Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
An approximation of a classic Sir John Charnley quote is: “It takes a curved cast to make a straight bone.” Nowhere is this more true that in the setting of fractures of the pediatric distal radius and ulna. However, we would be lucky if crooked was the only thing we had to worry about, as there are a variety of complications that may occur in association with these injuries. By their sheer volume (distal radius and ulna fractures being the most common pediatric fracture), over time any orthopaedic surgeon who regularly treats children will be confronted by one or more of these complications, some subtle and some not so much. The distal radius and ulna are high-growth areas, and this can have both beneficial and detrimental impacts following injury ( Table 6.1 ). The goal of this chapter is to facilitate their recognition and management. As an enigmatic pediatric orthopaedic surgeon has said: “The pathology is always looking at you, are you looking at it?”
| Ossification Center Appears | Physeal Closure | Avg. Growth/Year (late) | |
|---|---|---|---|
| Girls radius | 1 year (range 4–18 months) | 17 years a | 6.75 mm |
| Girls ulna | 4 years (range 3–6 years) | 17 years a | 8 mm |
| Boys radius | 1 year (range 6 months–2 years) | 19 years b | 7.5 mm |
| Boys ulna | 5 years (range 3–6 years) | 19 years b | 8.8 mm |
a Girls reliable continued growth/remodeling potential after physeal fracture <12 years.
b Boys reliable continued growth/remodeling potential after physeal fracture <14 years.
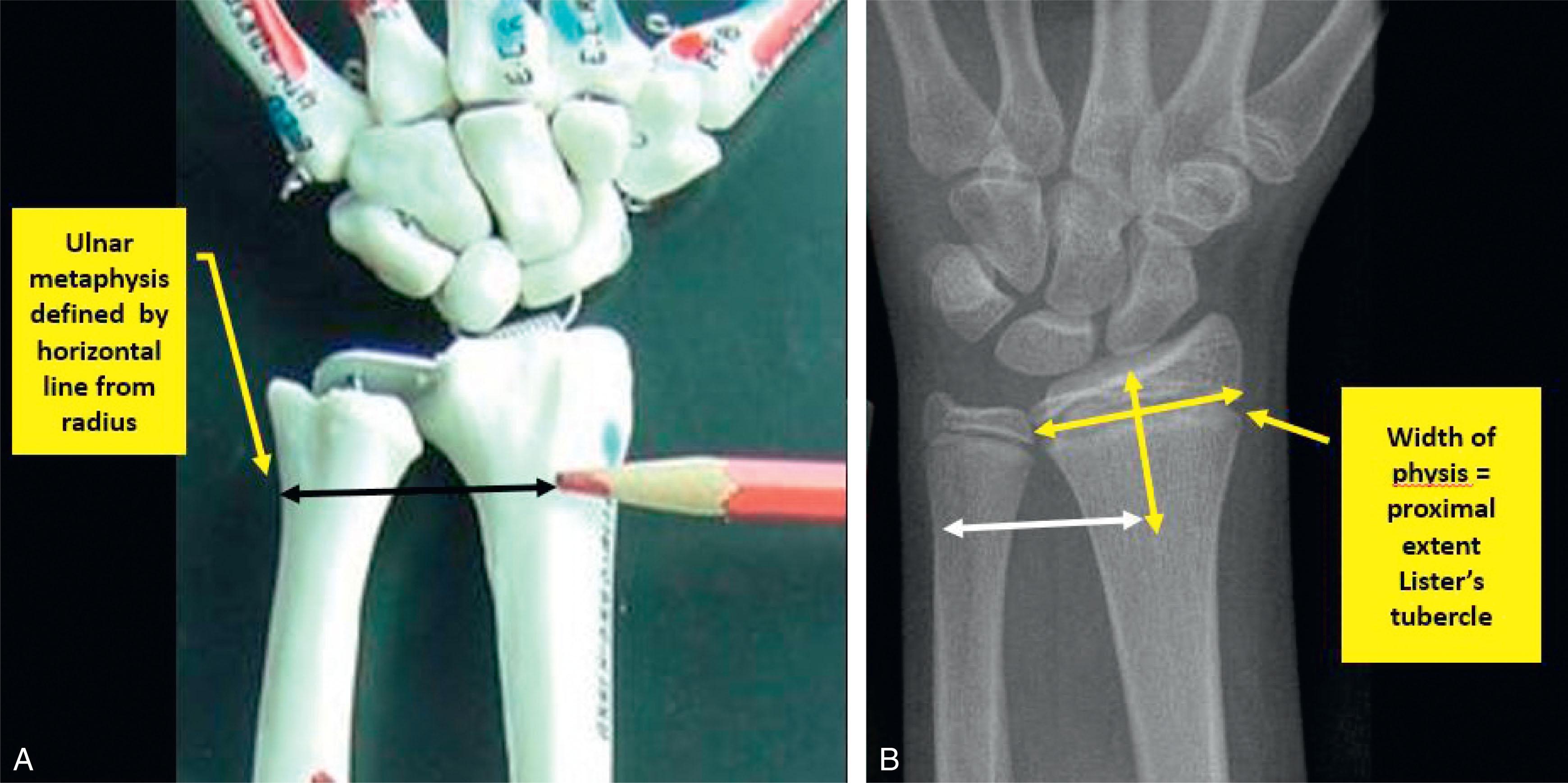
The first distal radius and ulna complication is misdiagnosis. In spite of their ubiquitous nature (or perhaps because of it) significant variation has been documented among pediatric orthopaedic surgeons regarding diagnosis and treatment of these fractures. It is also disturbingly rare for publications focusing on distal radius and ulna fractures to anatomically define the injuries that they discuss. Our definition of the distal metaphyseal regions of the radius and ulna relates to the anatomic landmark of the most proximal extent of Lister’s tubercle and the corresponding level of the adjacent ulna. Since Lister’s tubercle is not discernable on most plain radiographs, one may approximate its location by measuring the width of the physis on the anteroposterior (AP) radiograph and extending this same distance proximally from the distal aspect of the radius ( Fig. 6.1 ). The fractures that we will discuss in this chapter lie in this defined territory.
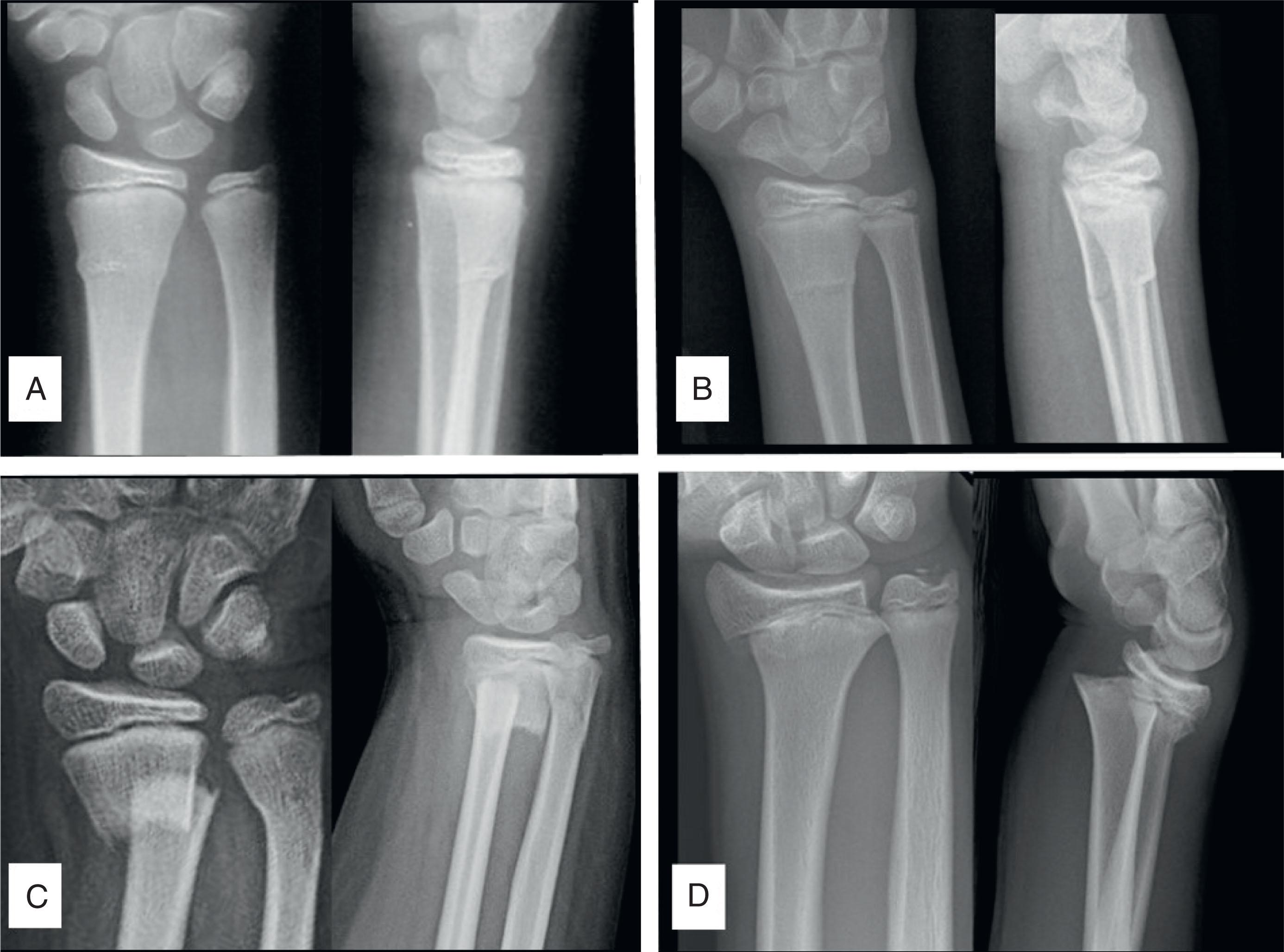
Beyond defining the anatomic region of these injuries, one must also accurately identify the specific fracture type. Four common patterns are recognized: buckle (aka torus), greenstick, complete, and growth plate fractures (almost exclusively Salter-Harris I and II) ( Fig. 6.2 ). The distinction is not at all esoteric, as substantial differences in prognosis exist (e.g., risk of displacement, risk of growth disturbance) for the different categories. It has been shown that orthopaedic surgeons can reliably classify such distal radial fractures when given visual examples with written descriptions. It can be said that starting with the right diagnosis is strongly associated with choosing the right treatment. For example, provided an accurate diagnosis is applied, robust data now show that buckle fractures can be treated quite minimalistically (e.g., a plaster-back slab in England or a removable wrist brace in Canada or the United States).
Another complication of distal radius and ulna fractures relates to needless delays in their acute management. Throughput time for procedural sedation (e.g., ketamine and midazolam) for forearm fracture reduction in pediatric emergency rooms is notoriously onerous, routinely exceeding 5 to 6 hours. Effective alternative pain control strategies such as hematoma blocks augmented with nitrous oxide have been well documented. The hematoma block has a long, successful history in orthopaedic surgery. It has been shown that 2 hours or more of time spent in the emergency department can be eliminated by applying such hematoma block–focused distal radius fracture reduction protocols to children.
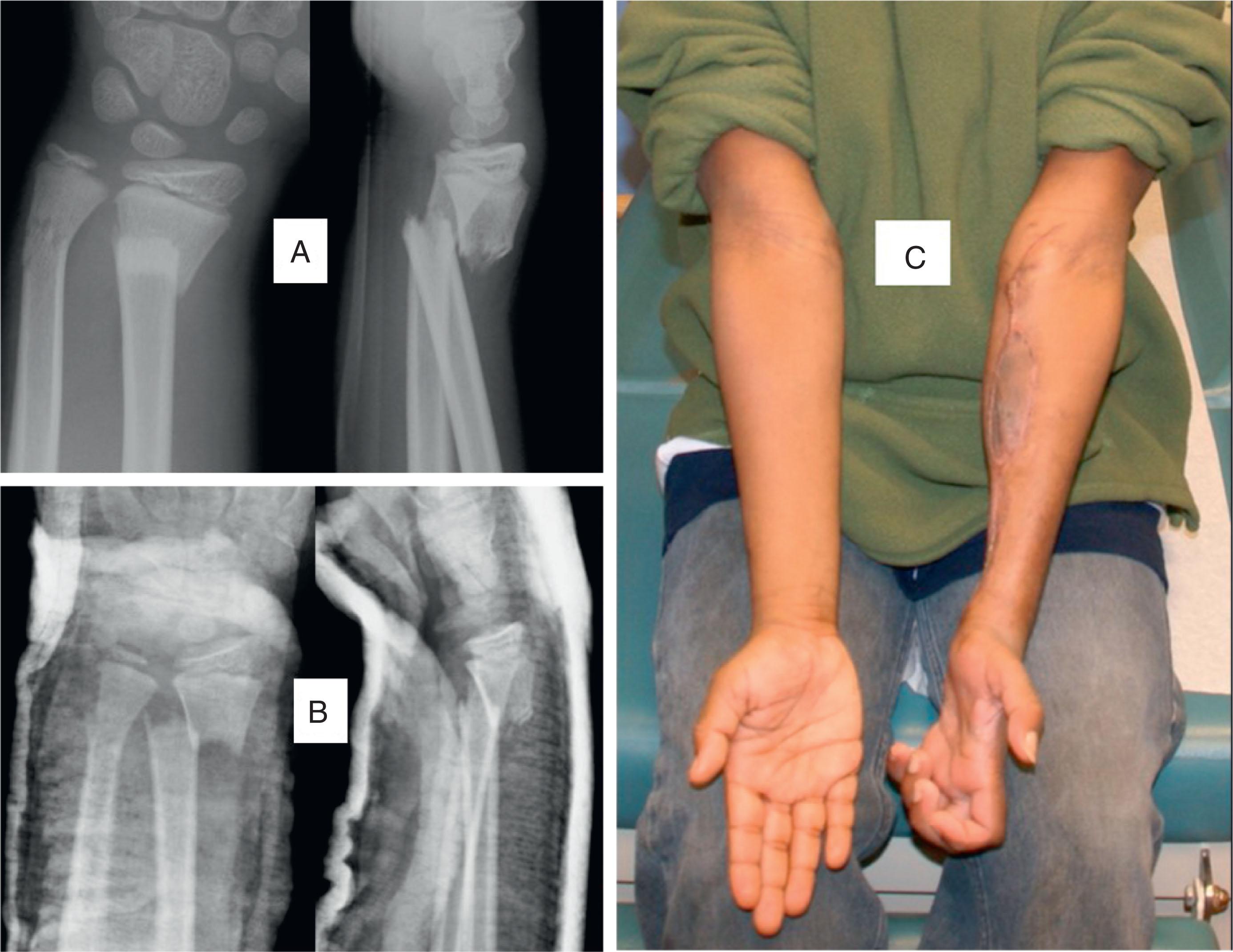
Markedly displaced fractures may lead to a particularly concerning complication: acute carpal tunnel syndrome and/or acute compartment syndrome. In the heat of the clinical moment there may not be clear demarcation between these two entities. Besides classic compartment syndrome symptoms, isolated median nerve symptoms may be due to compression or contusion. We are not talking about subtle tingling (perhaps with some motor findings) because 37% of distal radial physeal fractures and 13% of distal metaphyseal radial fractures will have such findings acutely. When acute carpal tunnel syndrome occurs it is commonly associated with substantially displaced growth plate fractures of the distal radius, but it can occur with other fracture patterns as well. Among 109 displaced radial physeal fracture patients presenting to a pediatric trauma center, 1.8% (two patients) were noted to have acute carpal tunnel syndrome in conjunction with acute forearm compartment syndrome (requiring fracture reduction followed by urgent decompression). It has been suggested that strong consideration be given to appropriate reduction and internal fixation of the fracture aimed at eliminating the need for the additional external pressure of a cast or splint needed to maintain fracture alignment. As in other parts of the body, missed compartment syndrome is a tragedy ( Fig. 6.3 ).
