Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Although reports of contact lens–induced corneal neovascularization can be traced back as far as 1929 it is only in the past five decades that this problem has attracted the attention of contact lens practitioners at large. A variety of terms can be used to describe the vascular response of the cornea to lens wear. This has unfortunately resulted in some ambiguity in the literature, with various authors using different terms to describe the same phenomenon or using the same term to describe different phenomena. Some of the more commonly used terms that are used to define the presence of blood vessels in the cornea are as follows:
Vascularization: The normal existence of vascular capillaries within the cornea (encroaching no more than 0.2 mm into the cornea from the limbus).
Neovascularization: The formation and extension of vascular capillaries within and into previously non-vascularised regions of the cornea.
Limbal hyperaemia: Increased blood flow, resulting in distension of the limbal blood vessels. Hyperaemia may be active, when caused by dilation of blood vessels, or passive, when the drainage is hindered. It is also termed limbal redness , limbal injection or limbal engorgement .
Vessel penetration: Apparent ingrowth of vessels, typically toward the corneal apex, measured from an arbitrary reference at the corneo-scleral junction.
Vasoproliferation: Increase in the number of vessels.
Vascular pannus: Vascularization and connective tissue deposition beneath the epithelium; usually in the superior limbal region. Pannus is Latin for ‘cloth’; an advancing vessel plexus has the appearance of a cloth draping over the cornea.
Vascular response: A general term encompassing any alteration to the normal vasculature, including those entities described earlier.
The original haptic lenses were capable of inducing corneal neovascularization, although there is little data on the magnitude of the problem apart from isolated case reports. Certainly, the prevalence of corneal neovascularization amongst wearers of polymethyl methacrylate (PMMA) lenses has been reported to be very low.
Reports of the prevalence of corneal neovascularization amongst patients wearing hydrogel lenses on an extended-wear basis for cosmetic reasons are inconsistent, with retrospective studies indicating substantially fewer cases of abnormal vascularization than do prospective studies. The prevalence of neovascularization during rigid (gas-permeable) lens wear appears to be extremely small.
The earlier literature reported a greater prevalence of corneal neovascularization in patients using extended-wear hydrogel lenses for correction of aphakia than in cosmetic lens wearers. Such a finding was not unexpected in view of the surgical trauma that the cornea has endured, the compromised physiological status of the cornea as a result of surgery and the necessarily thick lenses needed to be worn to provide the optical correction for an aphakic eye.
The reported prevalence of corneal neovascularization in patients wearing soft lenses for therapeutic reasons varies markedly. The extent of neovascularization in such patients may be related to the underlying corneal pathology being treated, the type of lens fitted and the mode and duration of lens wear.
Published estimates of the prevalence of lens-induced neovascularization reported in clinical trials and surveys are presented in Table 25.1 . When considering the data presented in this table, it is important to bear in mind that there are significant differences among studies with respect to sample sizes, experimental protocols, patient characteristics and criteria chosen for considering a vascular response as being normal versus abnormal.
| Lens type | Mode of lens wear | Lenses replaced regularly? | Patient type | Prevalence of vascularization (%) |
|---|---|---|---|---|
| PMMA | Daily wear | No | Cosmetic | 0.03 |
| Low-Dk rigid | Daily wear | No | Cosmetic | 0.0 |
| Low-Dk rigid | Extended wear | No | Cosmetic | 0.0 |
| High-Dk rigid | Daily wear | No | Cosmetic | 7.3 |
| High-Dk rigid | Extended wear | No | Cosmetic | 7.4 |
| Hydrogel | Daily wear | No | Cosmetic | 0.64 , 1.25 , 14.2 |
| Hydrogel | Extended wear | Yes | Cosmetic | 0.86 , 14.5 , 65 |
| Hydrogel | Extended wear | No | Cosmetic | 0.0 , 0.2 , 1.75 , 7.0 , 8.7 |
| Hydrogel | Extended wear | No | Aphakic | 14.2 |
| Hydrogel | Extended wear | No | Therapeutic | 2.88 , 35.0 |
| Silicone hydrogel | Daily wear | Yes | Cosmetic | 0 |
| Silicone hydrogel | Extended wear | Yes | Cosmetic | 0 |
In 1992, Stapleton et al. reported that, of 1,104 patients with contact lens–related disorders presenting to an acute referral hospital eye clinic, none presented with corneal neovascularization. Of the extensive hospital-based surveys of contact lens complications conducted between 2009 and 2018 – carried out in China, India, Nepal, Singapore, the USA and the UK – the prevalence of corneal neovascularization ranged from 0.1% in the UK to 37% in the USA ( Table 25.2 ). These differences may relate more to the types of clinics (acute referral clinics or general contact lens clinics) and mode of data collection than reflect true differences in prevalence.
