Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Patients admitted to the intensive care unit (ICU) frequently have conduction disturbances because of their acute medical condition or underlying risk factors. The clinical manifestation varies broadly from asymptomatic to life-threatening events. Locating and understanding the conduction disturbances are vital to stratifying the patient’s risk and choosing the best medical or invasive therapy option.
Depolarization of the myocardium begins spontaneously from a specialized group of cells forming the sinoatrial (SA) node located in the superior and posterior portion of the right atrium (RA). They are regulated by the sympathetic and parasympathetic nervous system. The activity of the cells cannot be seen on a surface electrocardiogram (ECG).
SA depolarization spreads through the right then left atrium, resulting in the P wave seen on the surface ECG. Because the atria and ventricles are electrically isolated, the impulse must travel through the atrioventricular (AV) node, located in the lower part of the atrial septum and regulated by the sympathetic and parasympathetic nervous system as well, to generate the PR interval on ECG.
The impulse is transmitted to the ventricles through the bundle of His, dividing into right and left bundle branches to finally diffusely ramify to form the Purkinje network, resulting in the QRS wave on ECG. The ventricular repolarization can be observed as the T wave on ECG. The atria repolarization is hidden by the ventricular depolarization (QRS).
Bradycardia is defined as a heart rate (HR) <60 bpm. It can be divided into two categories: sinus node dysfunction (SND), when the rate of impulses arising from the SA node is lower than expected, and AV block, when there is failure to propagate the impulse from the atrium to the ventricle. SND and AV block share common etiologies and may be present at the same time. Nevertheless, their prognosis and treatment are not the same. A high-quality 12-lead surface ECG is mandatory to help differentiate them. Etiologies of bradyarrhythmia are listed in Table 73.1 .
| Intrinsic | Extrinsic |
|---|---|
|
|
SND refers to a number of conditions causing symptoms and inappropriate atrial rates (bradycardia, sinus pauses, and sinus arrest). Symptoms could include weakness, chronotropic incompetence (inability to reach a targeted heart rate), palpitations, and syncope. The mechanism is either an inner pacemaker defect or an SA block ( Table 73.2 ). Degenerative age-related SA fibrosis is the main cause of SND, affecting patients in their seventies and eighties. The fibrotic process, however, is not just limited to the SA. SND is often associated with AV node fibrosis as well. Patients with symptoms attributable to SND have a higher risk of cardiovascular events, including syncope, atrial fibrillation, and heart failure (HF). Moreover, the development of chronotropic incompetence with age is associated with an increased risk of cardiovascular death and overall mortality. Usually, SND is chronic and the result of irreversible causes. Even when clinical presentation is acute and potentially reversible, as in acute myocardial infarction, electrolyte/metabolic disturbances, dysthyroidism, and iatrogenesis (e.g., beta-blocker [BB] use), symptoms are typically mild, stable, and generally do not require therapy apart from correcting the metabolic disturbances and stopping the medication that generated the syndrome. In brady-tachy syndrome (a variant of SND), SND is responsible for pauses after termination of atrial tachyarrhythmia and often needs either invasive ablation of the arrythmia, permanent pacing, or both. Table 73.3 shows a description of the different etiologies of SND.