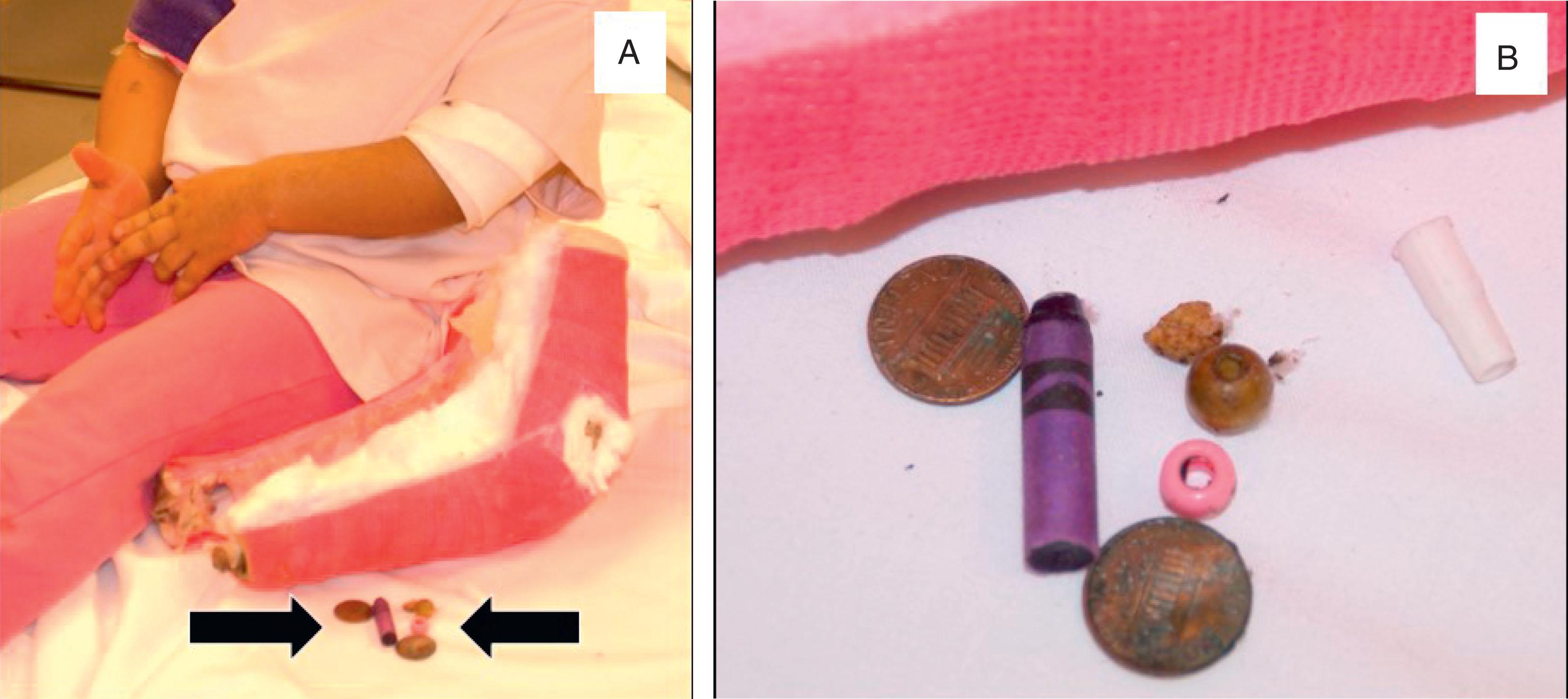
The most common definitive treatment of distal radius and ulna fractures is cast treatment, and thus these fractures become the most common backdrop for cast-related complications. These complications include a range of cast application and cast removal issues, as well as a certain number of patient behavioral challenges ( Figs. 6.4–6.6 ). Due to the strong transition away from plaster casting materials, this discussion is focused on fiberglass casting. A key aspect of the safe application of fiberglass casting materials is the stretch-relax technique described by Davids and coauthors, an article that should be required reading for all orthopaedic surgery residents and orthopaedic technicians (cast technicians) in training. A robust literature exists on this topic that can help the orthopaedic surgeon avoid most of these problems and properly counsel patients and families about the others.

The acute care of displaced distal radius and ulna fractures involves balancing concern for maintaining (holding) reduction and anticipating (accommodating) postreduction swelling. A time-honored approach to this issue is the sugar-tong splint, which minimizes circumferential constriction while allowing for three-point molding. A variety of researchers have shown that sugar-tong splints are as effective as casting in the early treatment of forearm fractures. If the surgeon opts for plaster sugar-tong splinting, care must be taken that dip water is not excessively hot, appropriate padding is used, and the splint is cut to proper length in order to avoid fold-overs at the ends that may increase risk of thermal injury. Some practitioners may still choose to be acute casters (rather than sugar-tongers), and this opens up the issue of whether or not to split the cast in some fashion. If deemed necessary, dorsal or volar univalving has been shown to be ideal for structural reasons, along with the possible addition of spacers to maintain the spread position. However, two separate randomized controlled trials cast doubt on the practice of univalving/bivalving because they showed no significant difference between acute casting of reduced pediatric forearm fractures with or without cast splitting. Minimizing univalving and bivalving of casts also helps decrease the likelihood of cast saw–related injury. Waterproof cast lining has been shown to demonstrate significant constricting properties (even after bivalving a cast), therefore, waterproof cast padding is not recommended for the acute treatment of fractures that are likely to swell.
