Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Congenital spine deformity originates in early gestation, with multiple combinations of failure of formation, segmentation, and other anomalies possible.
Associated vertebral, intraspinal, and visceral anomalies are common and may be clinically hidden. Screening for renal, cardiac, and intraspinal anomalies by ultrasound or magnetic resonance imaging is indicated.
Congenital spinal deformities are an “early-onset spine deformity” with risk of thoracic insufficiency syndrome from a short spine or distorted thorax. Early fusion or instrumentation may produce untoward spinal shortening, contributing to an already inherently short spine.
Congenital spinal deformities are most progressive with rapid growth during the first several years of life and during the early adolescent growth spurt. They may remain stable during the steady growth period of childhood, creating a false sense of stability.
Progressive deformity may be subtle and gradual. When measuring serial radiographs, identical landmarks should be compared, and all available images over time measured.
Progressive deformity in a normally segmented portion of the spine adjacent to congenital scoliosis may be attributed to spinal cord tethering.
Global spinal deformity as well as local deformity should be assessed. Global deformity or secondary deformity may be of greater consequence than the local congenital deformity.
Surgical interventions are individualized according to the deformity and progression.
Common contemporary options include convex in situ fusion, hemivertebra or wedge resection, and expandable growth-friendly instrumentation, as well as definitive instrumentation and fusion with or without osteotomies closer to maturity.
Congenital spinal deformity carries a higher risk of perioperative neurological loss.
Congenital scoliosis and congenital spinal deformity are relatively uncommon, encompassing a wide spectrum of deformity. The overall incidence of congenital spinal anomalies is not clear, as many anomalies go undetected and are of no clinical significance. Because the origin of congenital deformity is in early gestation, associated spinal and other organ anomalies formed at the same time are common. Unlike idiopathic scoliosis and kyphosis, nonsurgical treatments such as exercise or bracing are rarely effective in treating congenital spinal deformity. As with any early-onset spine deformity there is the potential for significant compromise of pulmonary function and overall musculoskeletal functioning. The natural history of congenital spinal deformity is highly variable, depending upon the balance of growth. Surgical treatments are of necessity individualized to minimize final deformity and maximize function at maturity.
The vertebral malformations in congenital spinal deformity may present as a localized finding, may appear as multiple vertebral malformations, or may appear in association with recognized genetic syndromes ( Table 19.1 ). The origin of congenital spinal malformations is acknowledged to occur approximately in the first 6 to 8 weeks of gestation when segmentation occurs. Abnormalities in the normal sequence of embryological events associated with the segmentation clock are generally felt to be responsible for vertebral segmentation errors, , with presumed NOTCH , HOX , or other gene dysfunction. Several congenital spine deformities, such as Klippel–Feil , and both spondylocostal dysplasia (SCD) and spondylothoracic dysplasia (STD), have demonstrated familial inheritance and associations with identified chromosomal abnormalities. Seki found abnormal expression of Hox genes in a rat congenital scoliosis model, whereas SCD has been associated with abnormalities in the DLL3, MESP2, TBX6, HES7, RIPPLY2, DMRT2, and LFNG genes. Multiple genetic syndromes, such as Allageile, DiGeorge, Goldenhar, or Cornelia DeLange syndromes with identified inheritance patterns and gene abnormalities, are also commonly accompanied by congenital vertebral anomalies. However, a majority of simple congenital vertebral anomalies are sporadic, isolated occurrences, without a specific genetic or syndromic origin. Known environmental factors contributing to congenital spine deformity in humans and animals include exposure to carbon monoxide and hypoxia, , hyperthermia, maternal diabetes, and ingestion of valproate. The incidence or prevalence of congenital spinal deformities in the general population is difficult to discern, as many are asymptomatic and go undetected, and criteria vary, potentially including transitional lumbosacral anatomy or other minor anomalies like spina bifida occulta. Passias documented the occurrence of congenital spinal anomalies in a national hospital database, noting 0.09 hemivertebrae and 0.04 Klippel–Feil deformities per 1000 patients. Shands estimated a congenital vertebral incidence of 0.5 to 1 per 1000 based on a survey of chest x-rays.