| Sinus Bradycardia | Sinus Pause/Arrest | Sinus Node Exit Block | Bradycardia-Tachycardia Syndrome | |
|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
| Congenital Sinus Node Dysfunction |
| Long QT syndrome, Brugada syndrome, congenital heart disease, noncompaction cardiomyopathy |
| Acquired Sinus Node Dysfunction |
| Myocardial ischemia |
| Infective heart disease |
| Dengue fever, Chagas disease, encephalitis, endocarditis, Legionnaires disease, typhoid, diphtheria, rheumatic carditis |
| Autoimmune diseases |
| Systemic lupus erythematosus, systemic sclerosis |
| Infiltrative diseases |
| Hemochromatosis, cardiac lipomatosis, amyloidosis |
| Endocrine disease |
| Hypothyroidism, hyperthyroidism, hyperparathyroidism, phaeochromocytoma |
| Autonomic dysfunction |
| Carotid hypersensitivity syndrome, athletic training, intracranial hypertension |
| Drugs |
| Antiarrhythmics, digitalis, ticagrelor, lacosamide, carbamazepine, lithium, ropinirole, ranitidine, clonidine, diphenylhydantoin |
| Iatrogenic |
| Cardiac surgery procedures, especially for congenital pathologies |
| Radiofrequency catheter ablation of arrhythmias |
| Percutaneous coronary intervention: right coronary artery stent implantation because of iatrogenic occlusion of sinus node artery |
AV block encompasses all possible lesions, congenital or acquired, that may interrupt or delay the normal propagation of the sinus node impulse to the ventricles. The most common cause is degenerative. Congenital (Fallot, transposition of the great arteries, etc.) and systemic disorders (amyloidosis, Fabry disease, etc.) are rarer nonreversible etiologies ( Table 73.4 ). As block level and position are associated with different prognoses and therapeutic options, locating block sites helps in understanding the mechanism and stratifying the patient’s risk. AV node location (supra-Hisian) is characterized by a slower progression of the disease and a more sustained and reliable junctional escape mechanism with better response to chronotropic drugs (atropine, isoproterenol). On surface ECG, the QRS complex is usually thin. In contrast, intra- and infra-Hisian AV blocks are characterized by a broader QRS complex (>120 ms), poorer prognosis, faster progression, less reliable junctional escape mechanism, and poor or paradoxical response to chronotropic drugs. Some clinical maneuvers can help to identify the level of the disease. Carotid sinus massage, which increases the vagal tone and slows the sinus rate and conduction through the AV node, would further deteriorate nodal block. It may improve the infra-Hisian block by improving the His-Purkinje conduction of slower sinus beats. Atropine, isoproterenol, and exercise would improve a supra-Hisian block but would deteriorate an infra-Hisian block.
| Electrolyte disturbances | Hyperphosphatemia or hypophosphatemia |
| Acidosis | |
| Hypoglycemia | |
| Hypoxemia/hypercapnia | Sleep apnea, alcohol and/or drug abuse |
| Ischemia | Acute myocardial infarction |
| Heart surgery | Maze procedure |
| Valve replacement | |
| Infectious | Lyme disease |
| Acute rheumatic fever | |
| Diphtheria, Legionella , psittacosis, typhoid fever, Listeria , malaria, leptospirosis, dengue fever | |
| Viral syndrome | |
| Dysthyroidism | Hypothyroidism |
| Hypervagotonia | Stress, pain, carotid compression, other |
| Drugs | Beta-blockers |
| Non-dihydropyridine calcium channel blockers | |
| Digoxin and antiarrhythmic drugs | |
| Lithium, methyldopa, risperidone, cisplatin, interferon | |
| Autoimmune disease | Sarcoidosis, ankylosing spondylitis, rheumatoid arthritis, scleroderma, lupus |
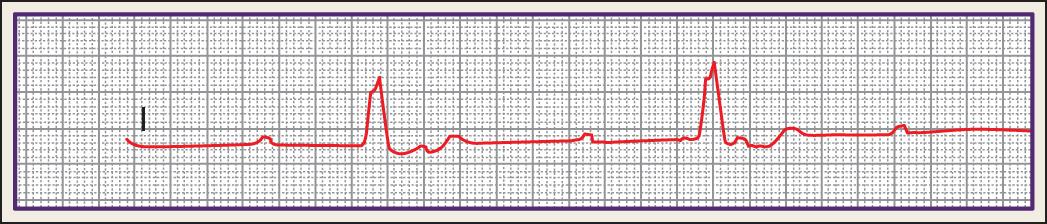
AV blocks are also categorized according to a three-degree scale. In first-degree AV block (BAV 1°), every P wave is conducted to the ventricles with an increased conduction delay (PR >200 ms) ( Fig. 73.1 A). BAV1° is usually asymptomatic and requires no treatment.

