Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter describes and discusses disorders caused by neurologic disease that affect the adult and adolescent foot and ankle. It is divided into three sections: general considerations , congenital neurologic disorders , and acquired neurologic disorders .
Both congenital and acquired neurologic conditions can profoundly impact the shape and function of the lower extremity. Accurate diagnosis is vital for determining prognosis, likelihood of progression of the underlying condition, and selection of proper treatment alternatives. Each point in decision making and patient/family counseling requires recognition of the specific neurologic disease.
All neurologic abnormalities manifest with an imbalance of available functional musculature regardless of timing and etiology. This section will describe considerations allowing the individual to be assessed in the context of their disease and help the reader develop a framework upon which to assess patients with neurologic disease in general.
It is fundamental to appreciate the goals of treatment before determining a care plan for a given patient, and in no area of orthopaedic medicine is this more apparent than in the management of patients affected by neurologic disease. These patients deserve an accurate diagnosis and discussion of disease prognosis and treatment alternatives, which must be accompanied by a recognition of their functional attributes and cognition status and an acknowledgment of the context of their disease and the family environment experienced by that individual. For instance, the spectrum of “ambulatory goals” is familiar to providers but may be an altogether novel concept to parents of a child recently diagnosed with muscular dystrophy or an adolescent male with newly recognized Charcot-Marie-Tooth (CMT) disease.
A team of medical providers often collaborates to determine care for patients with neurologic disease. Consultation with neurologists, endocrinologists, physical medicine and rehabilitation specialists, geneticists, pediatricians, and/or physical therapists is common.
The age of the patient at the time of disease manifestation or onset is of fundamental importance in understanding how to assess and treat the patient. Neurologic conditions manifesting after skeletal maturity do not typically have the same adverse effects on modeling of the foot and ankle osteology as do congenital disorders. Neurologic disorders result from a variety of etiologies, which can be static (e.g., cerebral palsy) or progressive (e.g., CMT disease). A static neurologic disorder in a child can lead to a progressive deformity with growth. Some of these conditions have a significant sensory component as well as affecting motor function. Acquired neurologic disorders, such as cerebrovascular accident (CVA; stroke), traumatic brain injury (TBI), and spinal cord injury, primarily involve the central nervous system (CNS). The treatment of spasticity is the primary concern in these patients. However, these three etiologies differ in age of occurrence and variable neurologic recovery time, and societal impact may be markedly different in these different patient groups.
Orthopaedic surgeons must apply a functional understanding of the limitations of the patient. Often, these limitations follow recognizable patterns of neurologic dysfunction. Lower motor neuron disorders usually present with decreased tone, loss of normal reflexes, weakness, and significant muscle atrophy. A common progressive neuropathy affecting the lower motor neurons is CMT disease. Other lower motor neuron disorders include poliomyelitis, myelodysplasia, and peripheral nerve injury. Upper motor neuron disorder s classically manifest with increased tone, enhanced reflexes, long-tract signs, and mild atrophy. These disorders include cerebral palsy, CVA, and trauma to the brain and spinal cord. Spasticity and weakness or paralysis in these disorders leads to muscle imbalance and deformity. Sensory impairment is an important consideration in the treatment of all neurologically impaired patients. Diminished sensation of the foot and ankle adds complexity to the treatment and risk factors for these patients. Sensory impairment occurs in lower motor neuron (peripheral nerve) disorders, except those involving the anterior horn cells (e.g., poliomyelitis) and the neuromuscular junction and the muscle itself (e.g., muscular dystrophy). In upper motor neuron lesions, difficulty in processing sensory input can lead to clinical problems similar to the insensate foot.
Accurate diagnosis is necessary for optimal treatment. Without a proper diagnosis, there is a risk of pursuing unachievable goals or failing to achieve significant functional milestones in a capable patient. A basic understanding of the distinction between upper and lower motor neuron disorders is important. In addition, the surgeon must understand the characteristics of the disease being treated—specifically, whether the disorder is static or progressive and has motor or sensory components, or both. It is also important to identify any potential genetic component to the disease so that timely counseling can be made available to the patient and his or her family. Basic scientific advances constantly add to the appreciation of the complexity of the diversity of these conditions. For example, classic phenotypic descriptions of conditions such as “type I CMT disease” are now recognized as a manifestation of multiple different gene mutations.
Although this discussion is focused on the foot and ankle, it is important for the physician to evaluate the lower extremities in their entirety. Limb length inequality, rotational and angular misalignment, and/or contractures and weakness around the knee and hip will significantly affect the functional capacity of the patient. Ankle instability in patients with proximal muscle wasting conditions is not uncommon, and long periods of recuperation should be avoided in these patients because functional proximal losses in strength may be permanent in those patients. If a deformity around the knee is significant, addressing that deformity before positioning a foot or ankle fusion is essential for a properly aligned limb. In general, it is best to address all the concerns about the lower extremity and the foot and ankle at the same time or work from proximal to distal in the lower extremity if concomitant surgery is not feasible.
Neurologically driven foot and ankle abnormalities seldom occur in isolation. Typically, systemic problems are also exhibited in these patients. Two particularly important conditions of which the orthopaedic provider should be cognizant include preexisting arthritis and vascular insufficiency of the lower extremity. Nutritional abnormalities are also commonly problematic. Poor protein reserves are common in patients with brain impairment by stroke or trauma. Not uncommon in many parts of the world, but especially the United States, obesity is often a comorbidity in patients suffering from neurologic disease. Directed counseling of patients at risk for obesity is imperative. This is because limited muscular power will fail to maintain ambulatory capability in patients with significant weakness or balance impairment and this is made worse with obesity.
The variable time course and progressive nature of some neurologic conditions makes the timing of surgical intervention critical to its success, and care must be individualized. In patients with CVAs or brain and spinal cord injuries, early bracing or surgical intervention for limb stabilization during an acute phase of brain trauma may prevent the development of severe contractures. Loss of motion in a functional position may be advantageous in certain settings. Since neurologic recovery, as is inconsistently observed with peroneal nerve palsy after knee dislocation, is possible in some settings, early surgery in circumstances like this is unwise if motion can be maintained. Identifying the proper time for surgical intervention is still more art than science, and this is particularly evident in the timing of surgery in patients with known genetic conditions, such as CMT disease. Given the variability in penetrance and severity of the condition, the surgeon must follow patients over time to identify thresholds for intervention based on functional losses.
Swelling management is a particular challenge in those with neurologic impairment because abnormal muscular behavior does not maintain normal limb contraction and fluid maintenance. Postoperative swelling may be persistent and require the use of compressive garments and orthotic management. Incorporating the expertise of an occupational therapist who specializes in edema control can be a huge asset in the treatment plan after surgery.
The best way to manage deformity from neurologic injury or disease is prevention. In the early stages of neurologic disease, splinting and physical/occupational therapy can prevent or delay the fixed deformities caused by joint stiffness and weakness. Orthotic devices can be used to hold a position but cannot yield greater motion. In general, correction of structural deformities involves surgical soft tissue releases and osteotomies, but there is a role for medical therapy, including injectable medications for temporary muscular paralysis (i.e., botulinum toxin), to allow the maintenance of necessary arcs of motion.
After correcting the deformity, through surgery or medical means, the next goal is providing stability, and this can often be achieved with an orthotic device. In addition, thoughtfully considered tendon transfers can allow the maintenance of joint position in selected cases, but it is particularly important to understand the natural history of the specific neurologic condition to appreciate whether these are going to be effective over time. In some cases, collapse of the inherent architecture of the foot or ankle precludes successful management with an orthotic device, and the foot’s internal stability and plantigrade position can only be achieved by selective arthrodesis. The triple arthrodesis has an excellent record in poliomyelitis, but the results are mixed in the overall treatment of neuromuscular conditions, particularly those with a sensory component. Therefore it is best to consider the triple arthrodesis as a salvage procedure only and to limit the number of joints fused to achieve the desired result.
By careful patient selection and evaluation, a well-planned tendon transfer can achieve significant long-term functional improvement. Again, the surgeon must consider all the concerns regarding functional goals, cause, and accompanying deformities. In evaluating remaining muscle function, the surgeon must take into account the strength of the individual muscles (motors) around the foot and ankle, their phase of firing, and the volitional control of each. It is equally important to understand which muscles have lost their motor function or are contracted. An EMG can help determine this and should be completed prior to any definite surgery.
A simple guiding principle in planning therapeutic strategies for neurologic patients should be the conservation of energy during ambulation. Endurance and power are typically limited in these patients. Those problems are exacerbated by a lack of balance that may accompany central neurologic disease or impaired sensory function in lower motor neuron–affecting conditions. Through selective strengthening, bracing techniques, or surgical modification, enhanced functional capacity can be achieved if energy conservation is considered.
The review of congenital neurologic conditions will emphasize commonly observed conditions and provide perspective on disease penetrance and options for treatment.
Hereditary motor sensory neuropathies (HMSNs), frequently termed Charcot-Marie-Tooth (CMT) disease, comprise a large group of genetically distinct conditions with similar phenotypic presentations involving both sensory and motor function. Together they make up the most common degenerative disorders of the peripheral nerves. The basic distinction in hereditary polyneuropathies, including CMT, is between motor and sensory components. The hereditary sensory neuropathies (HSNs) have no motor component.
CMT disease is a complex group of more than 50 diseases that are inherited, progressive peripheral neuropathies thought to result from an abnormality of myelination. CMT is the most commonly inherited neuropathy and affects 2.8 million people worldwide and 1 in 2500 in the United States. As knowledge of the genetic basis of HMSN improves, classifications will evolve, though currently type I (hypertrophic) and type II (neuronal) remain useful classifications. Improved understanding of the molecular pathogenesis of the distinct genetic causes of HMSN may lead to systemic, holistic treatments. Until that time, the orthopaedic treatment involves education and management around the secondary effects of progressive peripheral neuropathy.
