Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Corneal deposits can be classified by the layer where they are found in the cornea: superficial, stromal, and deep stromal.
Corneal deposits can also be classified by their color: pigmented, nonpigmented, and retractile/crystalline.
Heavy metals such as silver, copper, and gold can be deposited in the cornea.
Systemic diseases can be diagnosed initially on the basis of the observation of corneal deposits. Examples include Fabry disease, mucopolysaccharidoses, cystinosis, and Wilson disease.
Abnormal deposition of material in the cornea is easily discerned for two reasons. First, the cornea in its normal state is clear, and deposits of any type produce clouding. Second, the details of the cornea can be readily examined with a slit lamp, which magnifies the cornea under conditions of variable illumination.
This chapter presents a systematic approach to the evaluation of the patient with corneal deposits. The focus is on achieving the correct diagnosis by evaluating two major aspects of the deposits: the depth of the deposit in the corneal stroma and the color of the deposits. Identifying the location and color of the deposits considerably shortens the differential diagnosis.
The cornea can be divided into three depths: superficial, stromal, and deep stromal. The superficial layer corresponds histologically to the epithelium, Bowman layer, and the very anterior stroma. The stromal layer represents the bulk of the histologic, anatomic stroma. The deep stromal layer is defined as the deep posterior stroma, Descemet membrane, and the endothelium.
The color of the deposits can be divided into three categories: pigmented, nonpigmented, and refractile/crystalline. Pigmented deposits can be any color but typically are yellow or brown. Nonpigmented deposits are white or gray. Refractile or crystalline deposits are clear with indirect illumination but may be white or gray with direct illumination. Occasionally, crystalline deposits may be polychromatic.
The reader is referred to the appropriate nine groupings in Table 22.1 . The text highlights further specifics of the deposits.
| Superficial | Stromal | Deep Stromal | |