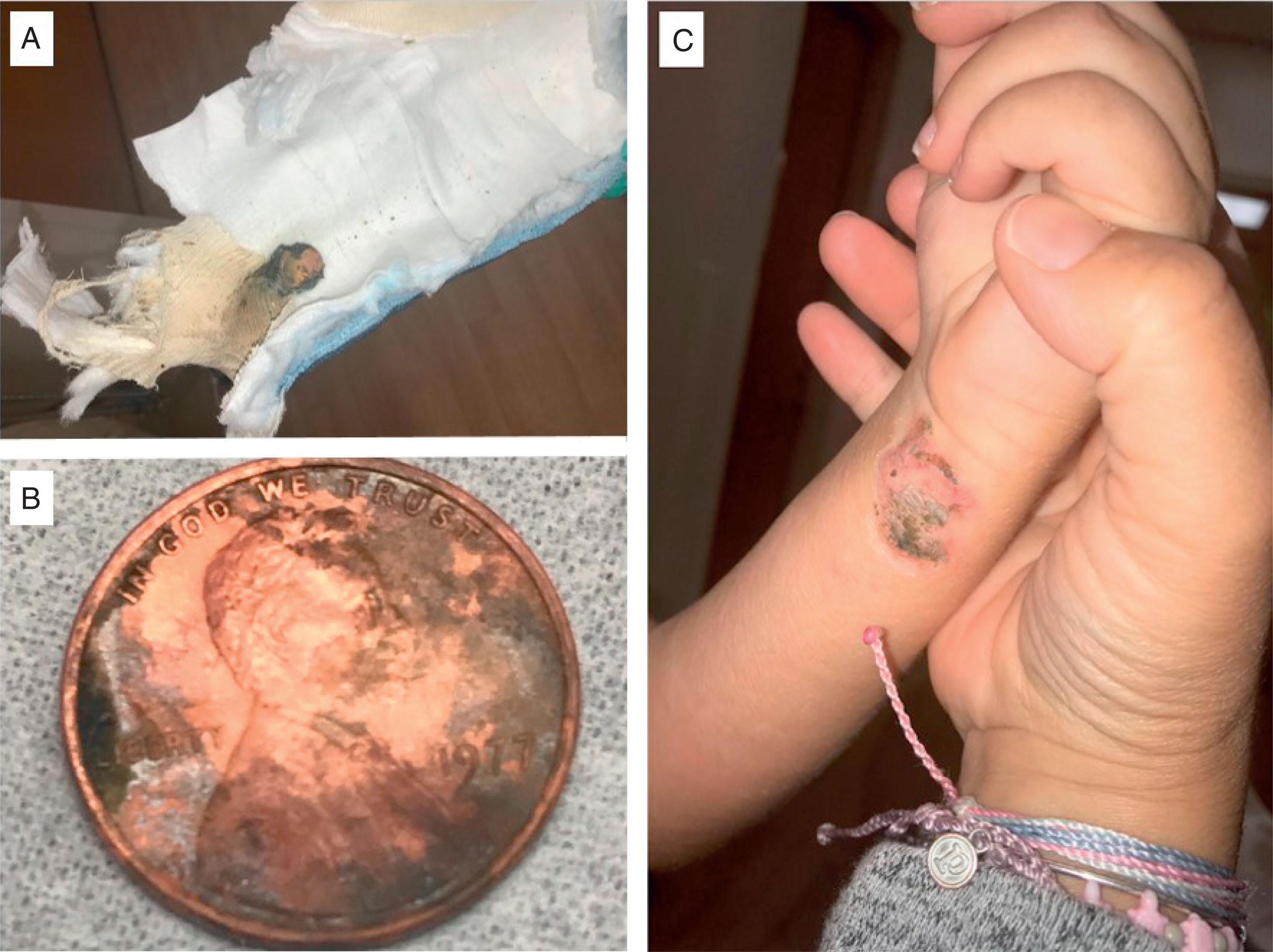
Cast saw–related patient injury occurs at a rate of about 1 in 1000 cast saw events. These injuries are usually cast saw cuts or cast saw burns. From a practical standpoint cast saw cuts to the patient’s skin are usually due to a combination of inadequate cast padding and poor cast saw technique (too much drag and not enough bounce). In addition to raising questions about adequacy of cast padding, cast saw burns are associated with allowing an active cast saw to linger too long in one place ( Fig. 6.7 ). Prevention of these cast saw complications focuses on perfecting initial cast application technique and optimizing cast saw maintenance and cast removal technique. Research has indicated that four layers of cast padding can decrease measured skin temperatures during cast removal (whether plaster or fiberglass). Running the cast saw with its associated vacuum, as well as wiping the blade down with isopropyl alcohol, decreases blade temperatures. Additional protection is conferred when commercially available flexible ribbons (safety strips) approximately 1 inch in width are placed along the projected cast saw path. Such safety strips can serve this function for cotton-padded or waterproof casting situations. Dull saw blades can be a major problem, and suggested criteria for cast saw blade changes have recently been published ( Box 6.1 ).