Type I HMSN is the classic and most common presentation of CMT disease. It typically presents in a patient’s second or third decade, and up to two thirds of these patients have a cavus foot by adulthood. The most common pattern of inheritance is autosomal dominant, although autosomal recessive and X-linked forms have also been reported. The disease is characterized by slow nerve conduction velocities, and it usually presents during the second decade of life. Genetic research has shown that the disease group demonstrates wide genetic heterogeneity, with 29 genes and more than 30 loci involved. Specific genetic sequences have been associated with a subset of type I patients, further defining this spectrum of disorders with future implications, not only diagnostic and prognostic but also potentially therapeutic. The majority of type I presentations have been linked to chromosome 17 and are designated CMT-1A. The most common abnormality identified on chromosome 17 is a duplication of a part of the PMP22 gene, but other variants have been identified.
Type II HMSN has a similar presentation but is less pronounced and usually appears later in life. In type II, the rate of impulse transfer is normal, but the magnitude of the impulse is decreased, as manifested by the loss of sensory- and motor nerve–evoked response amplitudes. Nerve conduction velocities are seldom slowed and, if so, only mildly.
The most common lower extremity presentation is bilateral progressive pes cavovarus deformities with leg weakness ( Fig. 19-1 ). Patients have a variety of complaints, including metatarsalgia, claw toes, tarsal prominence, and recurrent ankle sprains. In addition to the common presentation of the bilateral pes cavus, the orthopaedist must be aware of progressive weakness in the upper extremities, which usually occurs later than the foot findings. In general, CMT disease affects the longest nerves to the smallest muscles first, hence the symptomatic presentation of feet before hands. Hip dysplasia and scoliosis may also be present.

Because a majority of these are autosomal dominant diseases, a family history of similar foot problems is common. Despite this, the variability within families can be so great that individual family members can become symptomatic earlier or later and show significant disparity in the amount of disability secondary to the disorder.
The cavovarus presentation is the result of motor imbalance between consistent pairs of muscles around the foot and ankle ( Fig. 19-2 ). A common early finding is significant weakness of the tibialis anterior and peroneus longus muscles. As a result of tibialis anterior weakness, the first ray is plantar flexed by the stronger peroneus longus, creating a relative forefoot valgus. Compensation for this on weight bearing, considering the foot as a tripod, is a compensatory hindfoot varus. This hindfoot varus is further exaggerated by another muscle pair imbalance, the unopposed pull of the posterior tibialis muscle against the weakened peroneus brevis. Factoring in intrinsic wasting that causes an intrinsic minus (clawing) deformity at the metatarsophalangeal (MTP) and interphalangeal (IP) joints, the clinician sees the clinical presentation of hindfoot varus, to midfoot cavus and forefoot valgus, to clawing of the toes. Attempts by the extensor hallucis longus (EHL) and digitorum longus muscles to dorsiflex the foot further exacerbate toe clawing.

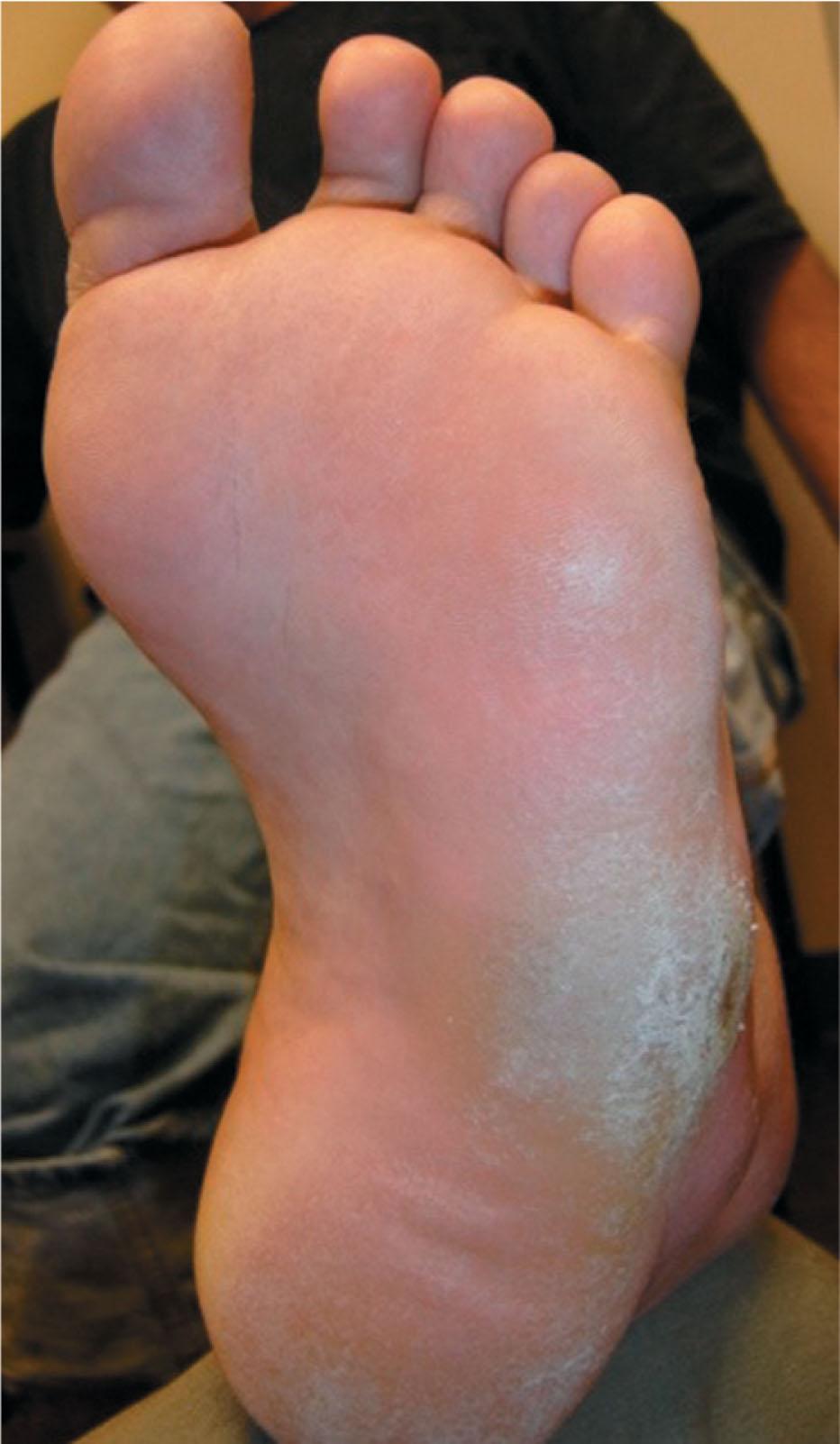
Although determining the pattern of muscle weakness is important to understanding the basic deformity of the cavovarus foot and for considering treatment alternatives, an equally important factor to remember is that CMT is also a sensory neuropathy. The early sensory changes can be subtle, primarily with loss of proprioceptive and vibratory sense. As with the different presentations of motor weakness, however, sensory presentations can vary greatly. Patients are less inclined to recognize or acknowledge the diminished sensation, but this loss limits their ability to balance properly. As with all other neuromuscular conditions leading to some level of diminished sensation of the foot and ankle, education on foot inspection is of fundamental importance. Patients must be taught to examine their feet carefully once they have significantly diminished sensation and must consistently protect their feet with appropriate footwear ( Fig. 19-3 ). Severe deformities and fusions are potentially problematic in the sensory-impaired foot and ankle.
A thorough neurologic evaluation of these patients is essential, starting with a careful motor examination. Weakness of the anterior tibialis and peroneus brevis muscles is commonly observed, but each muscle of the leg must be assessed as the relative strengths determine the options for management. The sensory impairment appears later and is usually not as severe. Up to 25% of patients do have significant sensory impairment. Vibration, two-point discrimination, and proprioception are the first factors to be affected.
In the patient with a cavovarus foot, standing examination shows the relative hindfoot varus, atrophy of the medial longitudinal arch, tarsal bossing, and some degree of toe clawing. In addition, the patient’s legs show significant atrophy below the knee ( Fig. 19-4 ). On the seated biomechanical examination, reduction of the foot into a neutral subtalar position allows the examiner to observe a relatively flexible hindfoot, indicating that the hindfoot varus is compensatory for a fixed forefoot valgus. The primary deformity of the forefoot is a plantar-flexed first ray, but over time, the second and third rays may be similarly depressed in relation to the foot’s lateral border. In the long-standing deformity, because of the relative parallelism between the long axis of the talus and the calcaneus (the varus position of the hindfoot is a result of the medial rotation of the calcaneus beneath the talus), limited dorsiflexion is present because of an abutment of the talar neck against the anterior tibia ( Fig. 19-5 ). The examiner must be sure to evaluate the motion of the talonavicular joint to determine if there is a mechanical block to abduction or a palpable prominence on the lateral aspect of the talar neck that precludes reduction of the midfoot to the hindfoot. When the patient is asked to ambulate, a combination of dorsiflexion weakness, fixed equinus, and difficulties with proprioception give a characteristic steppage gait.