|---|---|---|---|
| Pigmented | Cornea verticillata (Fabry disease and drug effects) Striate melanokeratosis Epithelial iron lines Spheroidal degeneration Adrenochrome |
Phenothiazines Blood staining Bilirubin Siderosis (iron) |
Wilson disease (copper) Chalcosis Chrysiasis (gold) Mottled cyan opacification Deep blue dot degeneration |
| Nonpigmented | Subepithelial mucinous dystrophy Coat’s white ring Calcific band keratopathy Fluoroquinolones Mucin balls |
Granular dystrophy Macular dystrophy Fleck dystrophy Lipid deposition Mucopolysaccharidoses |
Cornea farinata Pre-Descemet dystrophy X-linked ichthyosis Argyrosis (silver) |
| Refractile/crystalline | Meesmann dystrophy Gelatinous drop-like dystrophy Tyrosinemia II Intraepithelial ointment Gout (urate) |
Lattice dystrophy Schnyder dystrophy Bietti dystrophy Immunoglobulin Cystinosis |
Polymorphic amyloid degeneration |
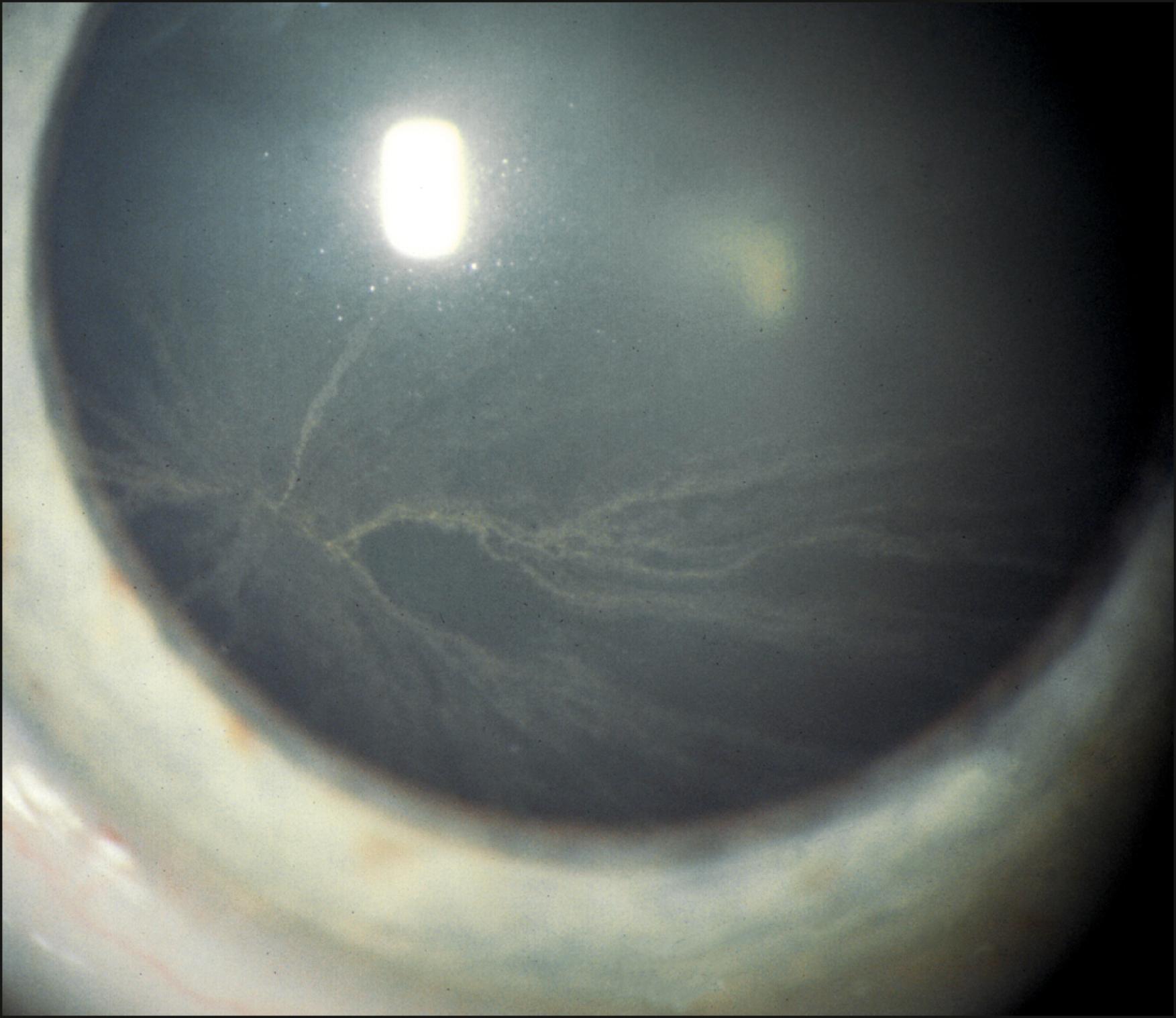
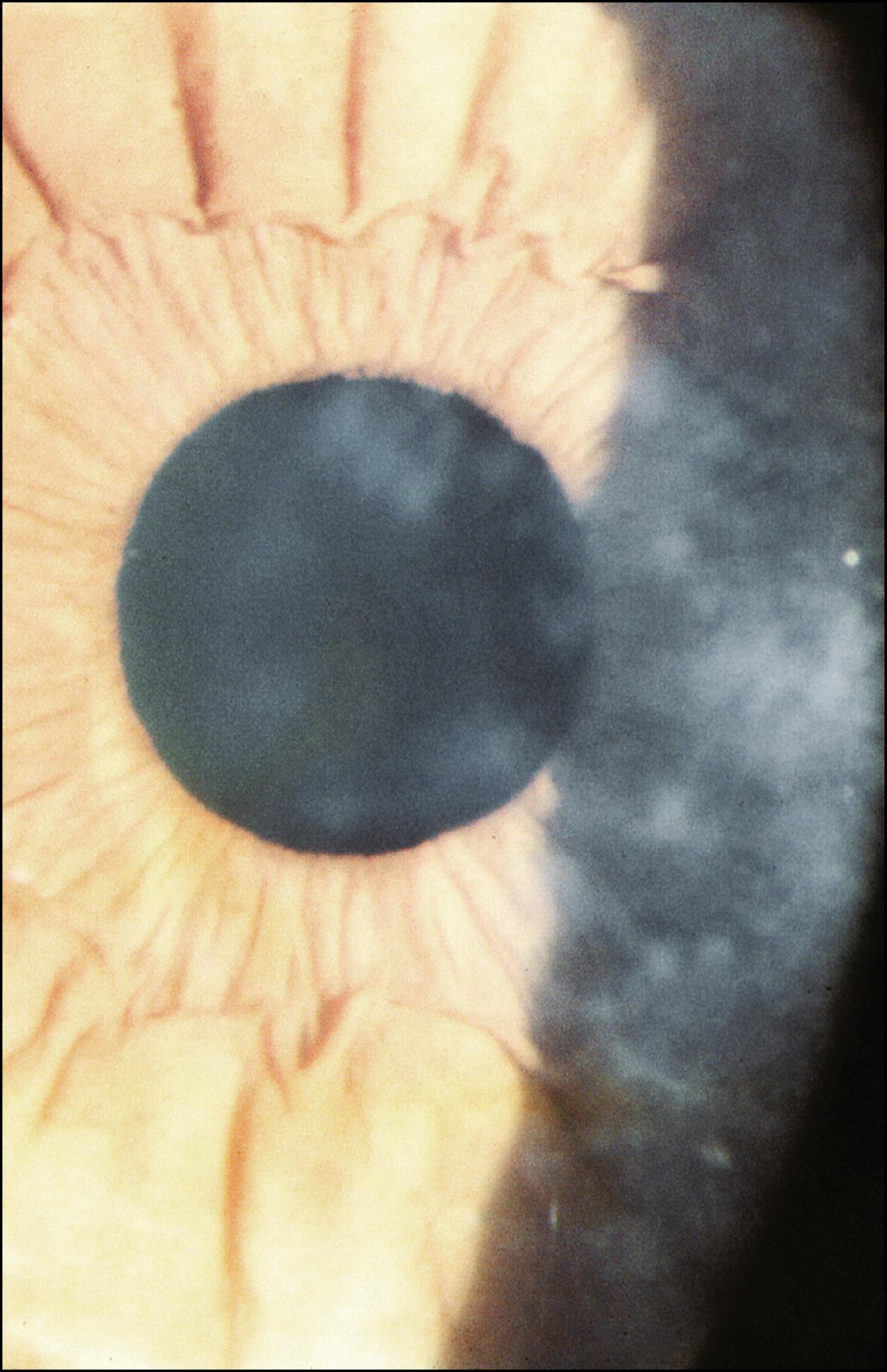
Cornea verticillata refers to linear opacities located within the corneal epithelium that assume a characteristic whorl-like pattern ( Fig. 22.1 ). The opacities are located primarily in the inferior paracentral cornea and are not elevated. Their color may vary from white to brown. Cornea verticillata is seen in Fabry disease and as a side effect from multiple systemic medications including amiodarone, chloroquine, quinacrine, chlorpromazine, indometacin, clofazimine, suramin, naproxen, and tilorone. Fabry disease is an X-linked lysosomal storage disease, which results in the accumulation of trihexosylceramide. , Corneal changes are found in both the hemizygote male and heterozygote female carriers. A spiraling corneal epithelial opacification has been seen as the presenting sign of multiple myeloma.
Striate melanokeratosis refers to pigment lines located in the epithelium, which extend from the limbus toward the central cornea ( Fig. 22.2 ). These lines normally occur in darkly pigmented individuals but can also occur in lighter pigmented individuals after injury or inflammation. The deposits are probably the result of migration of pigmented limbal stem cells onto the cornea.
