Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cutaneous lupus erythematosus is a disease with a wide spectrum of manifestations ranging from solitary chronic skin lesions in chronic cutaneous lupus erythematosus (CCLE), to widespread polymorphous lesions in subacute cutaneous lupus erythematosus (SCLE), to multiple-organ involvement in systemic lupus erythematosus (SLE). Lupus is thought to be a dysregulation of T cells causing the activation of B cells, producing a variety of autoantibodies directed against cellular antigens, such as DNA, RNA, and RNA–protein complexes.
Beware of drug-induced lupus variants; the clinical manifestations and serum findings are similar to idiopathic lupus. These variants include drug-induced SLE, SCLE, and CCLE. Drugs most frequently associated with drug-induced SLE are hydralazine, procainamide, isoniazid, methyldopa, chlorpromazine, quinidine, and minocycline. Drug-induced SLE usually spares kidneys and the central nervous system.
Review drug associations and, when possible, remove suspect medications that may be triggers of disease.
Sunscreen use and sun avoidance behavior are an essential element of therapy.
Sunscreens should be used that block broad-spectrum ultraviolet A—especially ones that contain Mexoryl SX (ecamsule) or Mexoryl XL or titanium dioxide and zinc oxide.
Excellent broad-spectrum sunscreens are Anthelios XL SPF 60 (La Roche−Posay) or Ombrelle SPF 60 sun cream (L'Oreal).
Sun-protective clothing is available from Sun Precautions (2815 Wetmore Avenue, Everett, WA 98201; Tel: 1–800–882–7860; http://sunprecautions.com ), Coolibar ( http://www.coolibar.com ), and from many other vendors.
Vitamin D should be supplemented because patients are likely to have low vitamin D levels from sun avoidance.
Smoking cessation should be encouraged because better disease control may be achieved. Less response to treatment is seen in smokers.
There are many treatment options. Whether to use a topical agent alone or with the addition of a systemic agent depends on the degree of disease extent and severity and other individual underlying medical conditions.
Newer immune modulators, pimecrolimus cream (Elidel) or tacrolimus ointment (Protopic), can be effective adjunctive therapy. Both are applied twice daily to lesional skin for extended periods and may be preferred first-line topical therapy for facial lesions.
Topical or intralesional corticosteroids, retinoids, and oral antimalarial therapy are standard treatments.
Cyclical use of groups I and II topical steroids; these are administered twice a day for 2 weeks, and moisturizers are used for 1 week.
Steroids, such as triamcinolone (Kenalog) 10 mg/mL, are injected into CCLE lesions.
Corticosteroid-impregnated tape (Cordran tape) is an option for CCLE lesions.
Hydroxychloroquine 200 to 400 mg once daily (dose less than 6.5 mg/kg once daily) is an effective first-line oral treatment in most cases; the onset of effect requires 4 to 8 weeks. Ophthalmic examinations are required at baseline and every 6 months to 1 year. Quinacrine can be added for resistant disease at a dose of 50 to 100 mg/day.
Other medications for cutaneous lupus erythematosus that may be considered include dapsone 25 to 200 mg twice daily (especially useful for bullous lupus erythematosus, vasculitic lesions of lupus erythematosus, or urticarial vasculitis associated with SCLE, and oral ulcerations); thalidomide in divided doses of 50 to 300 mg a day; sulfasalazine divided doses of 1.5 to 2 g/day; retinoids (e.g., acitretin 10 to 50 mg once daily or isotretinoin 1 mg/kg once daily). Prednisone 0.5 to 1.5 mg/kg once daily is an option, but long-term treatment should be avoided. Steroid-sparing immunosuppressive options include azathioprine (1–2.5 mg/kg/day); methotrexate (up to 20 mg once a week); mycophenolate mofetil (500–1000 mg twice daily); or cyclophosphamide.
High-dose intravenous immune globulin (IVIG) 1 g/kg once daily for two consecutive days a month can be used when other agents fail; treatment is expensive, and response duration is limited.