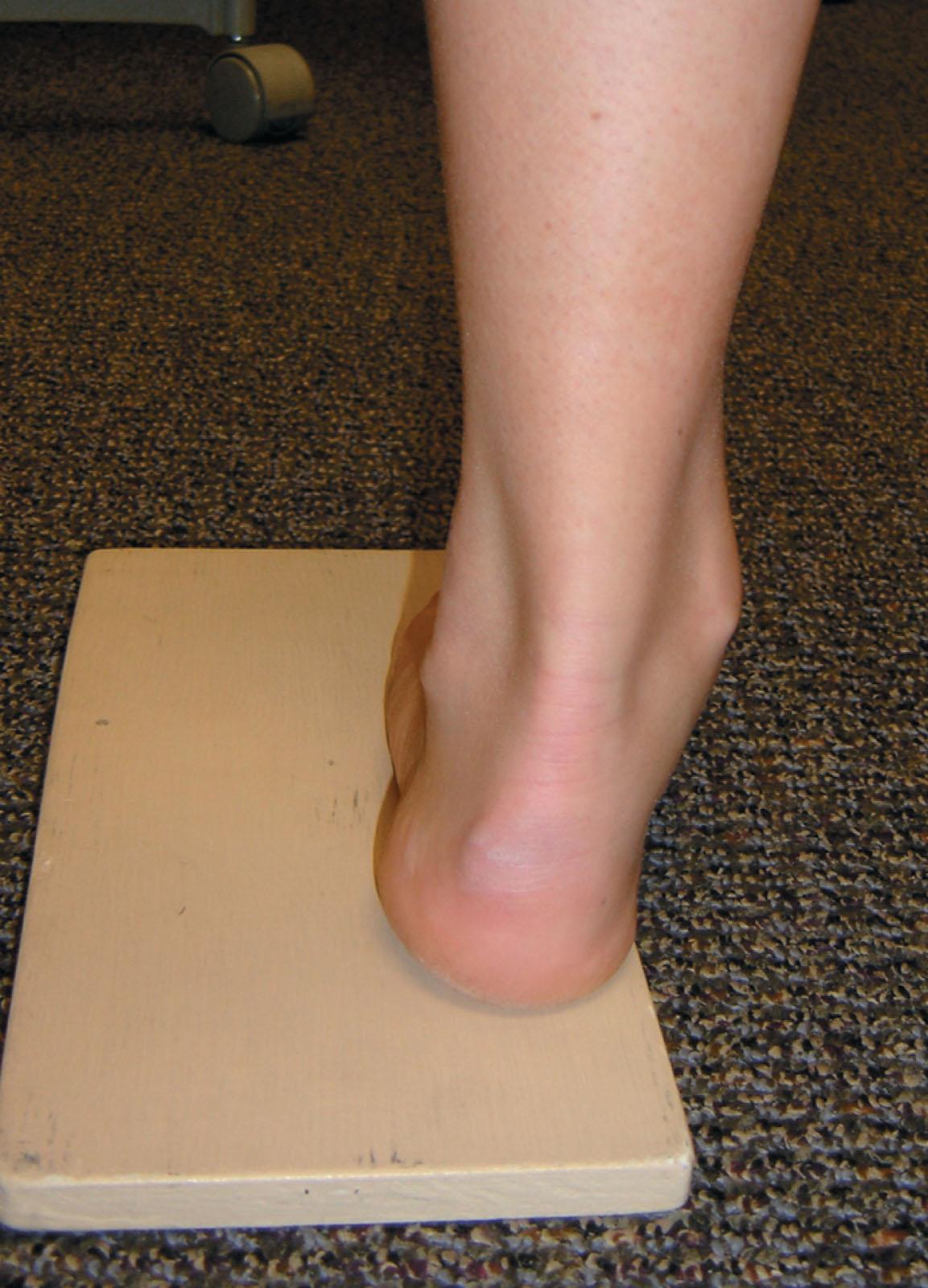
The Coleman block test remains the fundamental tool of clinical assessment of the patient with a cavus foot deformity. This classic test described by Coleman and Chesnut is useful in examining these patients clinically ( Fig. 19-6 ). The block test is performed by supporting the heel and the foot’s lateral border with a block but allowing the first ray to drop over the edge of the block, and the relative flexibility of the hindfoot is then evaluated. If the hindfoot corrects to neutral or slight valgus, the implication is a compensatory (i.e., “forefoot driven”) hindfoot varus, and that dorsiflexion of the plantar-flexed first ray will correct the hindfoot deformity. If the heel moves only slightly or fails to move at all, the hindfoot deformity is fixed and must be addressed directly, which usually demands a calcaneal osteotomy or hindfoot fusion procedure. This relative hindfoot rigidity, however, is not necessarily the end stage of an algorithm requiring triple arthrodesis.
Treatment begins with an accurate diagnosis, and in early stages, this might only require observation. Objective support for physical therapy has been reported in patients with CMT. For instance, physical therapy in a young child may improve early loss of motion. Orthotic management and shoe modification also have a role in the treatment of CMT disease and the cavovarus foot. In the foot with significant early involvement, an orthotic device may be used to hold the foot in a more normal position by allowing for plantar flexion of the first ray, with relative posting of the lateral forefoot. An additional lateral heel wedge can also be effective. Ankle–foot orthoses can be used to support the more involved leg and foot deformity, and many adult patients tolerate this for years. However, it is important to note that this may be only a temporary measure because the neuropathy and corresponding deformity will likely continue to progress.
Orthotic devices have a role in the adult patient who has substantial paralysis of the foot or significant footdrop. Orthoses may be used to accommodate foot deformity, protect the insensate foot, and to reduce some of the energy expenditure of a steppage gait. Orthoses can be used to some degree to prevent or delay deformity but cannot be used to correct rigid deformity. Severe and rigid deformities often make the use of an orthosis untenable, and surgery may be considered with the goal of creating a foot shape that allows an orthosis to be used to support ambulation.
Radiographic assessment is important in preoperative planning ( Fig. 19-7 ). A series of weight-bearing radiographs should be taken of both feet and ankles. Because of the severity of many of these deformities, particularly midfoot adductus, obtaining a good lateral view of the foot can be difficult. To obtain a true talar lateral view and a good assessment of the hindfoot, the axis of the medial and lateral malleoli should be parallel to the x-ray beam. This, however, makes the midfoot and forefoot difficult to assess, so a second lateral view may be necessary for a true lateral view of the forefoot. Studies of the ankle are important, particularly in long-standing severe varus hindfoot, in which case the lateral ligamentous structures may be compromised. Finally, because this is a sensory neuropathy, radiographic images are useful in the evaluation of possible Charcot neuroarthropathic changes in the foot and ankle.

Considerations for surgical treatment in these patients can be complex. The patient’s goals, expectations, and demands are the primary concern. Surgical treatment is usually complex and includes a combination of bony work as well as soft tissue balancing procedures in order to achieve a plantigrade foot to improve functional gait. See Chapter 30 for additional description of cavus foot correction.
In the patient who is considered a surgical candidate, the following three questions are important:
What is the motor status of each muscle around the foot and ankle?
Are the deformities fixed or flexible in terms of joint motion?
What degree of sensory impairment is present?
Complete plantar fascia release of the cavus foot is seldom performed in isolation but is commonly performed as an initial step during soft tissue and bone reconstruction in patients with CMT. In the earliest presentation of mild flexible cavus, the plantar fascia should not be released. The question arises: Can early soft tissue procedures (complete plantar fascia release) combined with tendon transfers (transfer of the peroneus longus to the lateral portion of the foot) alter the pathologic modeling of the immature foot? Are bony abnormalities observed in patients with CMT genetically driven or only the result of neuromotor imbalance?
The technique is as follows.
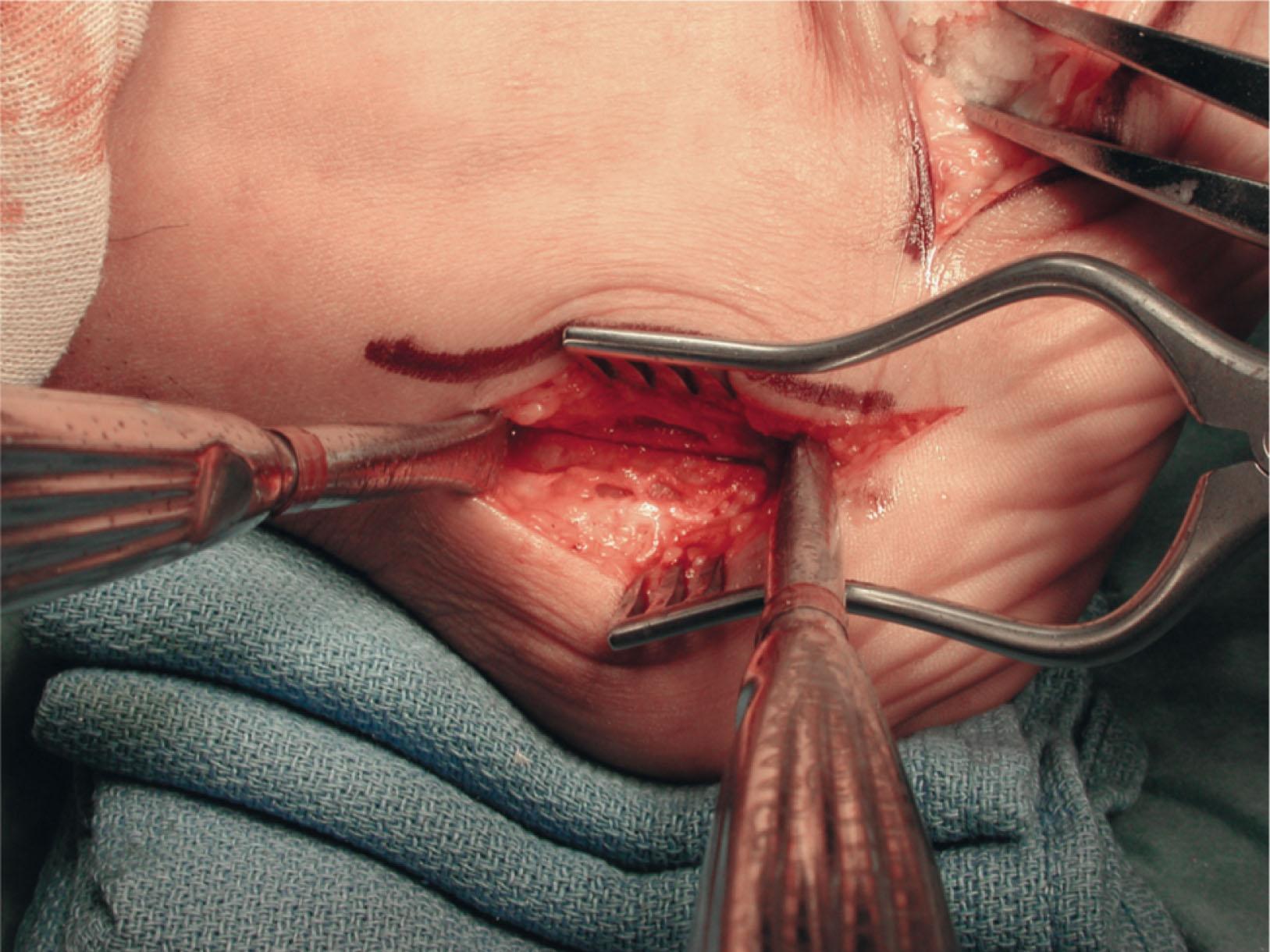
The plantar fascia is approached through a medial skin incision approximately 3 cm long at the junction between the plantar and medial skin, beginning at approximately the level of the medial tuberosity and extending distally.