| Syndrome | Clinical features | Vertebral anomalies | Responsible gene(s) |
|---|---|---|---|
| Alagille | Pulmonic stenosis, cholestasis, dysmorphic facies | Variable | JAGGED1, NOTCH2 |
| (Jarcho–Levin) Spondylocostal and spondylothoracic dysostosis |
Short trunk, thoracic vertebral, and rib malformations and fusions | Extensive, mixed thoracic vertebral anomalies | DLL3, MESP2, TBX6, HES7, RIPPLY2, DMRT2, LFNG |
| Klippel–Feil | Short neck, low posterior hairline, multiple subtype classifications | Multiple cervical and upper thoracic fusions | PAXl, GDF6 |
| Goldenhar | Hemifacial macrosomia, epibulbar dermoids | Variable | Multiple, variable |
| Vacterl | Variable combinations of vertebral malformations, anal atresia, cardiac malformations, tracheoesophageal fistula, renal, and radial anomalies, and limb defects | Variable | |
| DiGeorge (Velocardiofacial syndrome) | Cardiac malformation, cleft palate, hearing loss, renal problems, autoimmune disorders, hypocalcemia, hypoparathyroidism | Variable C1C2 dysmorphism |
Microdeletion, 22q11.2, 10p14–p13 |
| Kabuki | Facial features, hypotonia, other abnormalities | Sagittal clefts, hemivertebrae, butterfly vertebrae | MLL2, KMT2D , KDM6A |
| Charge | Coloboma, heart defects, choanal atresia or cleft palate, growth retardation, genital abnormalities, and ear abnormalities | Cervical anomalies, instability | CHD7 |
| Cornelia DeLange | Short stature, developmental delay, short arms, hands, and digits, hypertrichosis, microcephaly, distinctive facial features, hearing loss | Cervical anomalies, instability, stenosis | DES, SMC1A, SMC3, NIPBL, RAD21, HDAC8 |
The spectrum of congenital spinal anomalies includes the entire spine from occipitocervical anomalies to Klippel–Feil syndrome, STD and SCD, congenital spinal dislocation and dysgenesis, and lumbar or sacral agenesis, as well as spinal dysrhaphic anomalies including spina bifida and myelodysplasia ( Fig. 19.1 ). This chapter will concentrate on the more common congenital deformities: congenital scoliosis and kyphosis.
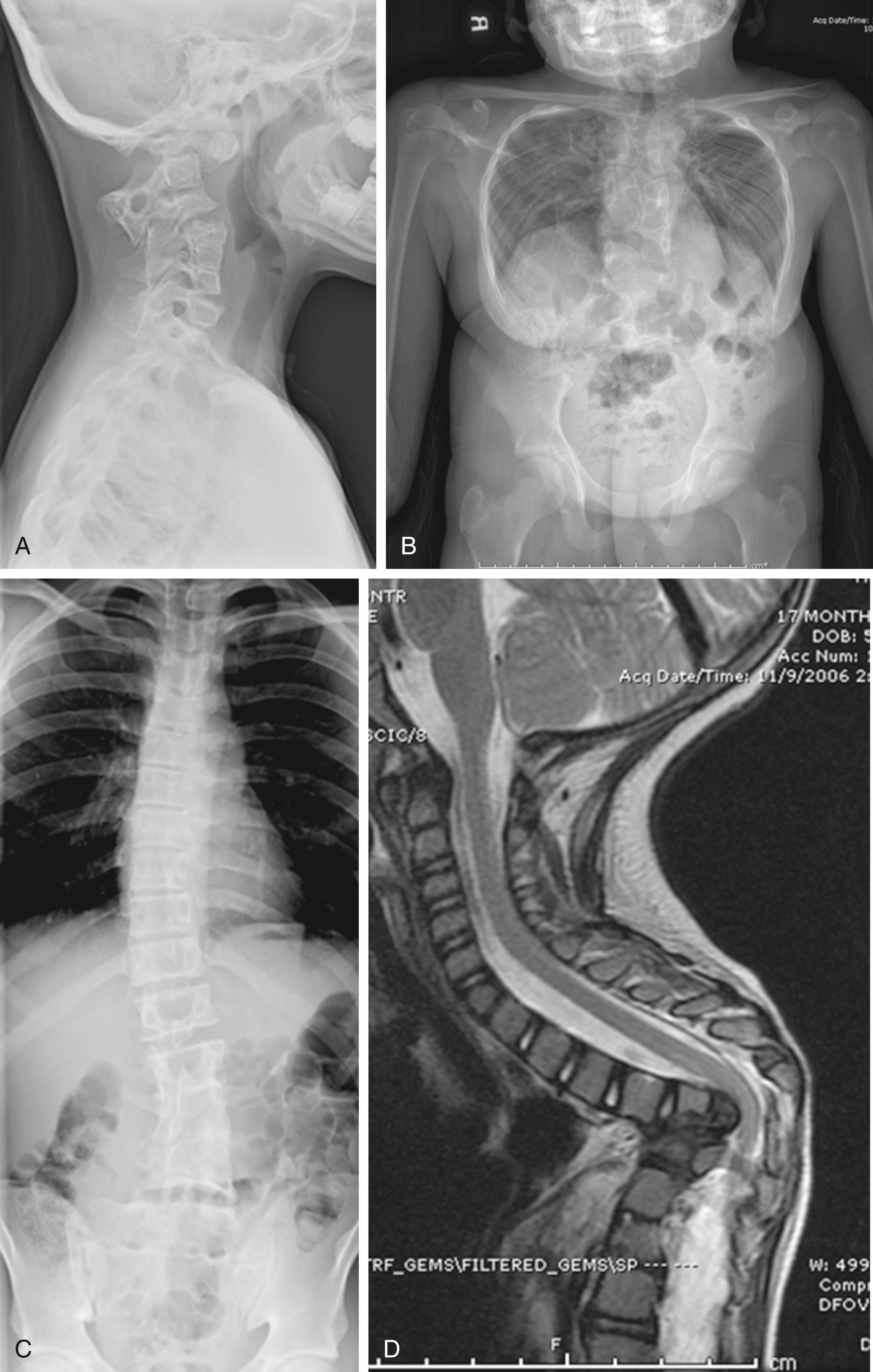
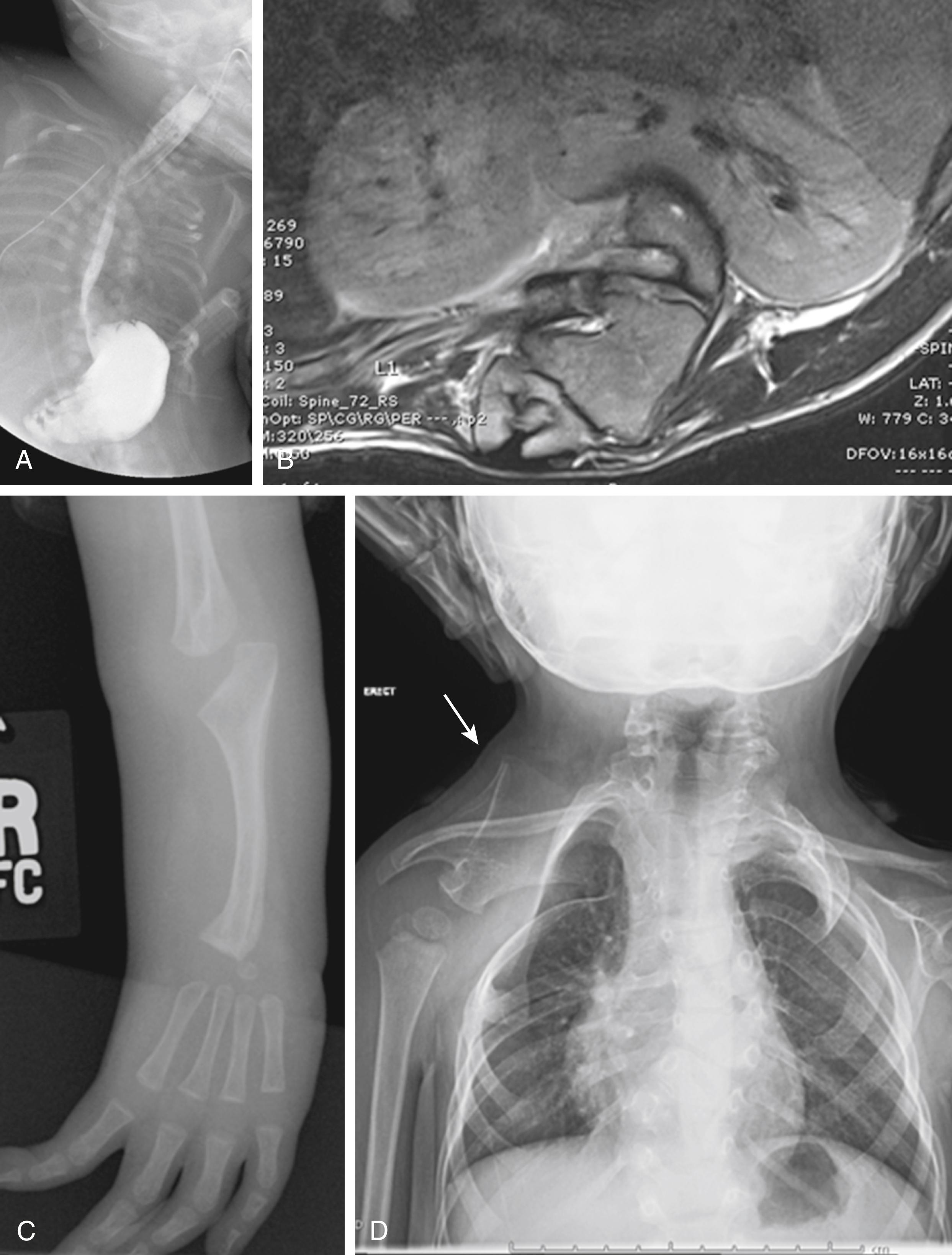