Rituximab alone or in combination therapy has been successful in treating patients with severe refractory cutaneous lupus erythematosus.
Skin disease often occurs with systemic disease in patients with SLE. Such patients require systemic immunosuppressive therapy to treat this form of lupus.





CCLE is the most common form of cutaneous lupus erythematosus; lesions may be localized to the head and neck or widespread and consist of scaling erythematous papules and plaques, often with central atrophy and scarring.
CCLE lesions are not always “discoid,” and this term should no longer be used.
CCLE is more common in women.
It is perhaps more common in people with an African American background.
The peak incidence is in the fourth decade.
Trauma and ultraviolet light may initiate and exacerbate lesions.
Photosensitivity is present in 50% of patients with lupus erythematosus.
There is a lower incidence of systemic disease; 1% to 5% of cases progress to SLE. Patients with nonlocalized, widespread disease are at greater risk for advancing to systemic disease.
Scarring alopecia is permanent.
Drug-induced CCLE is rare and may be provoked by tumor necrosis factor (TNF)-alpha inhibitors.
Pediatric discoid lupus erythematosus (DLE) is uncommon but is associated with SLE when lesions are generalized.
Antinuclear antibodies (ANAs) are positive in only 20% of cases; anti-Ro antibody is very uncommon.
Assess for SLE with a complete blood count, urinalysis (proteinure higher than 3), antinuclear antibody, erythrocyte sedimentation rate. If ANA is positive, then assess for extractable nuclear antibodies (double-stranded DNA, SS-A/SS-B, anti-Smith antibody, antiphospholipid antibody).
Skin biopsy shows an interface dermatitis with follicular plugging, perivascular and periappendeal infiltrate, and possibly scarring.
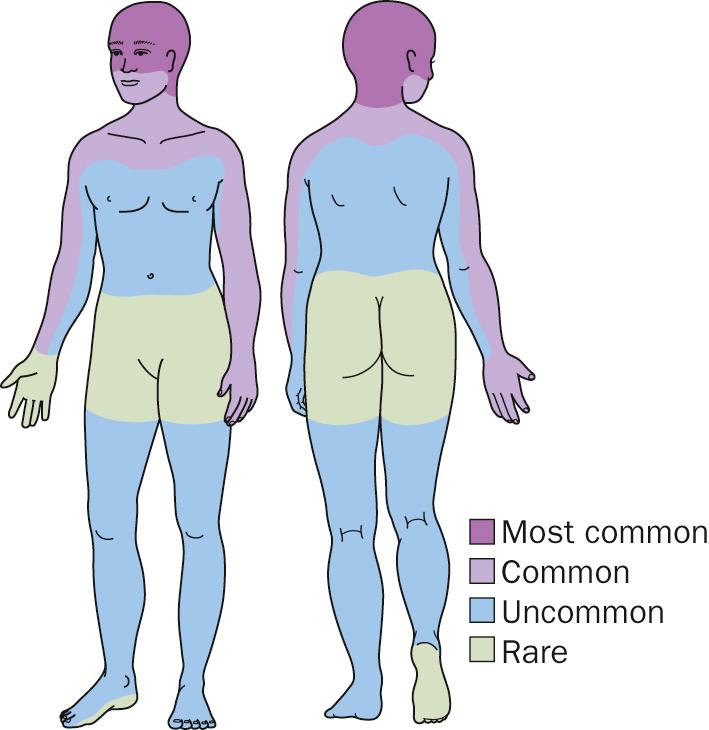
Lesions may occur on any body surface, but the scalp, face, and ears are the most common areas.