Sharp dissection is done down to the abductor hallucis muscle. The plantar fascia is easily palpable by using a blunt Mayo scissor, and the tissue above and below the fascia is dissected off the fascia. In long-standing disease, the abductor muscle may show signs of significant atrophy and fibrosis.
Once the muscle is retracted, the thickened lateral fascia of the abductor halluces is encountered, which blends plantarly into the plantar fascia and intrinsic musculature. The leading edge of this fascia is found cephalad and carefully transected. A Freer elevator is placed behind this to protect the lateral plantar nerve, which is often visible during this approach. Care must be taken throughout this procedure to avoid manipulation of the nerve.
When the abductor fascia is out of the way, the lateral plantar nerve can be seen crossing over to the lateral portion of the foot with a somewhat distal trajectory. The intrinsic musculature and plantar fascia should be clearly visualized and then can be sharply divided.
Because this is seldom done as an isolated procedure and is often combined with a calcaneal osteotomy, it is important to ensure that the plantar fascia is completely released so that the tuberosity can easily be mobilized during deformity correction.
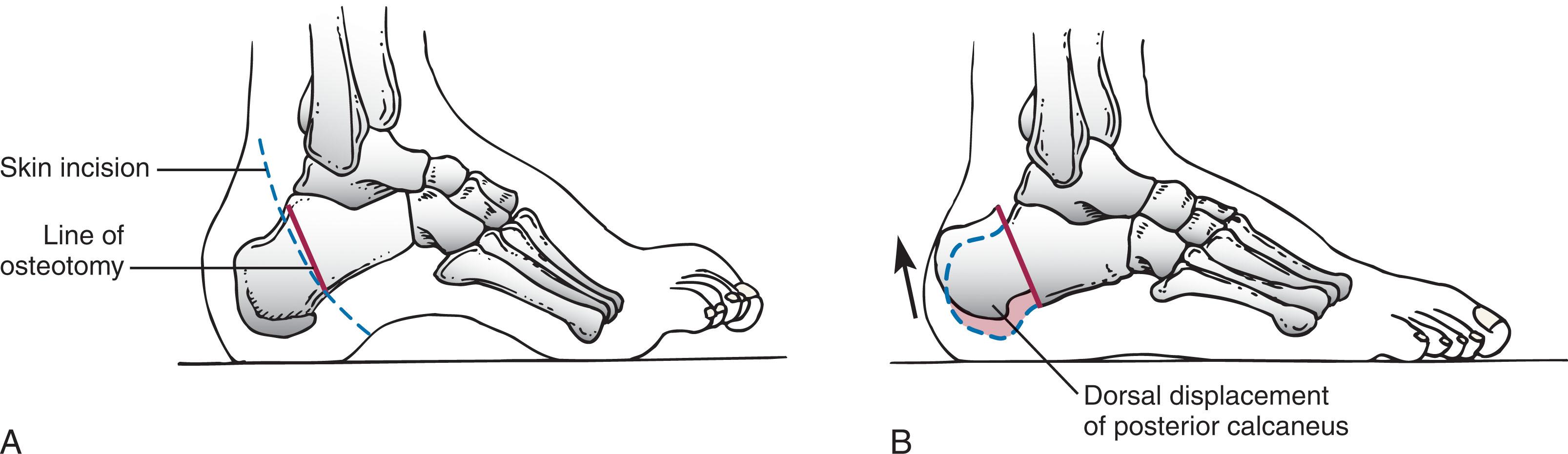
This procedure is performed to correct hindfoot varus alignment. If the Coleman block test shows some degree of correction but does not allow the hindfoot to correct to slight valgus, or if physical examination reveals well-preserved subtalar motion, a lateralizing calcaneal osteotomy is indicated ( Fig. 19-8 ). Preoperative standing radiographs of the ankle are important in addition to a careful examination because ankle instability may also be present in patients with long-standing deformities and can be confused with subtalar motion. Below, we will list both the traditional open approach and the minimally invasive approach. As more and more minimally invasive techniques are used, deformity correction surgery may become less invasive (and less morbid) with time.
The technique is as follows.
A curvilinear incision is made beginning 1 cm above the palpable calcaneal tuberosity between the Achilles tendon and the peroneal tendons. This curves down and ends at the junction between the lateral skin and plantar skin at the level of the peroneal sulcus.