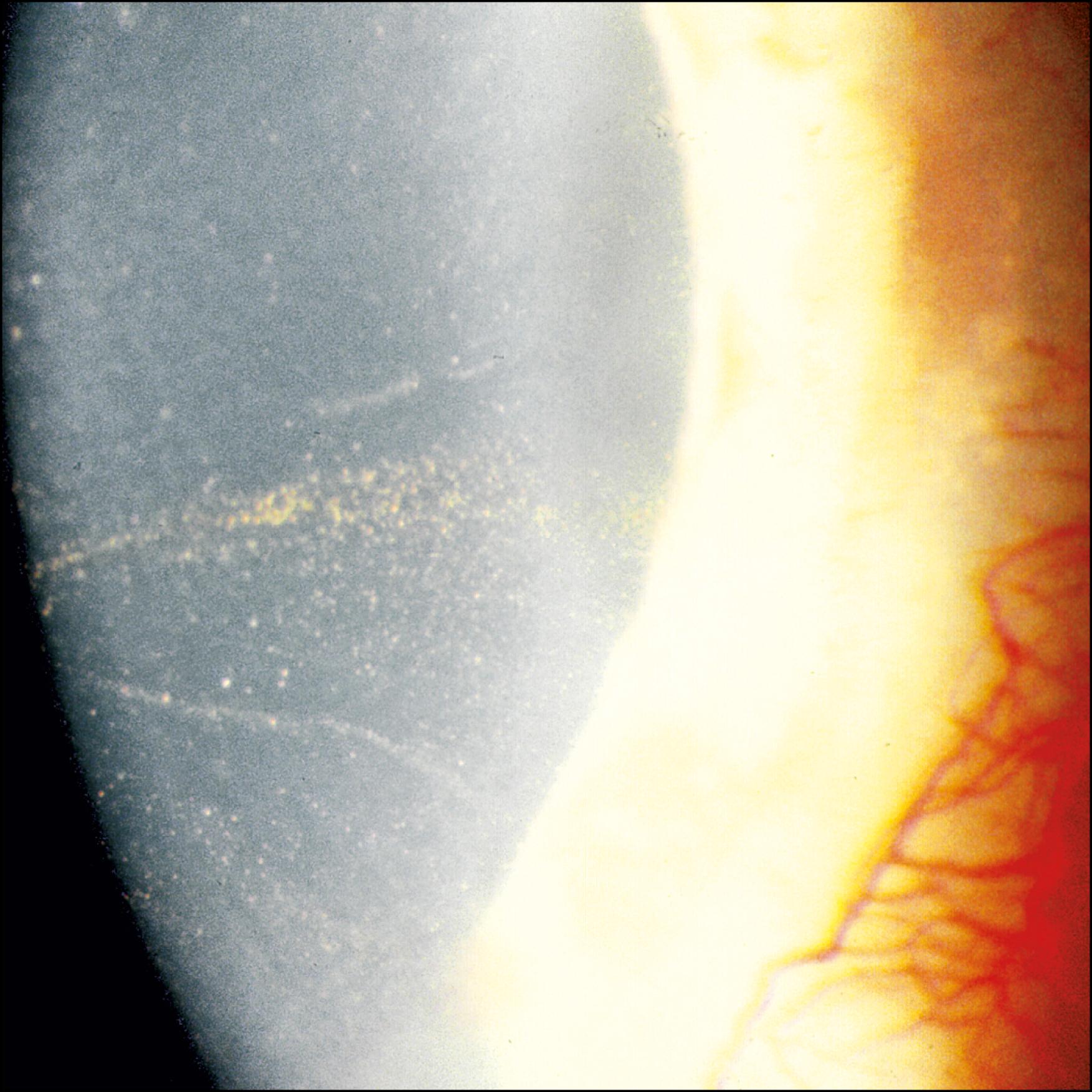
Iron deposits in the epithelium have a yellow-brown coloration ( Fig. 22.3 ). Pooling of tears in the region of topographic irregularities allows iron from the tear film to be deposited within the epithelium. Iron lines can be seen in the palpebral fissure (Hudson-Stahli), at the head of a pterygium (Stocker), surrounding the cone in keratoconus (Fleischer), at the head of a filtering bleb (Ferry), adjacent to areas of corneal elevation such as Salzmann nodular degeneration, anterior to the sutures in keratoplasty (Mannis), and after keratorefractive surgery. ,
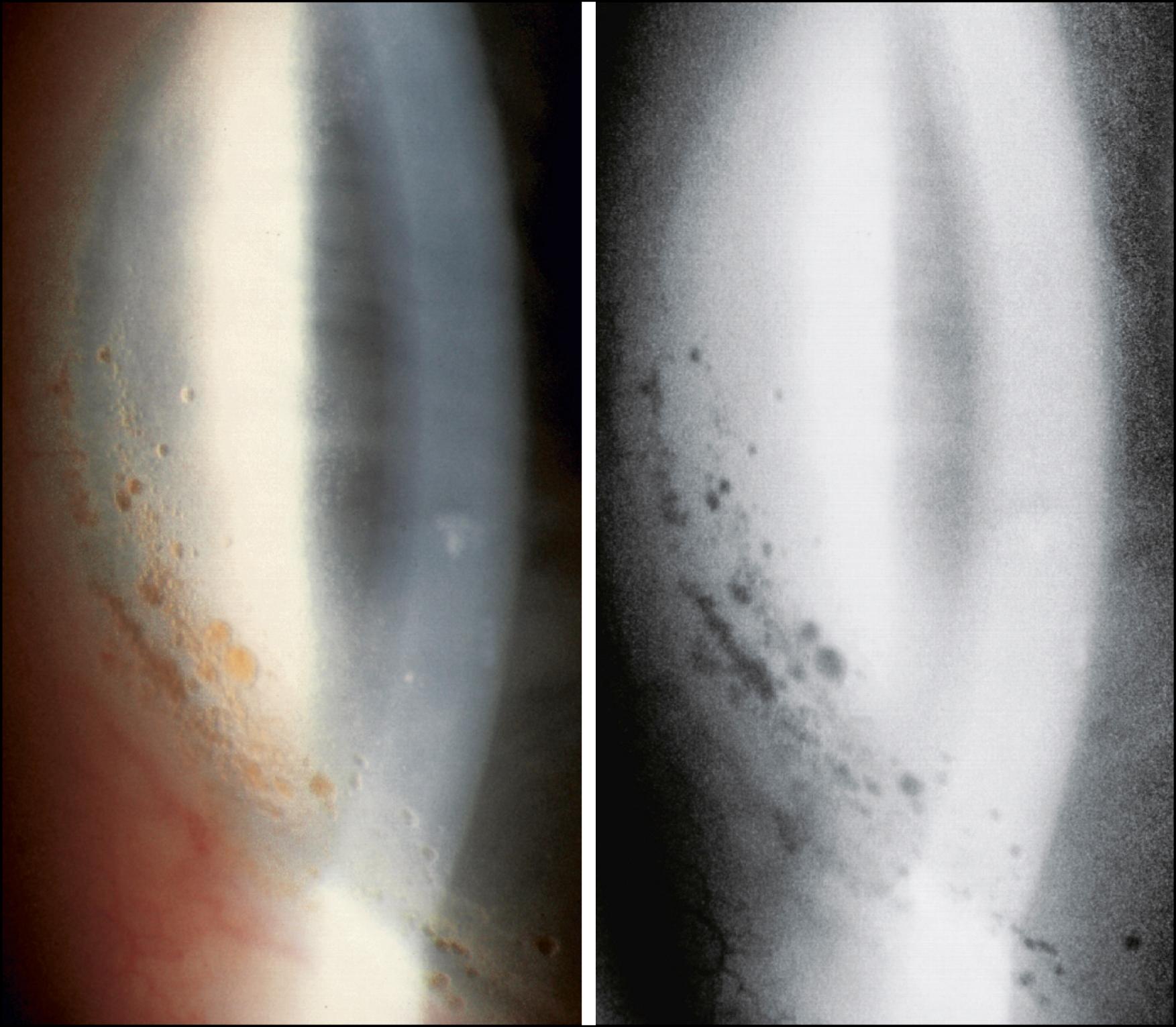
Spheroidal degeneration produces golden-yellow globular deposits within the interpalpebral area ( Fig. 22.4 ). The deposits are located within Bowman layer and the anterior stroma. In primary spheroidal degeneration, the deposits are bilateral and initially located in the nasal and temporal cornea; they can extend onto the conjunctiva. Secondary spheroidal degeneration is associated with ocular injury or inflammation. The deposits in secondary spheroidal degeneration will aggregate near the area of corneal scarring or vascularization.