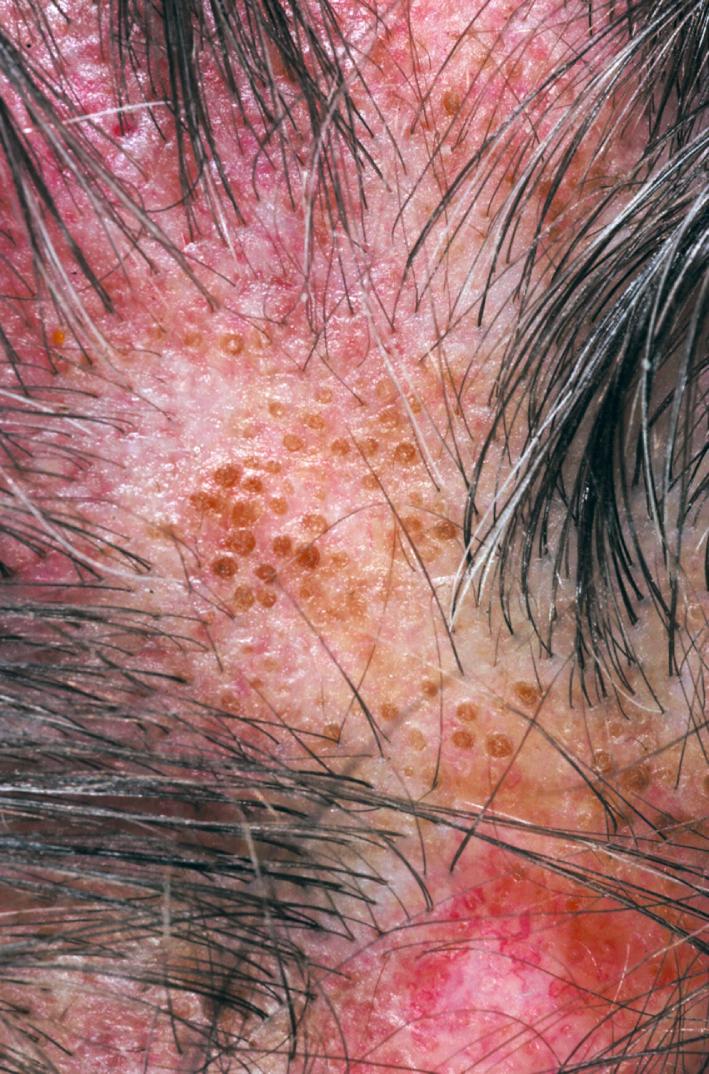
Chronic lupus erythematosus begins asymptomatically; there are well-defined, elevated, red to violaceous, 1- to 2-cm, flat-topped plaques with firmly adherent scaling.
Follicular plugs are prominent; peeling the scale reveals an undersurface that looks like a carpet penetrated by several carpet tacks.
Epidermal atrophy gives the surface either a smooth white or wrinkled appearance.
Lesions may be hypertrophic or verrucous; they may involve the palms and soles or the oral mucosa.
Lesions endure for months; they either resolve spontaneously or progress with further atrophy, ultimately forming smooth, white or hyperpigmented, depressed scars with telangiectasia and scarring alopecia.
Scalp disease begins with erythema, scaling, and follicular plugging.
Hair follicles are destroyed, resulting in irreversible, scarring alopecia. Hair loss is haphazard in distribution.
Drug-induced CCLE may have classical discoid lesions or lupus tumidus lesions. An ANA test is positive in two thirds of cases.
Initial treatment options include groups I to III topical steroids (i.e., fluocinonide cream 0.05%), intralesional steroids, antimalarials (e.g., hydroxychloroquine 200 mg twice daily), or acitretin 25 to 50 mg/day. Hydroxychloroquine and acitretin work equally well, but acitretin has more side effects and is more costly. Other alternative treatments include dapsone and oral corticosteroids. Difficult cases can be treated with methotrexate, azathioprine, thalidomide, or isotretinoin. IVIG may be tried in recalcitrant disease. Sunscreens are an essential aspect of therapy. Some patients may respond to tacrolimus ointment (Protopic). A broad-spectrum, water-resistant sunscreen should be applied daily (see treatment overview ).






SCLE is a form of cutaneous lupus erythematosus typically characterized by nonscarring, erythematous psoriasiform lesions or annular lesions in a sun-exposed distribution.
It is most common in white, young to middle-aged women.
Often a sudden eruption occurs after sun exposure, but this gradually progresses to involve more skin over time.