Stryker 940 Cast Cutter Saw with Ion-Nitride Blade
Saw without vacuum for plaster = 60 univalves/30 bivalves
Saw with vacuum for plaster or fiberglass = 103 cast removals
Use saw with vacuum whenever possible
These suggested blade changes relate to one type of cast saw, the Stryker saw (Stryker Corp, Kalamazoo, MI). An orthopaedic surgeon, Homer Stryker, MD, invented the oscillating saw in 1947, and the company that bears his name made oscillating saws continuously until 2021, when the company elected to stop production. Many Stryker saws will remain in use, but replacement parts (including blades) will eventually become scarce. New cast saws have appeared on the market, including the so-called Quiet Cast (DeSoutter Medical, Mooresville, NC) ( Fig. 6.8 ).

The two different types of cast padding present two different types of cast complications. As compared to waterproof cast liners, classic cotton cast padding is more strongly associated with an itch factor that may lead patients to pass devices (e.g., coat hangers) under the cast. Strategies for dealing with itching under a cast are presented in Box 6.2 . A prerequisite for waterproof casts is to get them soaking wet at least once a day. In the absence of the lubricating action of the water, the padding tends to excessively anneal to the skin, and this can be problematic at the time of cast removal. A general recommendation is for at least one water immersion session to be at the end of the day so as to allow things to naturally dry overnight. Even in the setting of proper care there may be rare instances of waterproof liner skin reactions. These skin reactions may be either localized and minor or generalized and severe ( Fig. 6.9 ). Our experience with waterproof cast liners has suggested that children with a strong history of eczema appear to be more susceptible to this generalized skin complication, and choosing cotton cast padding may be the better part of valor. Localized acquired hypertrichosis (also known as increased hairiness following cast treatment) is commonly attributed to the increased vascularity of fracture healing. It has been shown that 80% of these hypertrichosis patients will resolve within 6 months.
Scratch same spot on opposite side of body
Blow cool air into cast via hairdryer
Suction air thru cast via vacuum cleaner drapery attachment
Take Benadryl or Atarax
Take a bath/shower (waterproof liners only)
Patients must be told repeatedly to never stick anything into or under the cast!!!

Past concerns about the ability of waterproof cast padding to allow adequate cast molding and maintenance of fracture reduction for distal radius and ulna fractures have been put to rest by the long-term experience of pediatric centers across the United States, as well as published prospective trials. The impact on patient satisfaction and overall function is unmistakable. In addition to creating a certain amount of buoyancy, waterproof liners effectively eliminate the most common cause of unscheduled fracture patient visits (usually to the emergency department): wet casts. An additional level of care (parental oversight) is required to prevent water exposure when plaster casts or cotton-padded fiberglass casts are utilized. Home remedies for this have often involved garbage bags, but a variety of commercially available devices are now on the market to meet this need. Evidence indicates that a double garbage bag with duct tape approach or one of several commercially available protectors work very well at keeping casts dry during bathing.
Noise is ubiquitous in busy fracture clinics, often with multiple cast saws operating simultaneously. These devices are chainsaw loud. The noise (and the anxiety they may create) is not always innocuous, with documented increases in pediatric heart rate and even a cast saw noise–related death having been reported in an 18-month-old child with cardiomyopathy. Several devices, such as earmuffs and various types of headphones, have been suggested as ways to mitigate the noise and improve patient experience. A recent study has suggested that measures should be taken to avoid noise exposure to adjacent patients by moving away from the open bay settings commonly used for fracture clinics and increasing the use of closed-door individualized rooms.