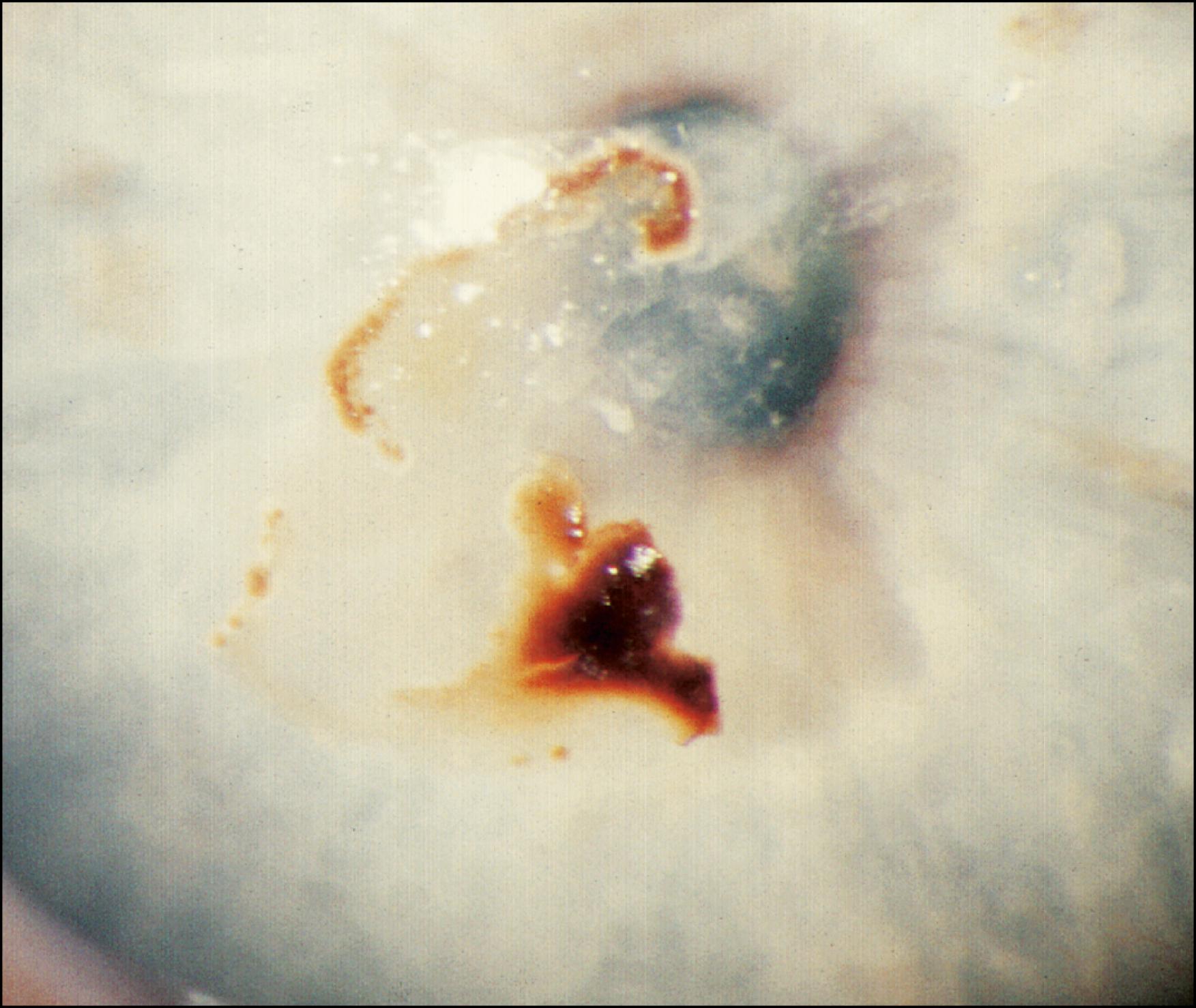
Adrenochrome deposits are usually found within the conjunctiva but rarely may occur on the corneal surface ( Fig. 22.5 ). These brown-black deposits occur in patients treated with epinephrine eye drops for glaucoma.
Subepithelial mucinous corneal dystrophy is an autosomal dominant condition, which results in the deposition of glycosaminoglycans in the subepithelial stroma ( Fig. 22.6 ). Clinically, a diffuse, homogeneous subepithelial haze is seen bilaterally. The haze is denser centrally and fades toward the periphery. Irregular gray-white opacities may also be seen centrally; these deposits may be raised.
Coat’s white ring is a superficial ring of iron deposition that remains after a metallic foreign body is removed ( Fig. 22.7 ). Small white opacities may be seen inside the ring. These rings develop when a rust ring from an iron foreign body is not entirely removed.