| Author | Country | Year | Population size studied | Retrospective or prospective | Prevalence |
|---|---|---|---|---|---|
| Li et al. | China | 2018 | 141 | Retrospective | 5% |
| Sapkota et al. | Nepal | 2013 | 4,064 | Retrospective | 3% |
| Lee et al. | USA | 2012 | 1,369 | Prospective | 37% |
| Teo et al. | Singapore | 2011 | 953 | Prospective | S – 7% D – 0.6% |
| Nagachandrika et al. | India | 2011 | 1,255 | Retrospective | 4% |
| Radford et al. | UK | 2009 | 877 | Prospective | 0.1% |
By using the limit of visible iris as a reference point, McMonnies and co-workers found the mean linear extent of limbal vessel filling, measured inferiorly, to be 0.13 mm in non–lens wearers, 0.22 mm in rigid lens wearers and 0.47 mm in hydrogel lens wearers (daily wear). Stark and Martin and Holden et al. reported an increased vascular response of 0.52 mm and 0.50 mm, respectively, associated with extended hydrogel lens wear.
Whether reports of vascular responses represent filling of capillaries that were empty, dilation of fine vessels that were barely visible, true penetration of vessels into the stroma or a combination of these is often unclear. Nevertheless, the fact that a number of authors have independently established that various modes of lens wear can alter the appearance of the limbal vasculature provides support for the concept of a normal (although in many cases undesirable) lens-induced vascular response.
Adjacent to the limbus, there exists a vascular plexus at all levels from which ingrowing vessels typically emerge. A variety of neovascularization patterns can occur, which are best considered under the following three headings.
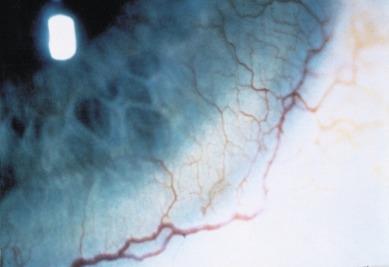
This is the most common form of contact lens–induced vascular response. In the undisturbed eye, episcleral branches of the anterior ciliary artery form a plexus around the limbus known as the ‘superficial marginal arcade’. Minute branches form at right angles to this plexus, encroaching the cornea and looping inward toward the corneal apex ( Fig. 25.1 ). The resultant vascular loops or arcades are typically semi-circular; they tend to anastomose with each successive arc becoming smaller, ultimately forming a rich vascular plexus around the limbus.
New vessels often leak a creamy, lipid-like fluid, which can be seen around vessels on high magnification (see Figure 15.9 ). The combination of extensive vessel formation surrounded by this extravascular fluid can lead to vision loss; however, reduced vision in the case of superficial neovascularization is rare and will only occur if vessels encroach the pupillary axis.
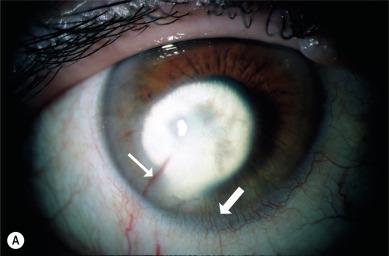
Contact lenses can induce neovascularization at all levels of the stroma, from just beneath the anterior limiting lamina down to the posterior limiting lamina. It develops insidiously and may progress in the absence of acute symptoms. The typical appearance is that of a large feeding vessel emerging sharply from the limbus, usually in the mid-stroma, rapidly developing into finer, wildly tortuous branches and ending in buds with numerous small vessel anastomoses ( Fig. 25.2 ). This irregular pattern is thought to result from a breakdown of structure of the stroma.
Rozenman et al. observed deep stromal neovascularization in five eyes and scarring in five patients wearing soft contact lenses during a 6-month period. There was no evidence suggestive of other causes of interstitial keratitis. Two patients had aphakia and required a penetrating keratoplasty. Weinberg reported the case of a 61-year-old man who developed deep corneal neovascularization, decreased visual acuity and associated corneal opacity at the level of Descemet’s membrane after prolonged wear of a soft contact lens for aphakia. The vascularization markedly diminished and vision improved after cessation of soft lens use; however, the associated opacity remained.