As the spine is developed and segmented during gestation, multiple other organ systems are formed concurrently. The association between congenital spine anomalies and other visceral, neural, and musculoskeletal anomalies is well established ( Fig. 19.2 ). Furdock found among 305 outpatients with congenital scoliosis that 84% had at least one organ defect: urogenital in 39%, cardiac in 54%, and both cardiac and urogenital in 12%. In hospitalized pediatric patients, Passias noted a wide range of visceral anomalies depending upon the type of congenital spine anomaly, with 63.2% of hemivertebra patients and 35.2% of Klippel–Feil patients showing concurrent anomalies. As a group, all spine anomalies had a rate of 6.5 cardiac, 5.5 urinary, 4.4 gastrointestinal, 2.1 genital, and 5.5 other syndrome per 1000 patients. The VACTERL association includes vertebral, anal, cardiac, tracheoesophageal fistula, renal, and limb (radial aplasia) anomalies and illustrates the spectrum of possible associations. Any congenital spinal anomaly carries a risk of these associations. Although many of these associated anomalies are immediately apparent, a diligent search for unrecognized renal, cardiac, and hearing anomalies is indicated, as these may remain clinically silent, yet be of great long-term significance ( Table 19.2 ). A screening renal ultrasound will detect major renal anomalies, including hydronephrosis or hydroureter, which might have otherwise gone undetected. Any preoperative evaluation should include a cardiac echo. Hearing deficits are sometimes not recognized early. Other musculoskeletal anomalies, such as Sprengel deformity or rib fusions, are more readily apparent on examination or plain x-ray.
| Anomaly | Screening suggested |
|---|---|
| Cardiac – congenital heart disease | Echo |
| Renal/genitourinary – hydronephrosis, obstruction | Renal ultrasound |
| Auditory | Infant hearing test |
Instraspinal anomalies
|
Spine ultrasound in first 6–8 weeks infancy Magnetic resonance imaging for neuroabnormalities or preoperatively, or when in doubt |
| Hematological | Only with thrombocytopenia with absent radius (TAR) |
Vertebral – other, remote
|
C-spine x-ray to include occiput. Flexion/Extension (F/E) if anomalous |
Musculoskeletal
|
Physical exam, chest x-ray |
| Syndromes (see Table 19.1 ) | Genetics consult |
Intraspinal neuraxis anomalies are common in congenital spinal deformity ( Fig. 19.3 ). Prahinski noted a 30% incidence, whereas McMaster reported an incidence of 18.3%, including diastematomyelia, neurenteric, epidermoid, and dermoid cysts, teratoma, lipofibroma, absence of nerve roots, fibrous bands, and tight filum terminale. Intraspinal anomalies occurred in 52% of cases with a unilateral unsegmented bar and contralateral