Sharp dissection is performed straight down to bone because the skin incision is away from the major trunk of the sural nerve and the peroneal tendons.
A curved retractor is placed over the top of the tuberosity and another under the calcaneus. An oblique osteotomy is performed perpendicular to the lateral face of the calcaneus from the midportion of the tuberosity to approximately 1 cm past the weight-bearing portion of the calcaneus plantarly ( Fig. 19-9 ).
The primary displacement of the tuberosity fragment is laterally into a valgus position. The mid-axis of the tibia should fall just to the medial side of the midpoint of the calcaneal tuberosity.
The calcaneus may be shifted slightly cephalad (i.e., more vertical) to diminish the calcaneal pitch. Care must be taken not to shift this too far, or impingement of the neck of the talus into the anterior lip of the tibia will result.
By changing the obliquity of the osteotomy from more vertical to horizontal, more or less length can be obtained from the calcaneus as necessary, as opposed to more correction of the calcaneal pitch with the more vertical cut.
At times, the varus deformity is severe enough that it is necessary to remove a secondary wedge (Dwyer osteotomy) ( Fig. 19-10 ). This wedge is generally 1 cm wide or less laterally, tapering to emerge at the medial cortex, coincident with the first cut. The wedge is usually taken off the distal fragment of the calcaneus.
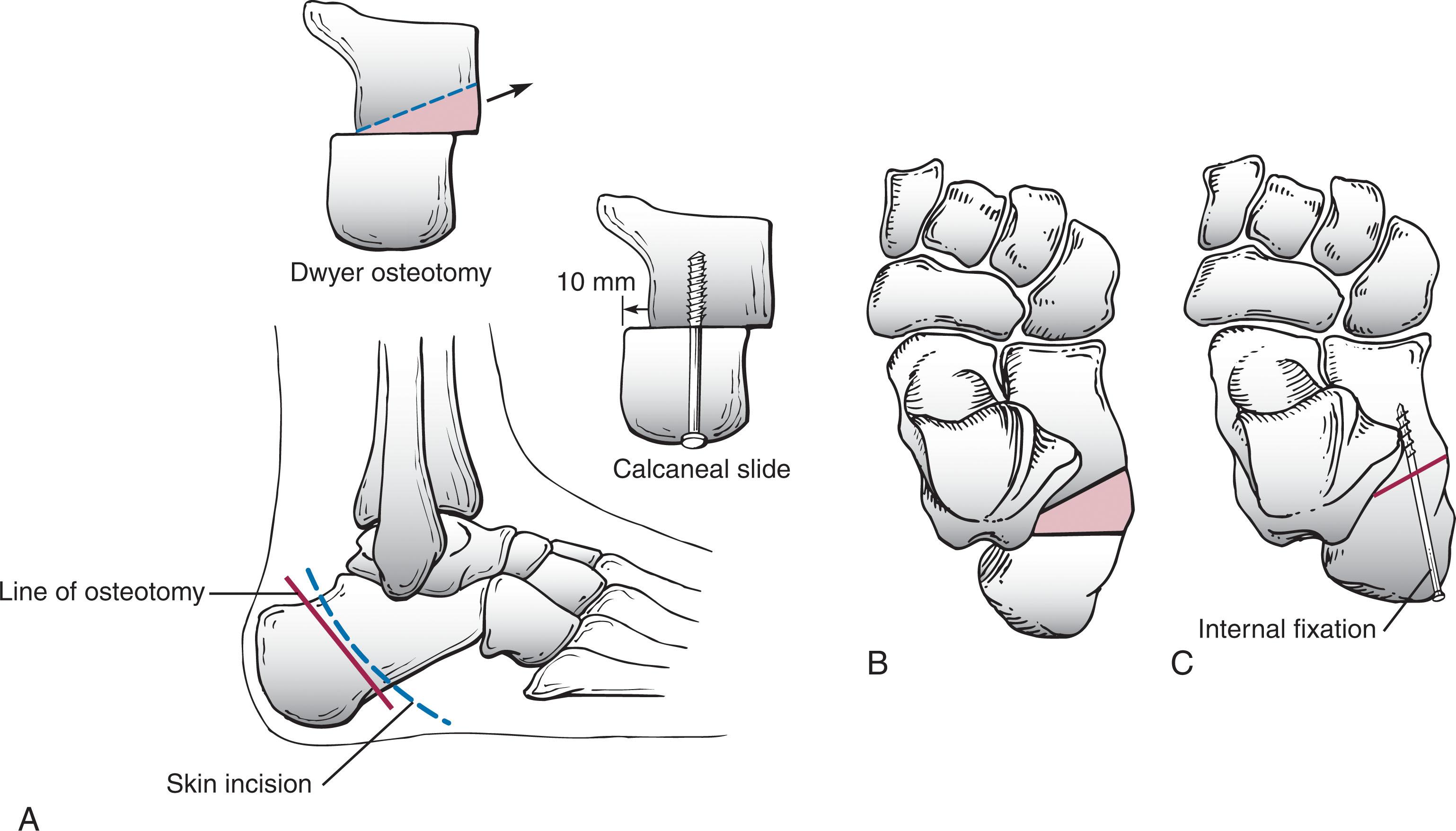
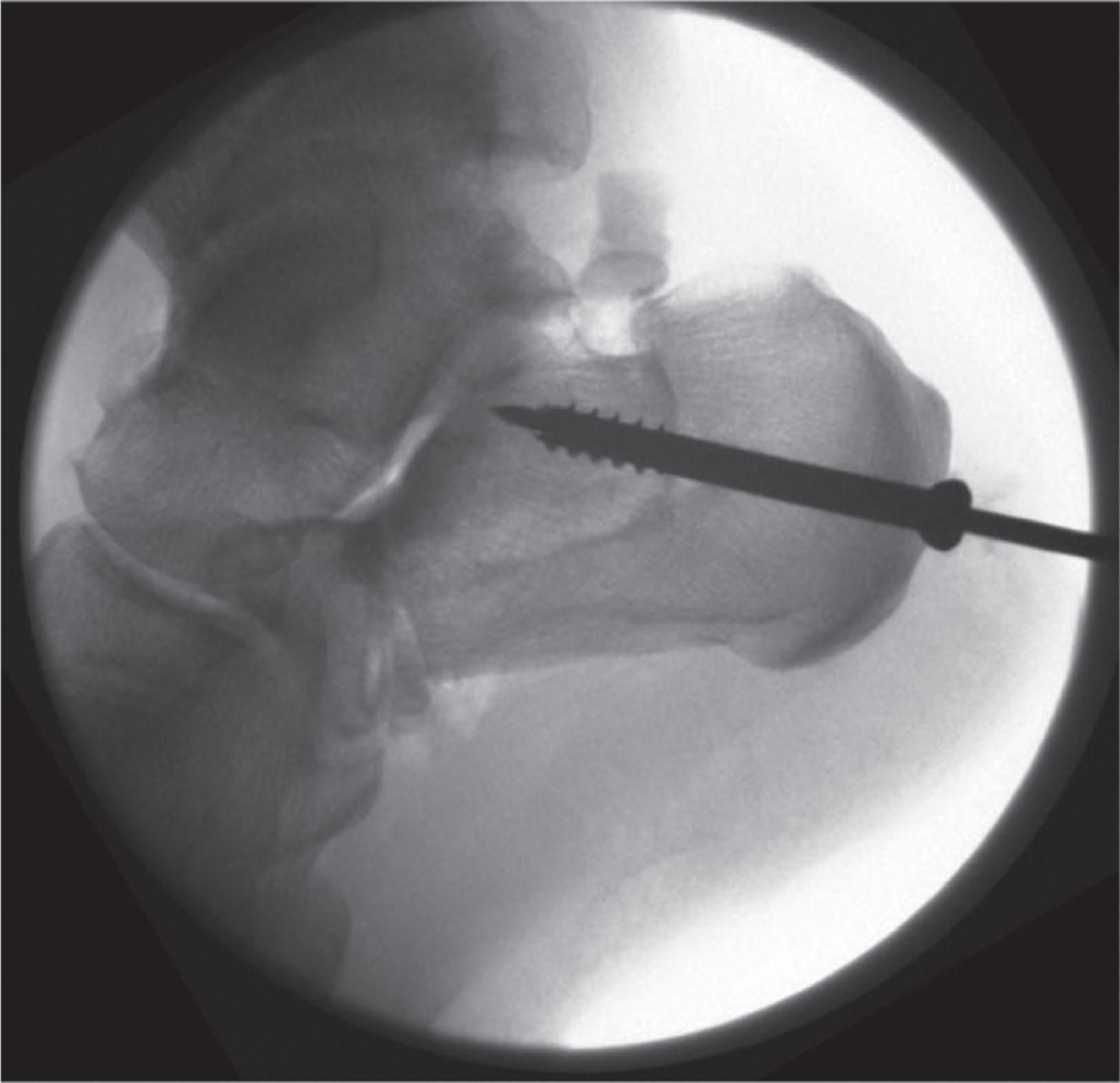
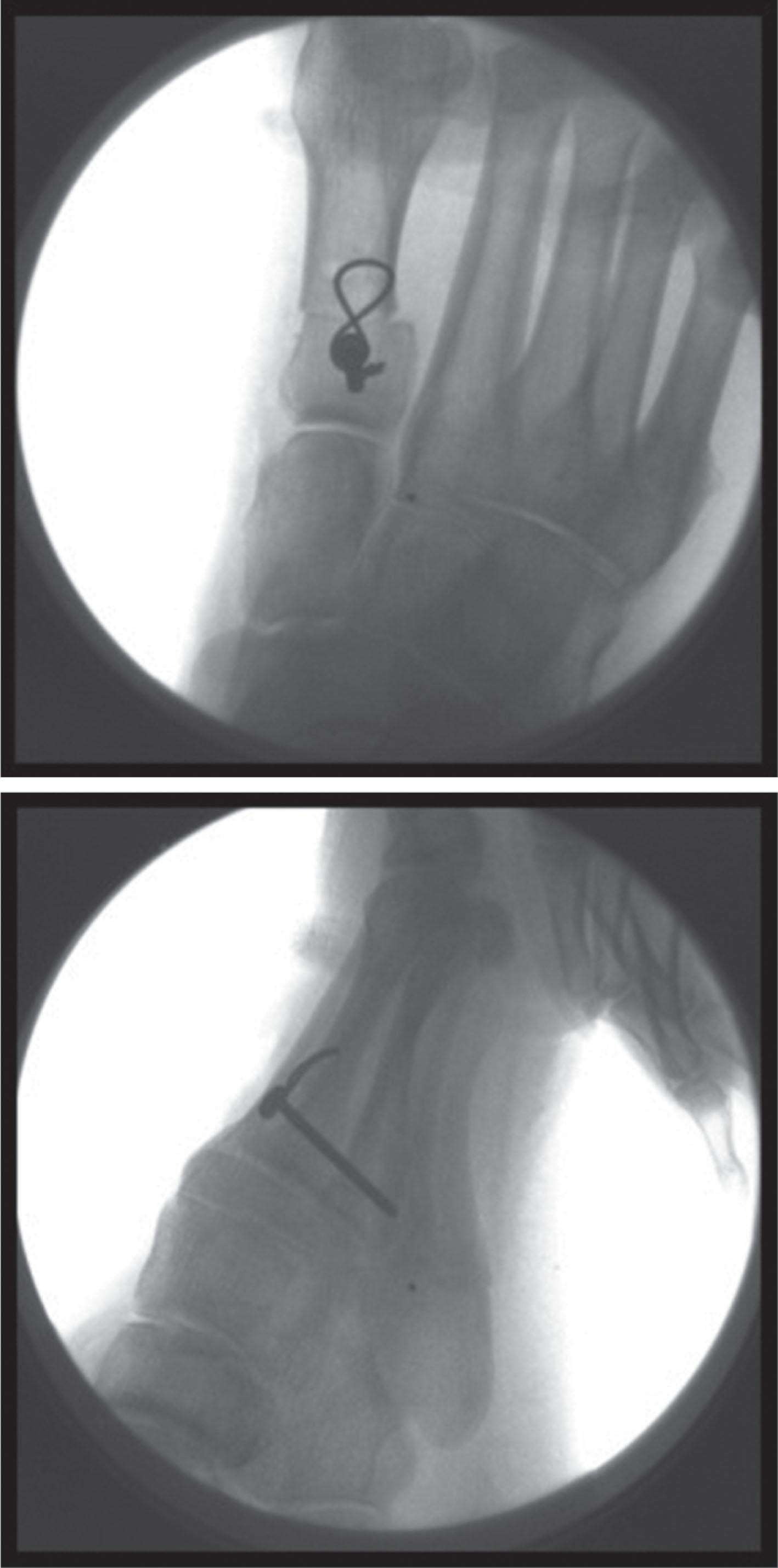
Fixation is accomplished with one or two screws inserted just off the heel pad posteriorly. Attempts should be made to keep the shaft–screw interface as far from the osteotomy as possible because this is the most common site of hardware failure. Both lateral and axial fluoroscopic image can be useful to confirm screw position.
In cases where a more significant deformity is addressed, a multiplanar osteotomy (“Malerba” type) may be used. This Z-shaped osteotomy has the potential advantage of allowing for translation, angulation, and rotation ( Fig. 19-11 ).
