigid – 0.93 ± 0.18
daily-wear hydrogel – 0.52 ± 0.08
extended-wear hydrogel – 0.51 ± 0.06
The SRI was statistically significantly greater than the control group for PMMA and daily rigid lens wear but not for daily or extended soft lens wear.
The clinical significance of changes in SRI was confirmed by the observation of the authors of an association in PMMA and rigid lens wearers whereby a decrease in BCVA occurred in patients displaying an increased SRI. The patients did not suffer significant discomfort.
A keratometer can detect gross corneal irregularity in the form of lack of clarity of the mires; that is, various sections of the mires will appear to be more in focus than others, and the circular mire lines may not appear to be perfectly smooth. Of course, such an assessment will only relate to the 3-mm-diameter ring of corneal surface that a keratometer samples optically.
Other inexpensive instruments, such as the Placido disc and Klein keratoscope, can provide a similar assessment to that offered by the keratometer, but over a wider expanse of cornea. Needless to say, corneal topography instruments offer distinct advantages over traditional instruments in terms of the extent of corneal coverage, sensitivity, accuracy, objectivity, computational power and data presentation.
Maeda et al. used a corneal topography device to develop an indicator of the asphericity of the central cornea, which they termed the ‘corneal asphericity index’ (CAI). These authors used the CAI to evaluate both normal corneas and corneas with rigid lens–induced warpage. The CAI (mean ± standard deviation) for the 22 control corneas was 0.33 ± 0.26, which indicates that the normal central cornea has a prolate shape. The average CAI for the 24 corneas with rigid lens–induced warpage was significantly lower (− 0.15 ± 0.36). These data suggest that some corneas have abnormal asphericity in the central cornea when warpage occurs with rigid lenses.
Consejo et al. assessed whether short-term soft contact lens wear alters the anterior eye surface. Twenty-two neophyte subjects wore soft contact lenses for a period of 5 hours. Topography-based corneo-scleral limbal radius estimates were derived from height measurements acquired with a corneo-scleral profilometer, and other ocular dimensions were determined by using an optical coherence topography-assisted biometer. Short-term soft contact lens wear was found to significantly modify corneo-scleral limbal radius (130 ± 74 mm, p < 0.001). In contrast, the white-to-white diameter and corneal curvature radius were not modified. Anterior chamber depth and central corneal thickness were significantly affected. Limbal radius increment was reversed 3 hours after lens removal for 68% of the subjects, but the time course of this reversal was not uniform.
Szczotka et al. evaluated 205 patients with keratoconus by using a corneal topography apparatus for both qualitative corneal topographic patterns and quantitative indices. Fifty-six patients were non–contact lens wearers, 130 wore PMMA or rigid lenses and 19 wore hydrogel lenses. Data from the keratoconus patients were also compared with that for a control group comprising normal individuals with no history of contact lens wear.
All three keratoconus groups had a significantly increased frequency of an asymmetrical bowtie/skewed radial axes (AB/SRAX) pattern compared with normal controls. Differences among the videokeratography patterns for the patients with keratoconus included a significant shift from the AB/SRAX videokeratographic pattern to the irregular videokeratographic pattern in the PMMA/rigid lens sub-group and an increased frequency of the irregular pattern in the hydrogel lens group versus the no-lens group. Additional differences between the PMMA/rigid contact lens and no-lens keratoconus groups included increased values for the quantitative indices of SAI, SRI, SIM-K, and central K in the PMMA/rigid lens group.
Rigid lenses can adhere to the cornea during open-eye or closed-eye wear. Adherence can occur at any time of the day in open-eye wear but is characteristically noticed immediately upon eye opening after overnight wear. In the latter case, the lens usually begins to move freely after a few blinks; persistent binding for more than a few minutes is considered problematic. Indentation rings can also be caused by silicone elastomer lenses.
Upon removal of a bound lens, an impression of the lens edge is usually evident on the cornea. Slit lamp examination with fluorescein reveals the presence of an annular indentation in the cornea ( Fig. 28.4 A ), mild punctate keratitis primarily outside the lens edge and dense corneal desiccation inside the lens edge. An imprint from the bound edge after lens removal is clearly visible in Figure 28.4 B, which is an unprocessed image of videokeratoscope rings. Lens binding is usually asymptomatic but can be mildly uncomfortable.

All known forms of contact lens–induced changes to corneal topography can be explained in terms of three underlying pathological mechanisms – (a) physical pressure on the cornea exerted either by the lens and/or eyelids, (b) contact lens–induced oedema and (c) mucus binding beneath rigid lenses. The relative contributions of these factors vary in accordance with the type of topographical alteration.
A comprehensive explanation of corneal shape change during PMMA lens wear has been provided by the classic analysis of Carney – an analysis that can be extrapolated from PMMA lens wear to explain virtually all cases of overall corneal shape change with rigid and soft lens wear.
Carney observed corneal shape changes induced by PMMA lenses in normal atmospheric conditions (21% oxygen) and in artificial conditions ranging from 0% oxygen (anoxia) to 100% oxygen. He demonstrated convincingly that corneal shape change during PMMA lens wear could be attributed to a combination of lens-induced oedema caused by hypoxia and physical pressure from the lens. The precise distribution of these two influences can explain the various forms of topographical changes observed with all forms of lens wear (see ‘Aetiology’ ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here