Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Mandibular distraction osteogenesis (MDO) remains a mainstay of surgical treatment for Pierre Robin Sequence (PRS). Three-dimensional (3D) printing and computer-assisted design/computer-assisted manufacturing (CAD/CAM) technology has revolutionized our ability to visualize, plan, and execute surgical treatment within craniofacial surgery. In this chapter, we will more fully explore the treatment for PRS and the applications for CAD/CAM technology and 3D printing in the context of MDO.
PRS is typically diagnosed in the neonatal period and its severity is defined by the degree of upper airway obstruction, quantified by polysomnogram. Upper airway obstruction relieved by jaw thrust may also be a therapeutic maneuver helpful in confirming the diagnosis. Surgery is considered for patients with severe sleep apnea (Apnea Hypopnea Index [AHI] >10). Although a number of interventions exist, including prone positioning, , glossopexy, tracheostomy, and palatal expander placement, MDO is frequently favored because of its ability to lengthen the pediatric mandible and pull the tongue forward to improve laminar airflow within the retroglossal space of the upper airway. By definitively de-obstructing the upper airway, tracheostomy placement can be avoided in this fragile population.
Of course, not all PRS patients are candidates for mandibular distraction. Patients who exhibit other concomitant airway abnormalities such as central sleep apnea, multilevel airway obstruction, certain syndromic diagnoses, severe neurologic compromise, or airway edema from severe reflux are precluded from undergoing MDO, as their symptoms extend beyond the anatomy of the upper airway. For these patients, a tracheostomy may be performed in the neonatal period to reestablish a safe and accessible airway.
Several studies have characterized the distinct dysmorphology of the Pierre Robin sequence mandible. While the PRS mandible is globally hypoplastic, the effect is disproportionately pronounced in the longitudinal dimension of the ramus, leading to an upper airway that is more posteriorly retruded and vertically shallow. Additionally, the anterior symphyseal angle in these patients is more obtuse, which further contributes to the flattened and restricted airway, making it more prone to inspiratory collapse.
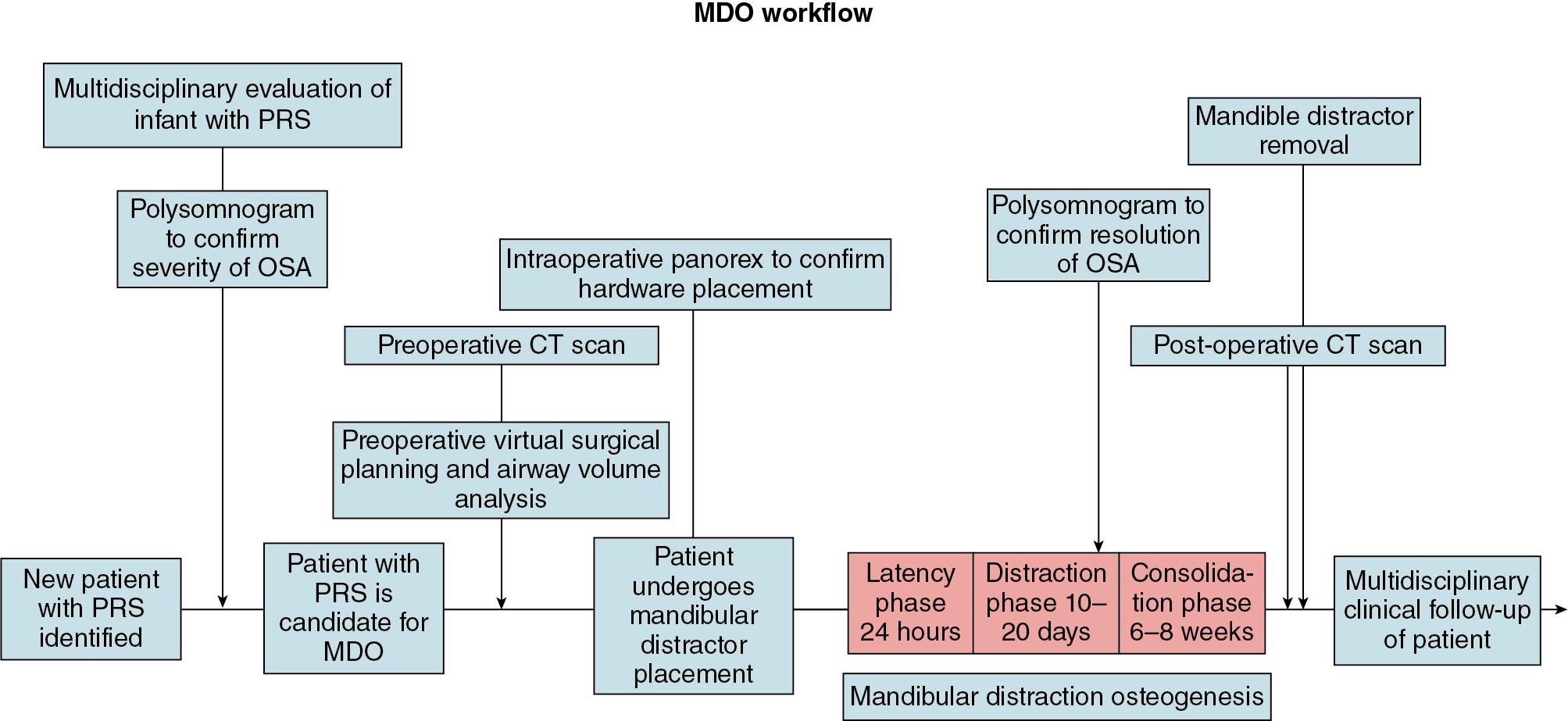
The initial presentation of patients with PRS typically occurs in the neonatal intensive care unit (ICU). Micrognathia is the most obvious physical indicator of underlying pathology, and, when combined with transient hypoxia and desaturations with supine positioning, usually triggers further clinical workup. The use of a multidisciplinary team consisting of neonatal intensivists, anesthesiology, plastic surgery, otolaryngology, speech pathology, and genetics is advantageous to establishing a safe temporary airway, stratifying surgical risk, identifying comorbid medical conditions, and determining safety and candidacy for MDO. At the University of Chicago, like many institutions, we have developed a multidisciplinary workflow to optimize care of these patients ( Fig. 16.1 ), which integrates the critical role of computer-assisted surgical planning (CaSP). Using this workflow, diagnostic and confirmatory testing is obtained, chief amongst them, a polysomnogram (PSG). A milk scan or 24-hour pH probe may be used to diagnose severe reflux, if clinical suspicion warrants. Direct laryngo-bronchoscopy by a pediatric otolaryngologist is helpful to more closely interrogate the anatomy and mechanics of the upper airway by confirming upper airway collapse and ruling out significant tracheomalacia, laryngomalacia, airway edema, vascular anomalies, or upper airway masses. Though cleft palate is not classically part of the triad of the PRS presentation, there is a high co-association and thus the involvement of speech and feeding therapists are critical to optimizing modifiable risk factors, such as malnutrition and feeding intolerance. A genetic workup is key to appropriately counseling families of syndromic patients regarding the need to overdistract to a severe class III skeletal relationship in select cases. This is done in order to prevent relapse and to compensate for the abnormal biomechanics of the syndromic upper airway. One must overcorrect with caution as maxillary “catch-up” growth to balance the skeletal relationships may never occur, especially in the case of a coexisting cleft palate. Parents should also be advised that their children may need future orthognathic surgery after skeletal maturity to correct occlusal issues, though the most critical role of MDO in the neonatal period is to obviate the need for tracheostomy.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here