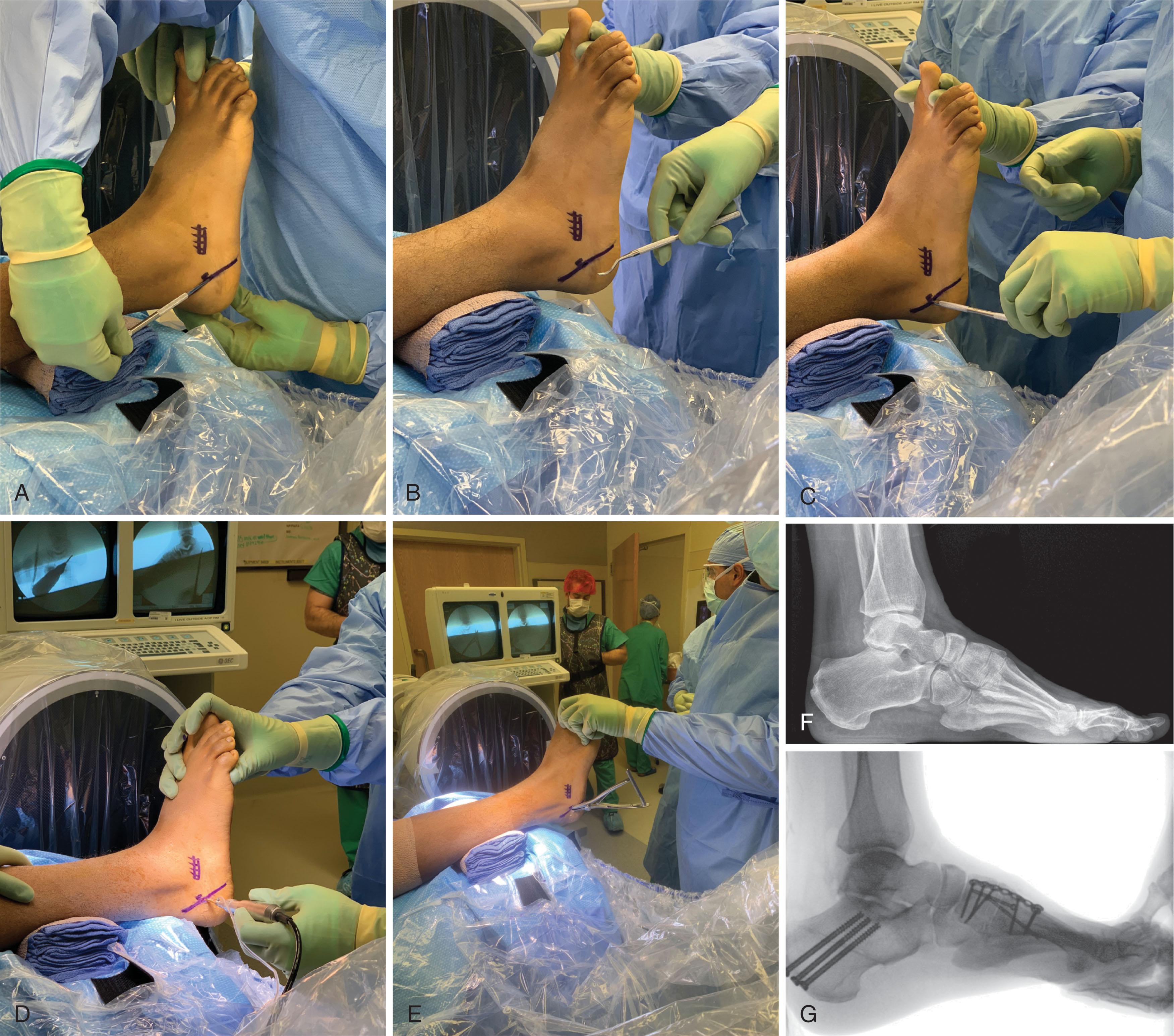
The technique is as follows.
An oblique line is made beginning 1 cm above the palpable calcaneal tuberosity between the Achilles tendon and the peroneal tendons. This is directed plantarly ending at the junction between the lateral skin and plantar skin at the level of the peroneal sulcus.
Fluoroscopy is used to ensure that the line drawn from the arc of motion of the osteotomy site is in good position.
Mark an area at the midpoint of the line where the small incision will be made for entry of the burr.
Make the incision and introduce the burr and check positioning on fluoroscopy.
Start the burr and with sweeping motions complete the osteotomy maintaining the burr in the predetermined plane, checking on fluoroscopy frequently. Make sure to irrigate to cool the burr as well.
Once the osteotomy is complete, you can use a lamina spreader to open the osteotomy site showing the cut is complete.
After translating the osteotomy laterally, fix with a percutaneously placed partially threaded screw from the posterior calcaneus.
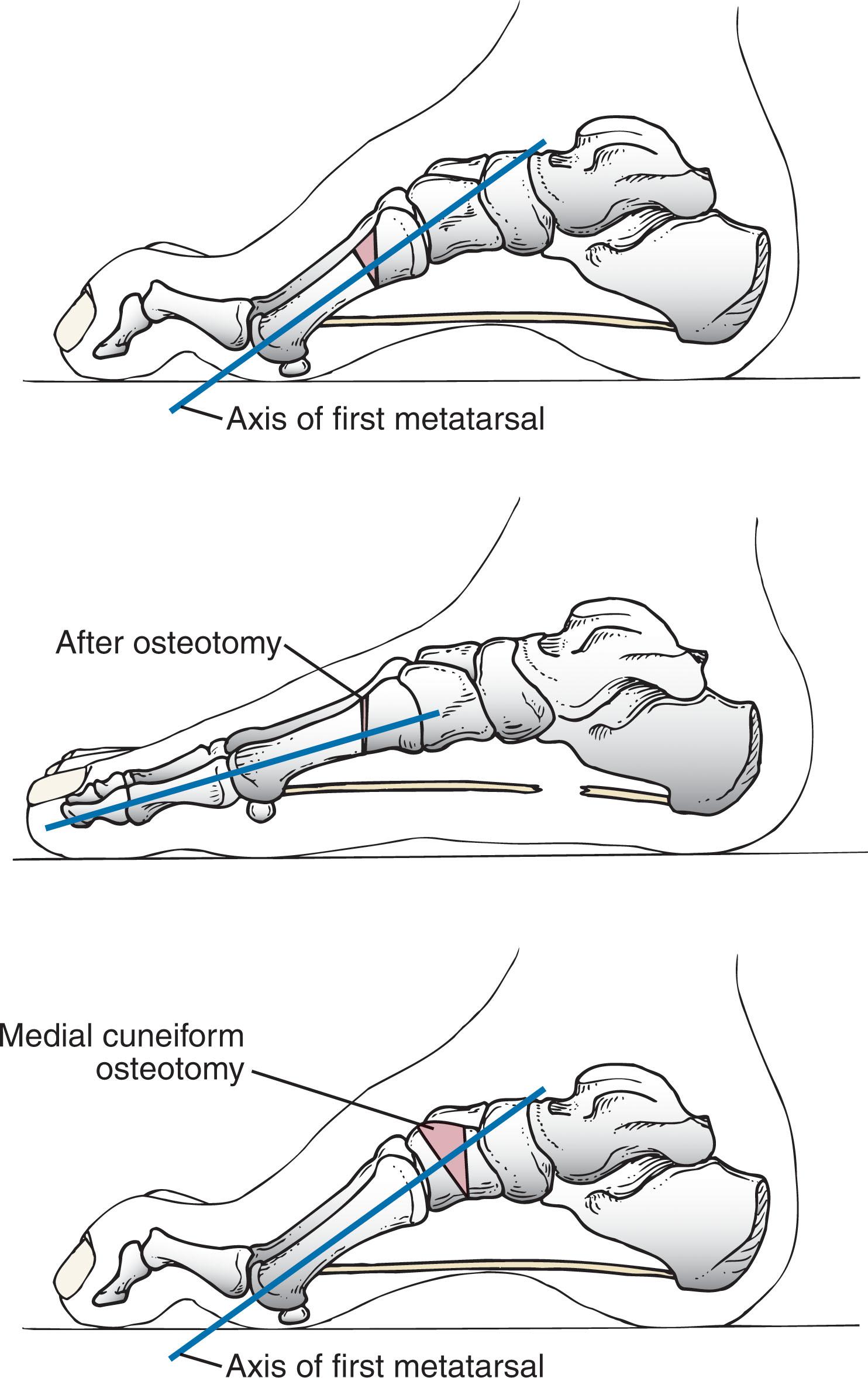
When the hindfoot corrects completely to slight valgus with the Coleman block test and the medial ray is fixed in plantar flexion, a medial column dorsiflexion osteotomy is indicated ( Fig. 19-13 ). Careful examination of the forefoot will reveal whether this deformity is limited to a plantar-flexed first ray, or if the second and sometimes the third rays are also involved. When only the first metatarsal is plantar flexed, a dorsal closing-wedge osteotomy of the medial cuneiform can be performed. In general, the osteotomy should be located at the apex of the midfoot as seen on the standing lateral radiograph. In some presentations, a dorsal closing-wedge osteotomy across the midfoot (navicular/cuneiforms/cuboid) is necessary. If there is an adductus component, this can require a biplanar osteotomy (dorsal–lateral). It should be noted that the reliability of achieving bony compression is greatest for the first metatarsal osteotomy, so one must consider whether the quality of the bone to be compressed will allow adequate fixation if a cuneiform or other osteotomy is contemplated.
The technique is as follows.
The proximal first metatarsal is isolated through a medial incision. In the skeletally immature foot, the proximal location of the first metatarsal growth plate must be identified and protected. The anterior tibial tendon must also be protected.
A dorsal closing-wedge osteotomy is most useful. Care is taken to maintain the plantar cortex. The first ray is dorsiflexed, and the overall alignment is assessed.
Fixation is generally with a smooth pin in the skeletally immature patient and with a distal-to-proximal screw or dorsal–medial plate in the skeletally mature patient.
An alternative method for stabilization is to approach the base of the first metatarsal dorsally and perform a closing-wedge osteotomy from the top. This can be stabilized with a tension band wire placed around a post created with a 2.4-mm screw adjacent to the tarsometarsal joint. A 22-gauge wire is sufficient ( Fig. 19-14 ).
Careful assessment is then made of the second and third metatarsals. If further deformity correction is required, an incision is made between the proximal half of the second and third metatarsals. The proximal portion of the second metatarsal is exposed subperiosteally, and a long oblique osteotomy is performed. Then the distal portion of the second metatarsal is allowed to float into its corrected position. A small amount of cancellous bone graft obtained from the calcaneus can be used to enhance bone healing around the first and second metatarsal osteotomies.
The dorsal closing-wedge osteotomy of the medial cuneiform is performed through a slightly more proximal incision. The tibialis anterior will be crossing over a portion of the cuneiform and must be protected. The first osteotomy is parallel to the distal articular surface of the cuneiform at about the distal two thirds. Make the second cut, creating and removing the appropriate-size wedge. Dorsiflex the first ray and use internal fixation. Remember that the medial cuneiform is wedge shaped and narrower at the base.
In general, the peroneus longus tendon maintains its strength well into the disease process. It is a primary deforming force and therefore an excellent choice for tendon transfer, which removes a deforming force while providing a useful and functional motor for transfer. Specifically, the goal is to oppose adduction by the posterior tibialis tendon and/or to aid in dorsiflexion of the foot. The latter is accomplished by tendon transfer around the fibula into the cuboid and the former by tenodesis to the peroneus brevis tendon.