Hypercalcemia and chronic ocular inflammation are the most common conditions associated with calcific band keratopathy ( Fig. 22.8 ). The calcium is deposited within the epithelial basement membrane, Bowman layer, and the anterior stroma. Clinically, subepithelial chalky, white deposits are found in the interpalpebral zone. The deposition initially begins in the peripheral cornea, with a clear margin separating the deposit from the limbus. The clear interval is thought to represent the anatomic limit of Bowman layer. Throughout the band are clear, small holes that give a “Swiss cheese” appearance. The holes occur at sites where corneal nerves penetrate Bowman layer.
Topical ciprofloxacin, norfloxacin, Tosufloxacin, and Gatifloxacin therapy can result in the deposition of a chalky, white precipitate within an epithelial defect ( Fig. 22.9 ). Although they are predominantly white in appearance, a crystalline pattern may also be observed.
Mucin balls are round, white deposits that accumulate between the posterior surface of a contact lens and the corneal epithelium ( Fig. 22.10 ). When the contact lens is removed, the mucin balls may be blinked away, but in some cases, they remain adherent to the cornea for several hours. When they are removed, they leave a depression in the epithelium. They are more common with rigid soft contact lens material such as high-Dk silicone lenses.
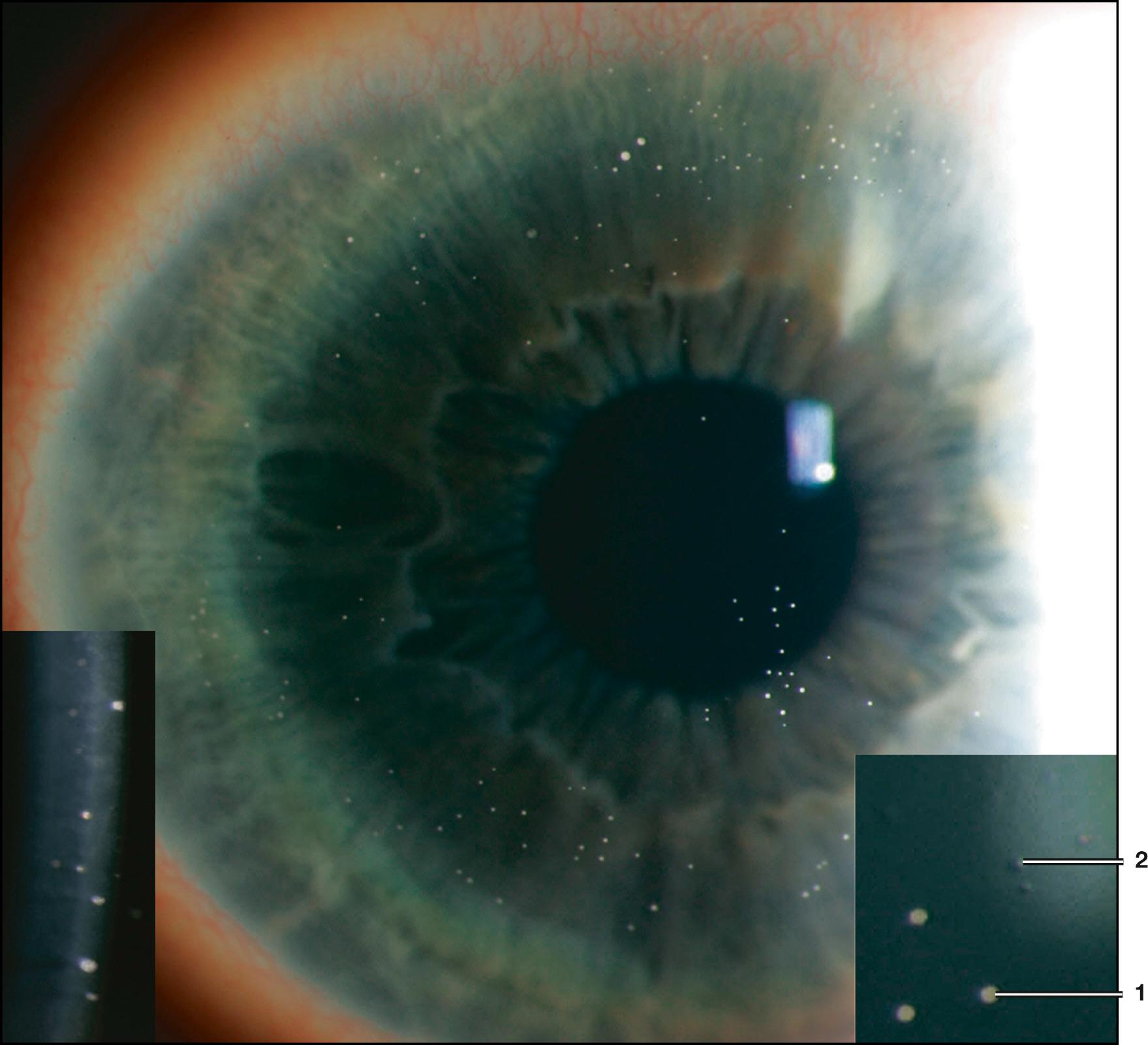
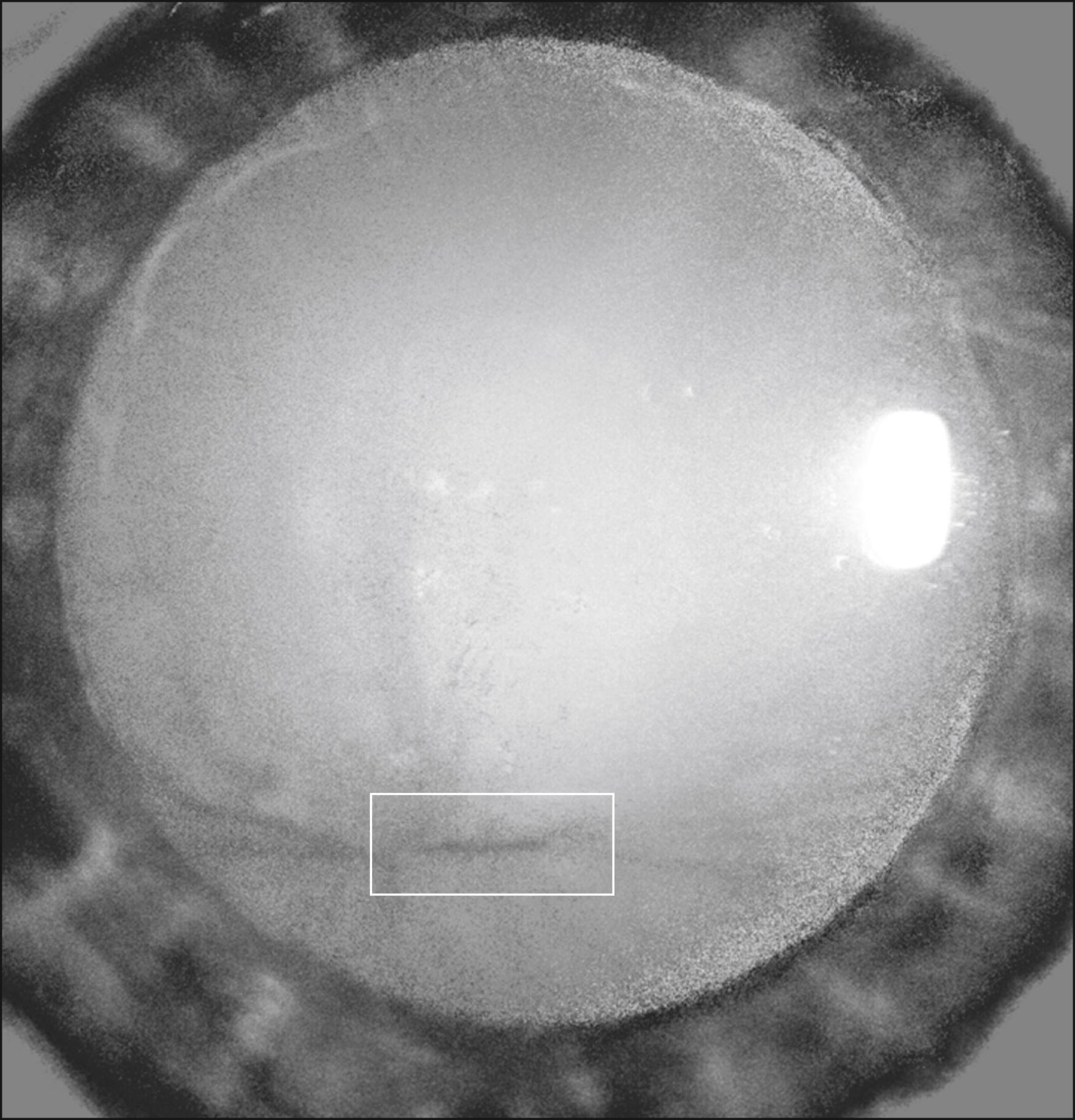
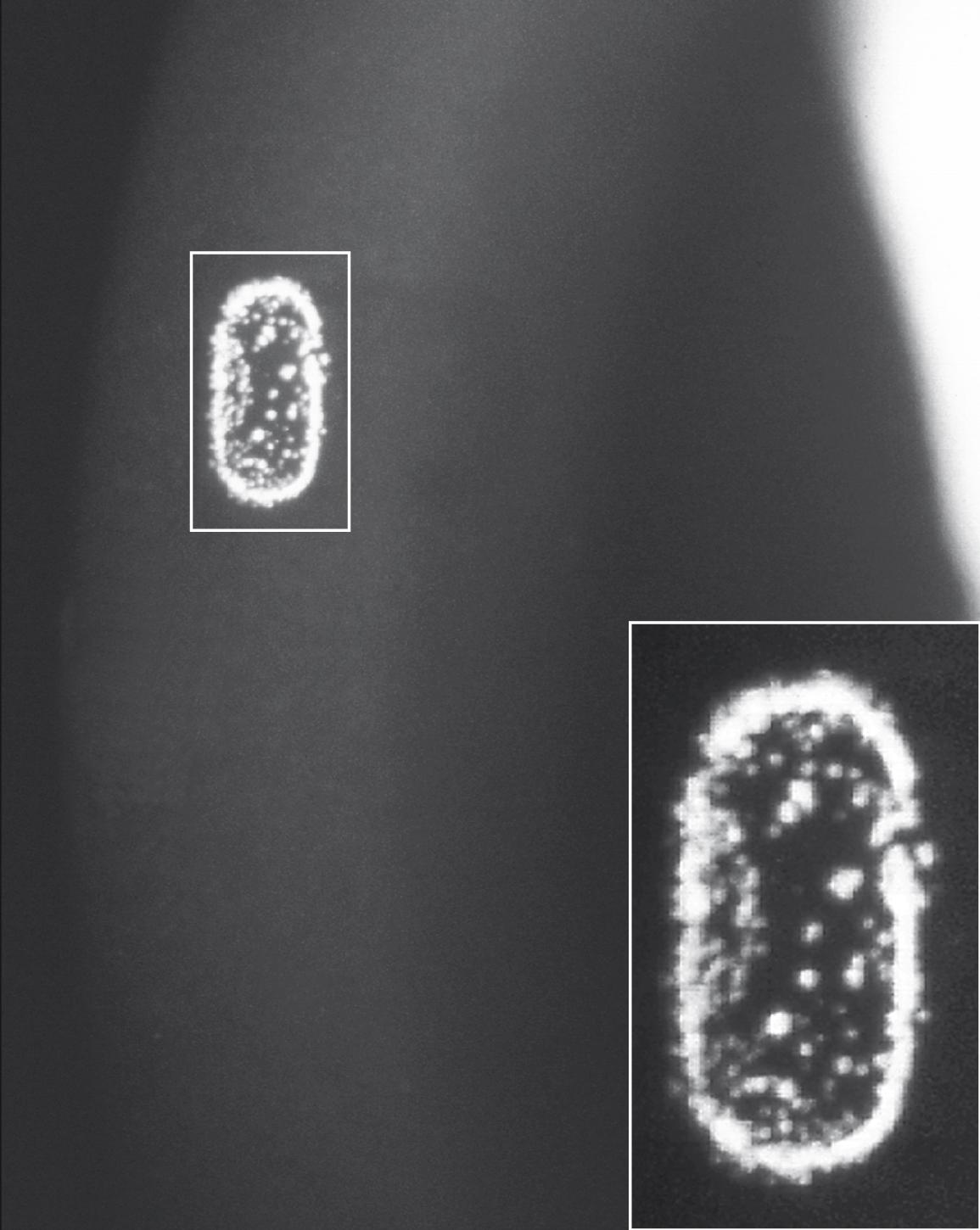
Meesmann dystrophy (MECD) is an autosomal dominant disorder that results in the accumulation of bilateral intraepithelial cysts throughout the cornea ( Fig. 22.11 ). These cysts appear gray on direct illumination but with retroillumination are transparent and are thus better viewed. The cysts are confined to the epithelium and extend to the limbus. The intervening cornea is clear.