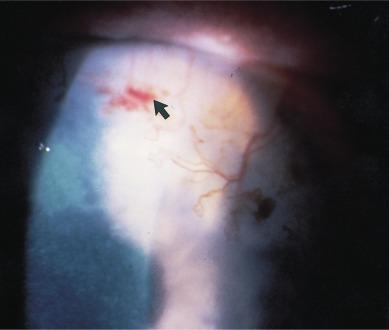
Loss of vision can occur when there has been leakage of lipid into the stroma. Donnenfeld et al. documented five cases of haemorrhaging of deep corneal vessels that were induced by contact lens wear ( Fig. 25.3 ); in one of these cases, a penetrating keratoplasty was required for visual rehabilitation.
Wong et al. reported a case of severe bilateral deep stromal neovascularization and opacification associated with unmonitored contact lens wear. A 46-year-old woman who had been using hydrogel contact lenses, bought without a prescription on the internet, for 5 years was found to have dense, bilateral corneal opacities with deep stromal neovascularization. The contact lenses of the patient were found to be tight-fitting. Medical history and serological studies were negative for infectious or rheumatological causes of interstitial keratitis. The authors concluded that this condition was most likely related to the unmonitored contact lens use and the lack of routine eye examinations.
Ang et al. described a technique of adapting a swept-source optical coherence tomography angiography instrument to image stromal vascularization, which enabled them to differentiate between superficial and deep vascular progression.
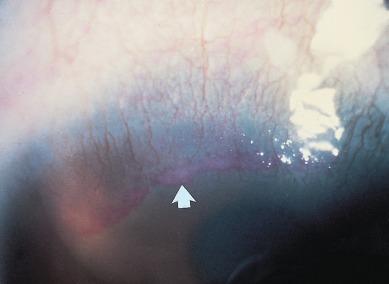
A pannus is an extensive ingrowth of tissue from the limbus onto the peripheral cornea. The penetration occurs between the epithelium and the anterior limiting lamina, resulting in a separation of these layers and often leading to a destruction of the anterior limiting lamina. The term ‘micropannus’ is used when the extent of invasion is less than 2.0 mm from the limbus ( Fig. 25.4 )

There are two forms of pannus – active (inflammatory) and fibro-vascular (degenerative); both types may be observed in contact lens wearers. An active pannus is avascular and is composed of sub-epithelial inflammatory cells. In the later stages, it may be associated with secondary scarring of the stroma.
A fibro-vascular pannus consists of an ingrowth of collagen and vessels and often contains fatty plaques. The clinical appearance of a fibro-vascular pannus is a congested band of vessels penetrating in an orderly fashion in the cornea, with the limit of penetration remaining even across its width. The invading end of the pannus often contains a considerable amount of fibrotic tissue, which stains brightly with rose bengal ( Fig. 25.5 ). This condition is observed in contact lens–wearing patients in association with superior-limbic keratoconjunctivitis. As this name suggests, the pannus is observed at the superior limbus.
Corneal neovascularization is generally considered asymptomatic, which is why the condition is so insidious. However, Nomura et al. examined 181 Japanese adults visiting an eye clinic for contact lens fitting and graded the degree of corneal neovascularization. These authors found a significant association between the extent of neovascularization and the subjective symptom of dryness.
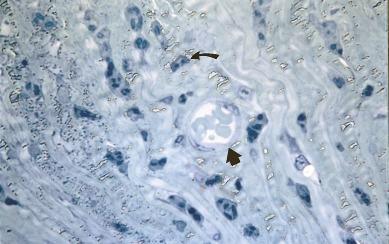
The ultrastructural tissue changes observed in contact lens-induced corneal neovascularization were described by Madigan et al. in a primate model. Vessel lumina were approximately 15 to 80 μm in diameter and contained erythrocytes and sometimes leucocytes. Numerous extravascular leucocytes were observed around blood vessels, and the surrounding stromal lamellae were disorganised and separated with lines of keratocytes lying between them ( Fig. 25.6 ). The overlying corneal epithelium was often affected, with general oedema, cell loss, and the presence of large fluid-filled vesicles. The underlying Descemet’s layer and endothelium were apparently unaffected.
The likely sequelae of events in the development of a vascular response can be predicted based on general vascular response studies in lower animals. In particular, detailed investigations of corneal neovascularization in the rat occurring after focal injury caused by chemical cautery have allowed three distinct phases of vessel formation to be defined – the pre-vascular latent period, neovascularization and vascular regression.
Numerous theories have been advanced to explain why corneal neovascularization occurs, all of which are potentially relevant to the contact lens–induced vascular response. These theories are summarised in the following.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here