The technique is as follows.
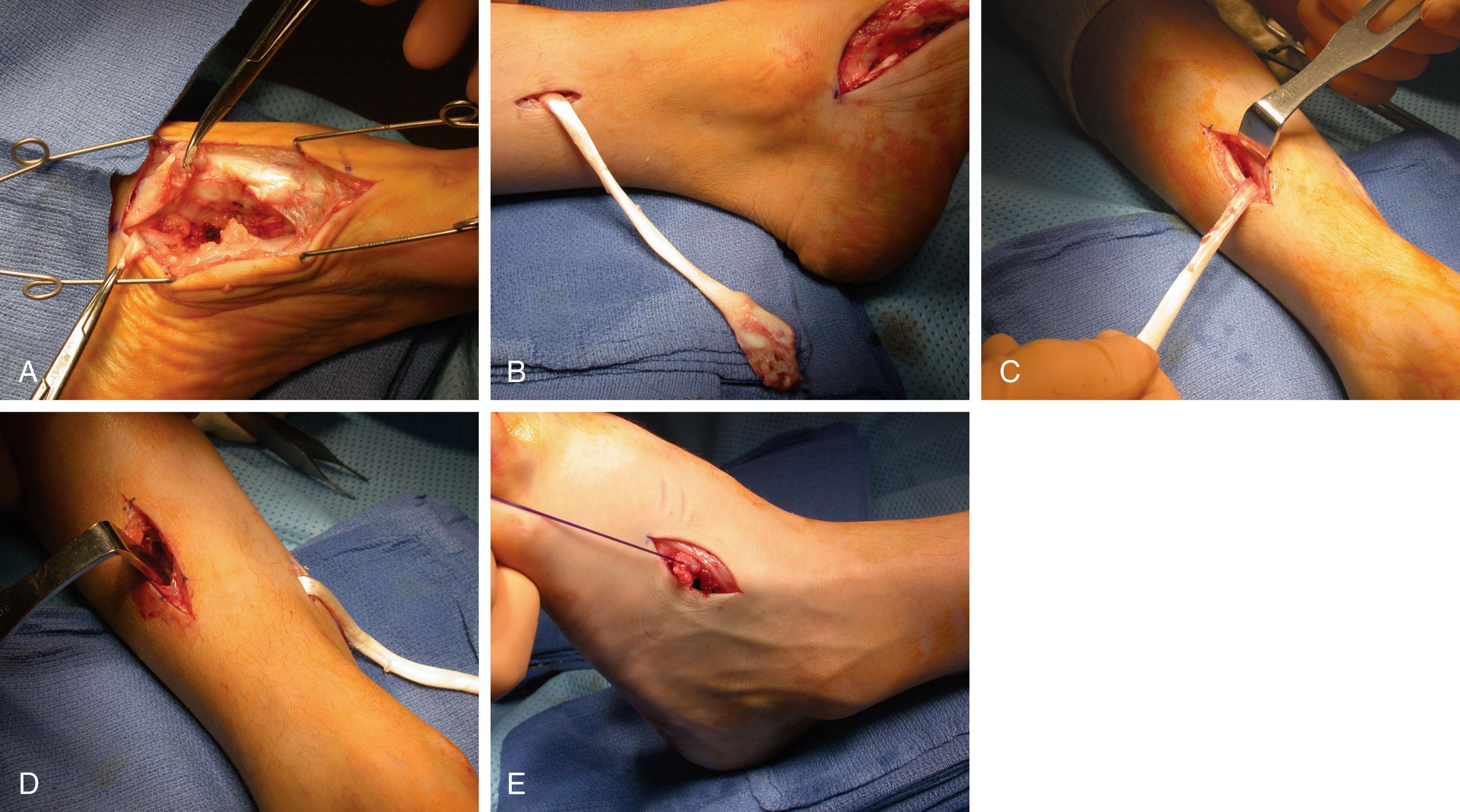
The incision for the calcaneal slide osteotomy is extended to the base of the fifth metatarsal, staying dorsal to the plantar skin. Alternatively, a small second incision is made following the distal course of the peroneus brevis tendon.
The abductor digiti quinti muscle is encountered first and retracted. The peroneus brevis tendon is identified and retracted, and the peroneus longus tendon is found deep to it against the groove in the cuboid.
The peroneus longus tendon is brought into the wound’s more superficial aspect with a right-angled instrument, the transection site is selected, and a suture is placed just distal to this and tied into the insertion of the peroneus brevis.
An incision is made approximately 10 cm proximal to the tip of the lateral malleolus just behind the fibula, with sharp dissection down through the skin and subcutaneous tissues. The peroneal sheath is opened. A slight tug on the peroneus longus distally identifies the tendon proximally. The tendon is then brought into the proximal wound.
An incision is made over the cuboid in line with the fourth metatarsal, and the peroneus longus tendon is transferred subcutaneously to this level.
The transferred tendon is secured using soft tissue anchors and heavy absorbable suture.
An alternative peroneus longus transfer is to the peroneus brevis tendon. Tenodesis can be accomplished over the last 3 to 4 cm of the peroneus brevis before its insertion into the fifth metatarsal. If a fixed adductus deformity exists, however, a medial release or midfoot osteotomies must be considered.
After the triceps surae musculature, which almost always maintains some strength, the posterior tibial tendon is the second strongest motor around the foot and ankle. Therefore it is usually a late deforming force and a motor with enough residual power to be considered for transfer. The posterior tibial tendon is transferred through the interosseous membrane ( Fig. 19-15 ) in patients with a foot that is essentially paralyzed except for the posterior tibial tendon and the triceps surae. A lengthening of the triceps surae may be necessary if an equinus contracture is present, but in the absence of equinus or if a calcaneocavus deformity is present, lengthening is typically not necessary.
When dealing with the posterior tibial tendon as a deforming force in the presence of significant midfoot adductus, the flexible deformity may be corrected with a medial release and transfer of the peroneus longus to the peroneus brevis tendon. In the fixed deformity, correction of the metatarsus adductus may require midfoot osteotomies ( Fig. 19-16 ).

The technique is as follows.
A short medial incision is made over the talonavicular joint. The posterior tibial tendon is identified and sharply excised from the navicular and cuneiform, obtaining as much length as possible.
Another short incision is made approximately 10 cm above the medial malleolus just behind the tibia. The posterior tibial tendon is readily identified proximally and then brought into this wound. The flexor digitalis longus (FDL) tendon is typically the first tendon visualized through this incision.
At the same level, approximately 10 to 12 cm above the ankle, a straight anterior incision is made just lateral to the crest of the tibia. The anterior compartment along with the neurovascular bundle is then retracted laterally. The interosseous membrane is then identified between the fibula and tibia.
A window approximately 3 -cm wide is made in the interosseous membrane. An instrument is then passed through the interosseous membrane, remaining on the tibial cortex, transferring the posterior tibial tendon deep to all other structures and through the window.
The tendon is then passed subcutaneously or underneath the retinaculum and carried down to the level of the cuboid and anchored using a soft tissue anchor with absorbable suture. Alternatively, the tendon can be fixed with a tenodesis screw if there is sufficient length. The tendon may be also sutured to the peroneus tertius.
Correction of clawing of the great toe with transfer of the EHL tendon is often indicated for the symptomatic deformity. This also improves the role of the EHL as an ankle dorsiflexor.
The technique is as follows.
A midline incision is made over the dorsum, exposing the MTP and IP joints of the hallux. With the EHL tendon protected, cartilage is removed at the IP joint and fixed with a single screw from distal to proximal ( Fig. 19-17 ).
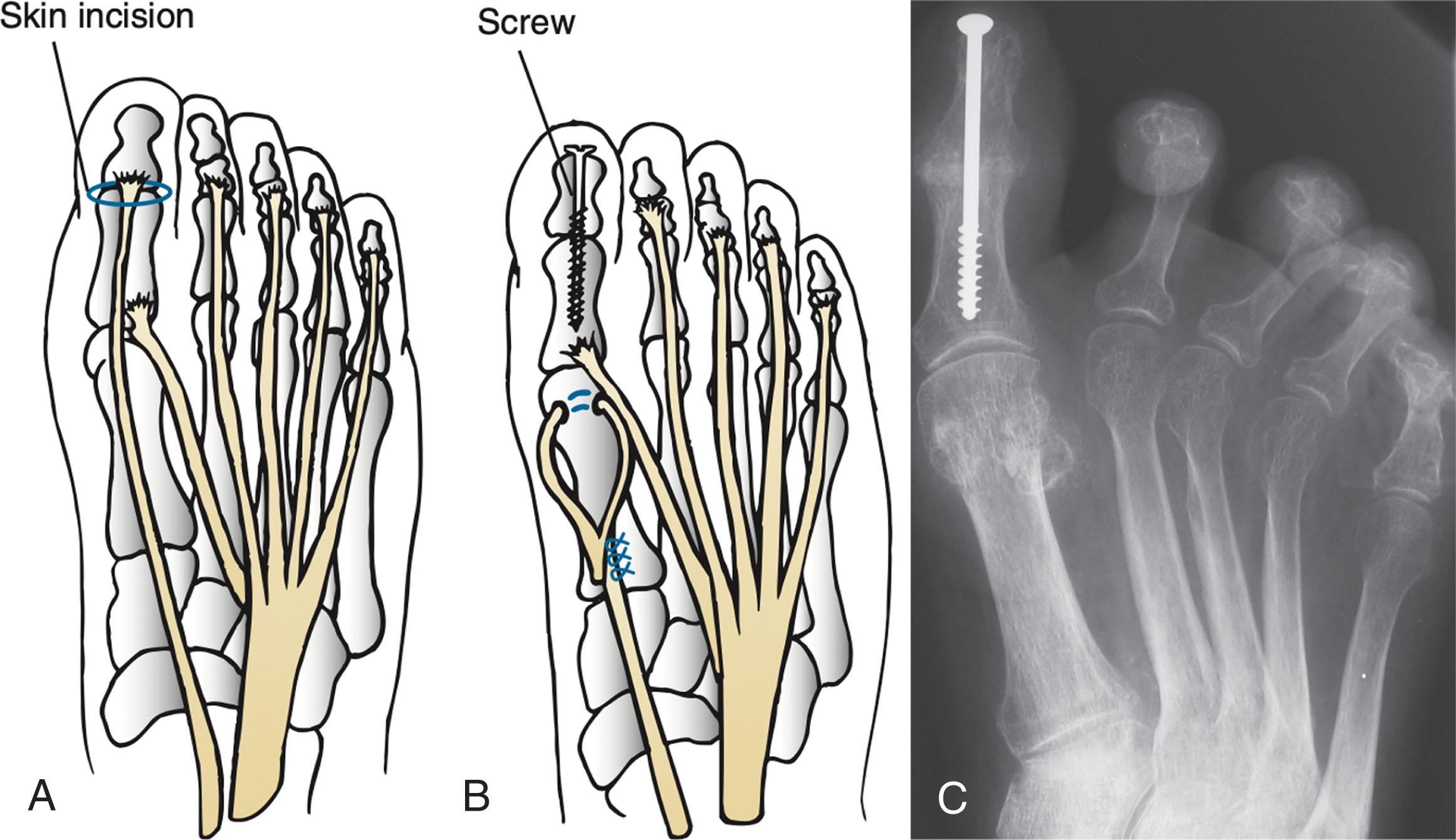
The EHL tendon is then transected, leaving enough tendon to allow tenodesis of the MTP joint in a neutral position.