In second-degree AV blocks (BAV 2°), some P waves are not conducted to the ventricles. BAV 2° are divided into two types:
Mobitz I is defined by a progressively longer PR period on consecutive beats, ultimately followed by a blocked P wave. The next PR period is then reset to the shortest duration and it repeats (Wenckebach conduction). The block location is usually nodal (72%) (see Fig. 73.1 B).
Mobitz II does not follow the same scheme and preserves a certain degree of P-wave conduction (see Fig. 73.1 C). The block location is usually intra-Hisian (20%) or infra-Hisian (80%).
The clinical presentation of first-degree AV block is usually benign and only very rarely are symptoms felt to be directly related to first-degree AV block. There are no signs or symptoms that are either sensitive or specific for first-degree AV block.
Most patients with high AV block will present with some degree of symptoms, though the severity of the symptoms can be quite variable. Symptoms in high AV block (Mobitz II) may include fatigue, dyspnea, chest pain, presyncope, syncope, Stokes-Adams attack, and sudden cardiac arrest.
The P:R ratio is used to describe how many P and QRS waves are contained in one repetitive block. The higher the ratio, the more severe the block. A case of 2:1 BAV 2° can be particularly challenging to determine whether it is Mobitz type I or II.
High-degree or high-grade blocks refer to more than two consecutive nonconducted P waves without a complete loss of AV conduction ( Fig. 73.2 ). These latter types are more intra- or infra-Hisian and associated with a poorer prognosis.
In cases of acute myocardial infarction, acute AV blocks secondary to right or circumflex coronary artery (responsible for AV and His bundle vascularization in most of the cases) occlusion are usually nodal and associated with a good prognosis and rapid recovery. Those secondary to left anterior descending artery (LAD) occlusion (responsible for right and left anterior bundle brunch vascularization) are associated with a poorer prognosis (infra-Hisian location) and fatal ventricular arrythmia.
Measurements of electrolytes, glycemia, pH, renal function, thyroid function, and Lyme serologic testing (if clinical suspicion of Lyme carditis) should be performed in any acute bradyarrhythmia, as they are common and reversible causes that can be treated promptly with possible normalization of conductance disturbances.
Conduction disturbances are encountered in a wide range of cardiovascular and systemic disease with very different prognoses and treatments. Assessment of heart structure and function is highly useful in order to exclude cardiomyopathies, valvular heart diseases, tumors, infections (endocarditis with abscess formation), congenital anomalies, infiltrative processes, great vessel disease, and pericardial diseases. Except for sinus bradycardia and first-degree AV block with no evidence of structural heart disease, it is recommended to perform a transthoracic echocardiography. This is especially true in newly identified left bundle branch block (LBBB; patients with LBBB have a higher prevalence of both noncardiovascular and cardiovascular comorbidities, including structural heart disease), AV block Mobitz II, and high-grade AV block. Magnetic resonance imaging (MRI) can be helpful in diagnosing an infiltrative or dilated cardiomyopathy. Cardiac computed tomography (CT) is helpful for the assessment of valve calcification and coronary artery disease.
The initial management of the patient with AV block depends on the presence and severity of any signs and symptoms related to the ventricular rate ( Fig. 73.3 ). Unstable patients may require pharmacologic therapy and, in some cases, should also receive temporary pacing to increase heart rate and cardiac output. Once the patient is hemodynamically stable, assessment and treatment for any potentially reversible causes should occur, followed by placement of a permanent pacemaker for patients without an identifiable reversible etiology.