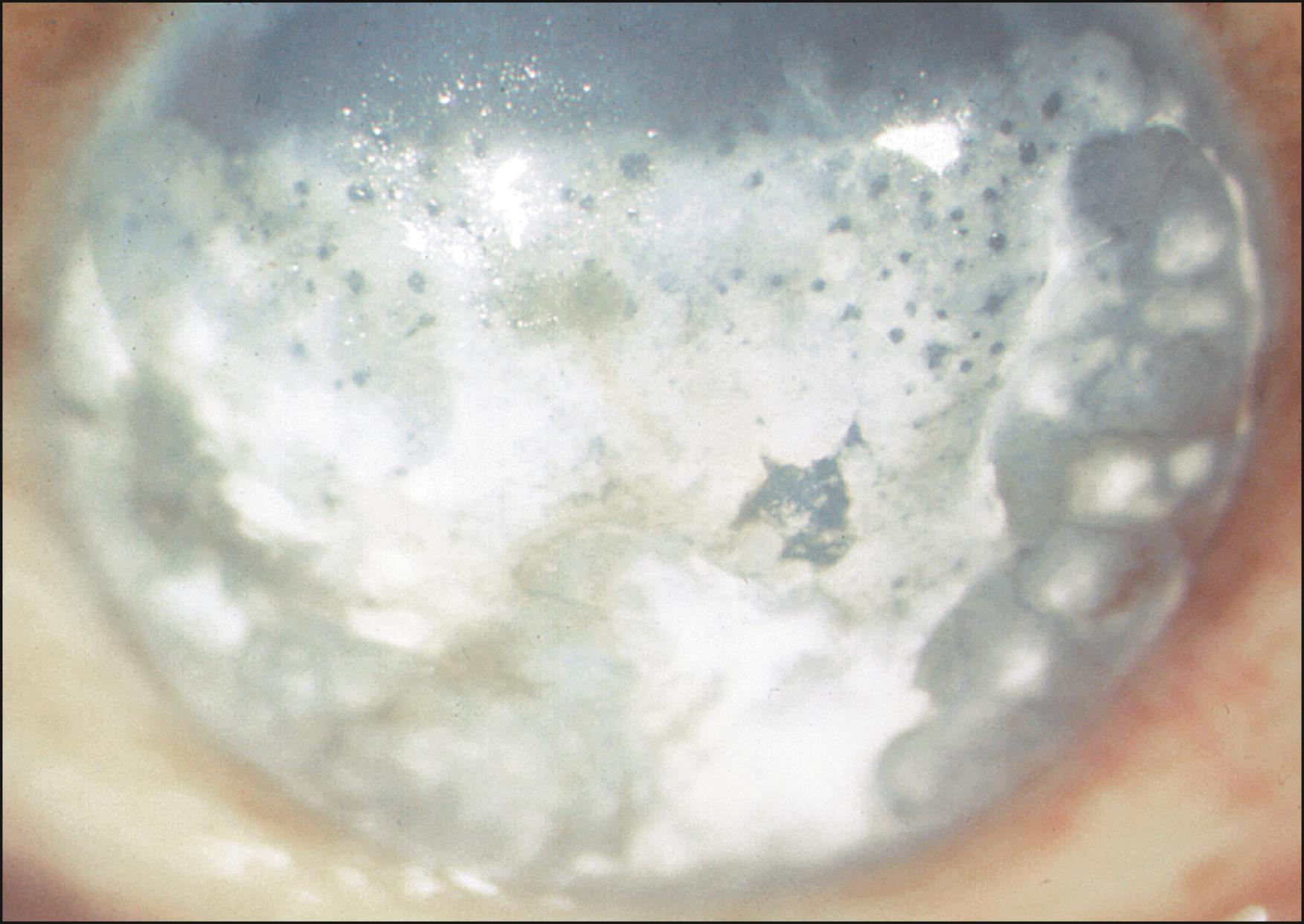
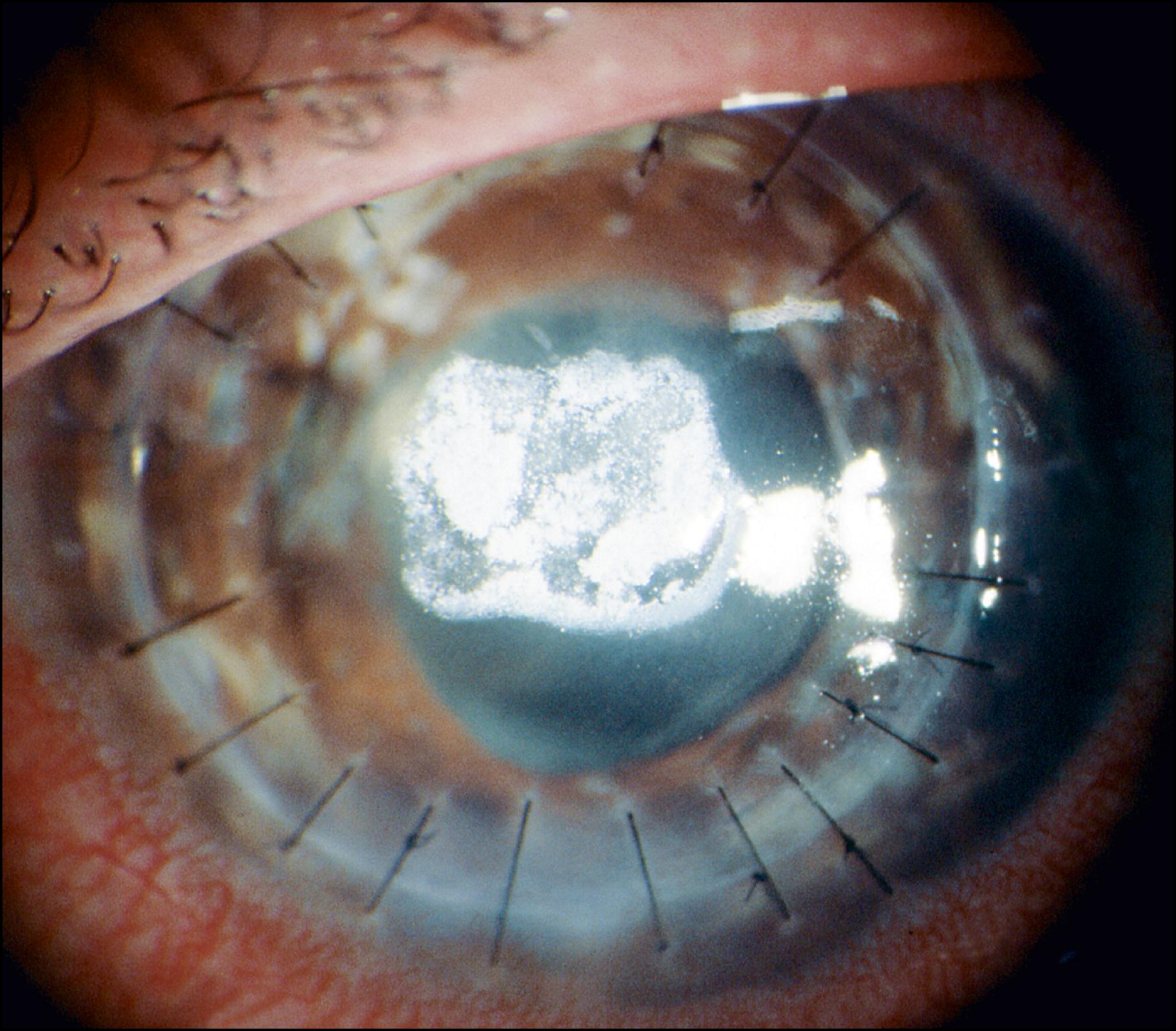
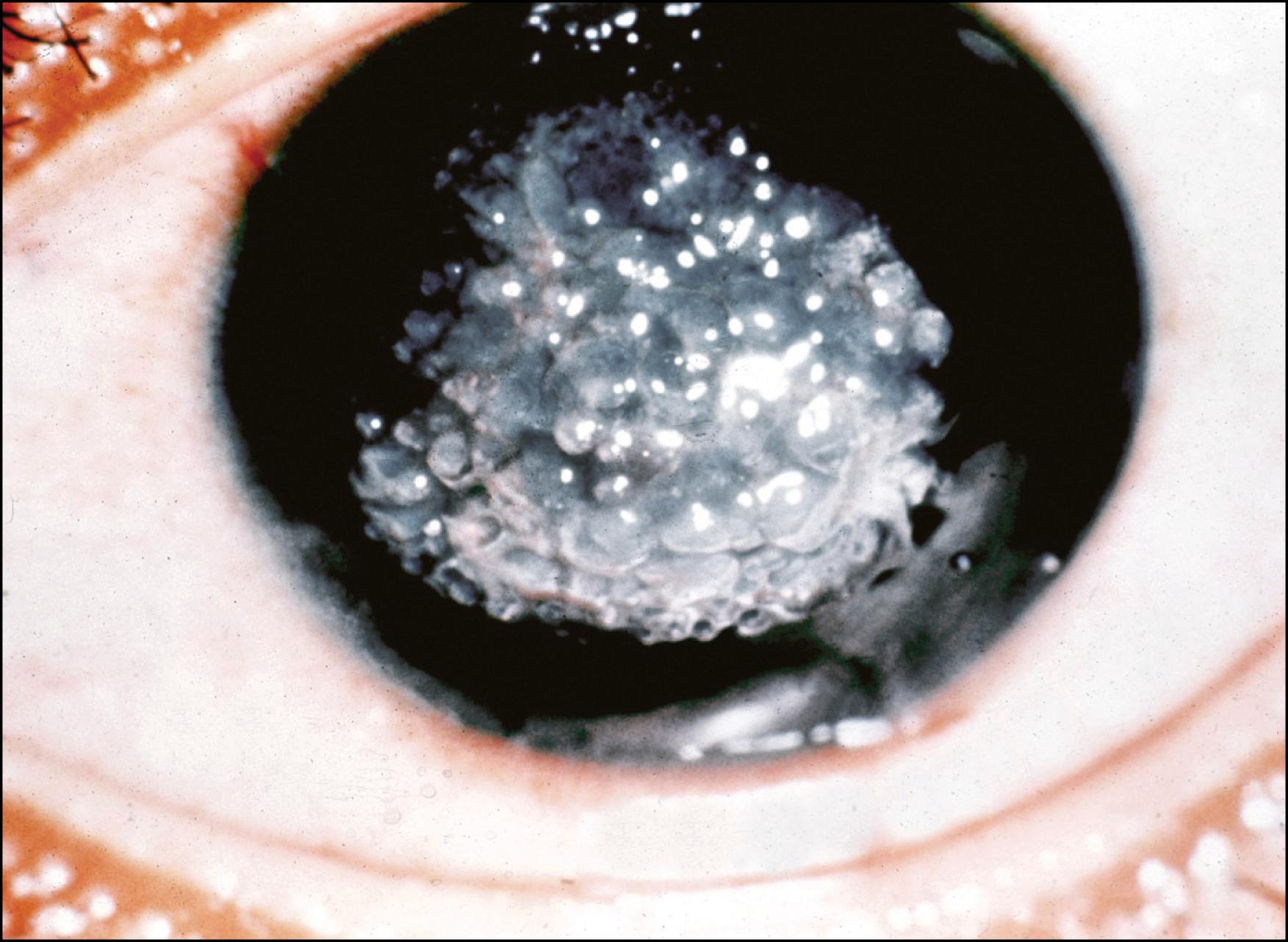
Gelatinous drop-like dystrophy (GDLD) is an autosomal recessive disorder that results in the bilateral accumulation of amyloid deposits in the anterior corneal stroma ( Fig. 22.12 ). This condition, as well as lattice dystrophy, is a form of primary localized corneal amyloidosis. Clinically, subepithelial raised, gelatinous deposits appear within the first or second decade. These deposits are refractile on indirect illumination, limited to the central cornea, and have been likened to the appearance of a mulberry.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here