Lesions occur on the upper trunk, nape of the neck, upper back and shoulders, extensor arms, face, and dorsal hands.
Internal involvement is limited and less severe than in SLE; it may not be notable at all.
Individual lesions may last for months.
This condition tends to be chronic and recurrent, with flaring during spring and summer months or during times of high sun exposure.
Drug-associated SCLE is the most common drug-induced lupus variant. Patients are often older than patients with idiopathic SCLE. It is similar to idiopathic SCLE clinically and serologicially but more frequently also involves the legs, and may have a bullous presentation. Arthritis, serositis, or major organ involvement is usually absent. Development ranges from 4 to 20 weeks after drug initiation. Some medications associated with SCLE include calcium channel blockers, angiotensin-converting enzyme inhibitors, thiazide diuretics, terbinafine, statins, tamoxifen, proton pump inhibitors, the antidepressant bupropion, the nonsteroidal anti-inflammatory drugs piroxicam and naproxen, interferon-beta, leflunomide, docetaxel, and anti-TNF medications.
There are two patterns: papulosquamous and annular polycyclic. The annular polycyclic lesions may have little scaling.
Lesions occur most often on the sun-exposed trunk; they are rarely seen below the waist.
Subtle gray hypopigmentation and telangiectasia are seen in the center of annular lesions; this becomes more obvious as lesions resolve. Hypopigmentation fades in several months, but the telangiectasia persists.
Follicular plugging, adherent hyperkeratosis, scarring, and dermal atrophy are not prominent features; these are more typical of discoid lesions.
Other signs include photosensitivity in 70% to 90%, periungual telangiectasia, CCLE, and necrotizing vasculitis.
Other variants of SCLE are neonatal lupus erythematosus, complement C2−deficient lupus erythematosus−like syndrome, drug-induced SCLE, and tumid lupus.
The ANA titer is elevated in 50% to 72% of cases.
Anti-Ro (anti−SS-A) antibody titer is elevated in 50% to 100% of cases. Patients with Ro/SS-A antibodies are at increased risk for new autoimmune diseases and drug-induced SCLE.
Anti-La (anti−SS-B) is positive in fewer patients; it most frequently coexists with anti-Ro (anti−SS-A) and is usually not present as a unique antibody.
Leukopenia is present in 25% to 50% of patients with SCLE.
Drug eruptions, or drug-induced lupus
Dermatomyositis
Secondary syphilis
Psoriasis
Cutaneous T-cell lymphoma
Seborrheic dermatitis
Tinea corporis
Patients with SCLE do not meet criteria for SLE, although involvement is not strictly cutaneous; some have renal or neurologic involvement and other systemic manifestations, such as fatigue and arthralgia. Hematologic involvement with leukopenia, decreased complement levels, and lymphopenia may also occur. The overall prognosis is better for SCLE than for lupus erythematosus.
Mothers with Ro antibodies may transmit neonatal lupus; the incidence in one study was 7.6%.


Neonatal lupus is acquired through transplacental maternal autoantibodies, typically to Ro/SS-A. The infant presents with cutaneous lupus lesions at birth or within days to months after birth, or congenital heart block. Thrombocytopenia is present in 10% to 20%.
Neonatal lupus skin lesions are annular plaques with overlying fine scale; they resolve spontaneously in weeks to months and may leave residual telangiectasias, mild atrophy, or pigmentary alteration. Lesional skin biopsy shows typical lupus erythematosus changes, and Ro antibodies are present in most affected neonates and their mothers.
Complete irreversible heart block occurs in roughly half of infants with neonatal lupus and can cause significant morbidity and mortality. A pacemaker is required for complete heart block.
A mother of a child with neonatal lupus is at high risk for having other children similarly affected; early prenatal counseling and high-risk obstetric expertise are advised.
Sun-protective measures, including broad-spectrum sunscreen, are an essential element of treatment for neonatal lupus. Low-potency topical steroid or the topical immune modulators tacrolimus or pimecrolimus may hasten lesion resolution.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here