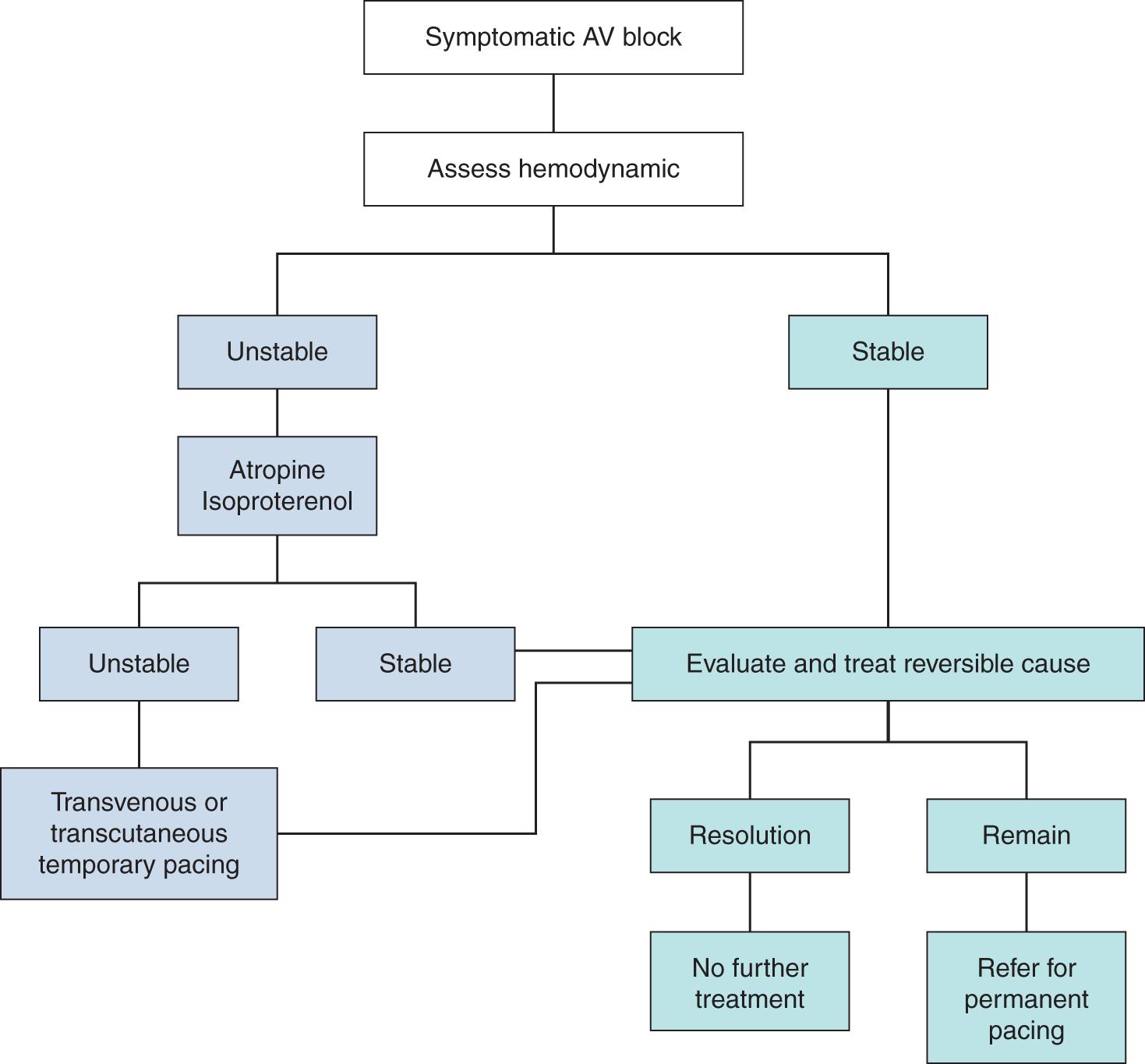
Regarding the pharmacologic therapy, atropine should be used in patients with symptomatic bradycardia or hemodynamic (HD) compromise with SND except in patients with heart transplant, in which paradoxical heart block is observed. , Isoproterenol may be used in symptomatic bradycardia/HD compromise with SND, but there are no data to either support or discourage its use in sinus bradycardia. , , Atropine should be used in patients with symptomatic bradycardia or HD compromise with second- or third-degree AV block with caution when the block location is thought to be intranodal or infranodal because of paradoxical worsening of conduction. Isoproterenol may be used in patients with symptomatic bradycardia or HD compromise with second- or third-degree AV block if the likelihood of myocardial ischemia is low.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here