The EHL tendon is then tenodesed into the distal portion of the first metatarsal through a drill hole, with the foot held in a neutral position at the ankle to apply appropriate tension (see the technique for the Jones procedure in Chapter 30 ).
If the extensor digitorum communis tendon is a deforming force acting to dorsiflex the foot, it could be tenodesed to the dorsum of the foot, again making sure that appropriate tension is achieved. If the toe deformities are flexible, a Girdlestone-Taylor transfer may be performed. If significant clawing is present, an MTP capsulotomy transecting the collateral ligaments will be necessary to achieve realignment. If the deformities are fixed, a Girdlestone-Taylor procedure may still be done, but resection of the proximal interphalangeal joint (PIP) with fusion may be indicated (see the technique for the Girdlestone-Taylor tendon transfer in Chapter 9 ).
For any procedure used to correct a progressive neuromuscular condition, the outcome is difficult to evaluate. Evaluation of triple arthrodesis, which for years has been a hallmark procedure in the treatment of the severe cavovarus foot deformity in this diagnosis, would indicate mixed results at best. Triple arthrodesis should be used only as a salvage procedure for a rigid deformity that shows signs of degenerative joint disease of the hindfoot. It is particularly important to ensure that concomitant ankle instability is addressed with ligamentous reconstruction, with or without anterior ankle debridement, and that the hindfoot is positioned in a neutral position if a triple arthrodesis is deemed necessary.
The triple arthrodesis can be an excellent salvage procedure. The concept of removing wedges to perform this arthrodesis is rarely beneficial. The key to successful correction of the deformity is derotation of the calcaneus under the talus, allowing the talus to plantar flex and the hindfoot varus to move into slight valgus. See Chapter 25 for further discussion of triple arthrodesis.
A variety of midfoot osteotomies have been described, the rationale being that the midfoot is the apex of the deformity. The Japas procedure is essentially a vertical chevron osteotomy through the midtarsal region. The Jahss procedure is a truncated wedge osteotomy through the midtarsal region at the apex of the deformity; however, the foot must have appropriate muscular balance.
Extraarticular corrections are preferred. The cavus deformity in the sagittal plane typically is readily correctable with calcaneal and first metatarsal osteotomies. If present, the adductus deformity in the transverse plane can be corrected with closing-wedge cuboid and opening-wedge cuneiform osteotomies. For the most severe deformities, a biplanar closing-wedge osteotomy through the midfoot (navicular/cuneiform/cuboid) is used.
Ankle instability must be documented and some form of treatment instituted. When the cavovarus foot is reconstructed, a lateral ligamentous reconstruction can be performed as well. This can be done with local tissues and suture anchors or autologous tendon.
Both joint sparing and joint sacrificing procedures, as outlined above, improve patient-reported quality outcomes in CMT. A series of 52 feet were retrospectively divided into those that had joint-preserving correction of cavovarus foot disorders and those that had fusions. Both groups improved outcomes based on the Foot and Ankle Disability Index (FADI). At 2 years, the functional improvement was greater in the joint preserving group, though the lack of randomization makes comparison between groups difficult. A retrospective review of 63 feet that had corrective surgery between 1967 and 2018 for CMT found a trend toward more joint-preserving surgery in the last decase. Overall, there was an 80% patient satisfaction rate with the outcome of their surgery, though walking ability based on the Walking Handicap Scale decreased as patients aged. Corrective surgery combined with intensive rehabilitation improved walking and balance, reduced pain, and increased ankle power in a small series.
The use of regional anesthesia, including indwelling catheters, did not worsen neuropathic symptoms in a series of 20 CMT patients undergoing foot surgery, based on pre- versus postoperative monofilament sensatory testing.
Myelomeningocele is a congenital malformation of the CNS, resulting in dysplasia of the vertebral elements as well as the spinal cord. Early closure of the meningocele with placement of a ventricular peritoneal shunt has vastly improved these patients’ survival. Folate supplementation in prenatal and pregnant woman has lowered the risk of this condition.
These patients are classified by their level of involvement into four basic groups: thoracic, upper lumbar, lower lumbar, and sacral. The thoracic and upper lumbar patients are, by definition, paralyzed below the knee but might have involuntary motors function affecting foot position. The pattern of sensory and motor loss is seldom symmetric. This is a CNS disorder, and both lower motor neuron (flaccid paralysis and lack of sensation) and upper motor neuron (spasticity) abnormalities must be considered. Growth can also change the basic neurologic picture because of tethering of the cord from soft tissue scars or bony anomalies within the vertebral column.
Treatment of this disorder involves a range of deformities, from congenital presentations to modeling changes in the growing foot and conditions in the skeletally mature patient. Up to one half of children with myelomeningocele have some type of significant foot deformity. The most common congenital foot deformity is talipes equinovarus (clubfoot) deformity. Vertical talus is also noted with this diagnosis. Other deformities include calcaneus and equinus of the hindfoot with components of valgus or varus. The primary goal in treatment of these foot deformities is a relatively supple plantigrade foot. Because of the highly variable paralytic and sensory deficit and variable functional capacity, treatment of these patients must be determined carefully. It is just as important for the nonambulatory patient to have a plantigrade, shoeable foot that fits on the footrest of a wheelchair as it is for a low lumbar patient with good quadriceps function to have a plantigrade and braceable foot and ankle for ambulation.
Although the early emphasis in these children is on functional motor level (i.e., whether they will ultimately ambulate), an important long-term prognostic factor is foot sensibility. Most of these children have an insensate foot and loss of proprioception; only patients with the lowest lumbar and sacral levels have any preservation of plantar skin sensation. Early patient and parent education focuses on careful inspection of feet, socks, and footwear. All children with this diagnosis should wear some type of orthosis as a protective measure for the insensate foot and a preventive measure against the deforming forces that can lead to fixed contractures and deformities. These children must never be barefoot and, even when swimming, must wear some appropriate form of protective footwear.
Discussions of foot sensory deficits with patients and their parents must also include the need for preservation of a plantigrade foot. Deformity that limits the weight-bearing contact surface of the foot’s plantar aspect increases focal pressures and can result in ulcerations. The correction of deformity alone is not enough; deforming forces around the foot and ankle must be balanced as well.
Bracing and orthosis use, combined with functional training, may improve gait in children with myelomeningocele. When these measures fail, tendon transfers and extraarticular osteotomies can be used to reduce pressure on the calcaneus. Although triple arthrodesis is an excellent procedure for the correction of severe deformities of the foot, it is not appropriate in patients with sensory compromise. Arthrodesis to correct deformities of the foot and ankle in these patients should be avoided. Rigidity of the foot and ankle reduces the foot’s ability to accommodate to irregularities of the ground. This can result in increased pressure on the foot’s plantar surface and on the joints adjacent to the sites of fusion. This increased pressure through the remaining articulations of the foot and ankle can result in the Charcot neuropathic arthropathy. However, in the older or nonambulatory patient who has trouble fitting shoes or braces, triple arthrodesis is a good compromise to obtain a plantigrade foot. Even then, a limited fusion is preferable.
Use of casting in these patients should be reserved for healing of ulcerations and for the protection of soft tissues after surgical reconstructive procedures. Serial casting of deformities can be problematic because of the insensate nature of the foot. The casting of the congenital deformities in these patients must be carefully considered. The majority of these feet will eventually need surgical correction. If no correction is found after short-term casting, the clinician should consider the use of holding splints until the child’s foot is mature enough to undergo surgery. Postoperative casting must be lightweight, be carefully padded, and have room for swelling. The cast should be used only to support the soft tissues and not to achieve foot correction.
When an insensate foot is covered with a cast, there must be a low threshold for removal of the cast and for inspection of the soft tissue envelope of the foot. Whenever persistent fever occurs with no evidence of a respiratory or urologic cause, the cast must be removed and the foot examined. Total-contact casts are the most common type of casting used in the patient with myelomeningocele. The first cast should be changed after 1 week and then changed every 1 or 2 weeks after that. The total contact equally distributes plantar pressure and helps diminish swelling.
Recurrent plantar ulcerations require patient education and careful evaluation of the foot and ankle for deformities causing increased pressure on the foot’s plantar surface. If a bony prominence cannot be protected with the orthosis, surgery is indicated. Surgery must be performed in a latex-free environment.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here