hemivertebra. Anomalies such as diplomyelia, tethered spinal cord, or intraspinal lipoma are of enough significance to warrant screening. If seen before 6 or 8 weeks of age, a spinal ultrasound is easily performed in infants and will detect major intraspinal anomalies, such as low conus, lipoma, or major anomalies. There is general agreement that magnetic resonance imaging (MRI) is needed as part of preoperative evaluation, if neurological abnormalities are noted, or if there are other suggestions of likely intraspinal abnormalities, such as skin dimpling, a hairy patch or hyperpigmentation, or spinal dysgenesis, or dislocation on x-ray. Progressive curvature, particularly in a normally segmented part of the spine, may indicate a tethered spinal cord and is a clear indication for MRI. Some authorities suggest that MRI be performed for any instance of congenital spinal deformity. MRI can be performed easily in older children, but for the younger child MRI usually necessitates sedation or even general anesthesia. The “feed and wrap” technique may obviate the need for sedation in infants. In children too young for MRI without sedation, and who have no neurological abnormality or other indication for MRI, it may be reasonable to observe until an older age when MRI can be performed more easily ( Table 19.3 ). If not already done, radiographs of the entire spine are indicated to search for any congenital anomalies remote to the area of interest, to ensure that significant congenital vertebral anomalies like craniocervical anomalies with instability are not overlooked.

| Clinical Situation | MRI? |
|---|---|
| Normal spine ultrasound in infancy, neuro examination normal | Magnetic resonance imaging (MRI) preoperative or if neurological change or progressive curve or signs of tethering |
| Infant—Congenital spine abnormality, stable, neuro examination normal, no sign of tethering | Spine ultrasound if less than 6–8 weeks of age Consider screening MRI with feed and wrap technique MRI preop or if neurological change or progressive curve or signs of tethering, otherwise defer screening MRI to later in childhood |
Child—Congenital spine abnormality, stable, neurological examination normal, no sign of tethering
|
MRI in all—suggested by some authorities
|
| Progressive deformity in normally segmented section of spine remote from congenital anomaly | MRI needed to rule out tethering |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here