Some final cast comments are in order relative to the decision that orthopaedic surgeons must often make about below-elbow casting versus above-elbow casting when treating these distal radius and ulna fractures. At least five separate randomized controlled trials have addressed this specific question. Bohm and his colleagues in Saskatchewan randomized 4- to 12-year-old children with distal-third forearm fractures requiring reduction (growth plate and open fractures excluded) to two different groups. Some 46 below-elbow cast patients (59% had radius and ulna fractures) were compared to 56 above-elbow cast patients (75% had radius and ulna fractures). High rates (that were not statistically different) of need for fracture remanipulation were noted in both groups (31% below elbow and 42% above elbow). Webb and his coauthors (Buffalo, NY) randomized children with distal-third forearm fractures requiring reduction (excluding pathologic and open fractures) who were 4 years of age and older with open growth plates to below-elbow and above-elbow cast groups. Some 53 below-elbow cast patients (13% physeal fractures) were compared to 60 above-elbow cast patients (17% physeal fractures). A total of 4% of below-elbow patients lost reduction, whereas 15% of the above-elbow group lost reduction. Paneru and his fellow Nepalese researchers randomized 4- to 12-year-old children with distal-third forearm fractures (excluding open fractures) to below-elbow and above-elbow groups. They analyzed 43 patients in the below-elbow group versus 42 in the above-elbow group. In total, 2.3% of below-elbow and 9.5% of above-elbow patients needed remanipulation. Seiler and her Swiss coauthors randomized 4- to 16-year-old children to above- versus below-elbow cast immobilization following reduction of their displaced distal radius fractures. With 60 patients in each group, they found no significant difference in loss of reduction between the groups: 17% in the below-elbow group versus 25% in the above-elbow group. Finally, Colaris et al. from the Netherlands randomized minimally displaced metaphyseal fractures in 3- to 11-year-old children to above- (31 patients) or below- (35 patients) elbow casting, with 32% of “aboves” and 14% of “belows” requiring remanipulation.
Pediatric orthopaedic common sense, as well as published research, has shown the obvious: that children can do far less in an above-elbow cast as opposed to the below-elbow variety. Therefore the interested practitioner has more than enough evidence to routinely choose below-elbow casting for these patients. However, at the discretion of the family and the orthopaedic surgeon, an above-elbow cast can certainly act as an activity-modifying device. As patient care must be tailored to the needs of the individual, the above-elbow cast decision may be operationalized for those children considered to be super active/likely noncompliant. This would be in an attempt to minimize activities that the child might engage in that would increase the likelihood of fracture displacement in the cast.
Early loss of alignment of a previously well-reduced distal radius or distal radius and ulna fracture is disappointing to orthopedists and parents alike. At times there seems to be an explanation (e.g., new fall, premature splint removal by child/family), but most often there is no clear reason. Parents must be told ahead of time that follow-up visits include a screening test called an x-ray, and this is aimed at identifying a “disease” called fracture malreduction. Early detection allows for proper early intervention. It is a useful analogy. The importance of educating the parents and actively involving them in a shared decision-making process around their child’s fracture cannot be overstated.
A completely accurate speech including evidence-based quotes about bone remodeling and Mother Nature can be delivered to parents during the early follow-up visits (before any cast or splint is removed), and yet when the cast or splint does come off for the first time there are gasps of horror ( Fig. 6.10 ). To paraphrase another Sir John Charnley quote: “When the parent sees a crooked wrist they will hate the doctor even more than if the doctor had done this to the parent themselves, because the parent’s earlier trust has been violated and the doctor has done this to their child.” Avoiding this scenario requires the previously mentioned education and shared decision-making, as well as careful and early unveiling of the child’s wrist so all can see/inspect its clinical appearance (preferably from multiple angles) ( Fig. 6.11 ), making it clear ahead of time that obvious radiographic imperfections often are barely discernable (or not discernable at all) when the child’s arm is visualized. This can be immensely reassuring to the parent, building their trust and supporting the pediatric orthopaedic concept that “I treat patients, not x-rays. X-rays help me make decisions about how to treat patients.”
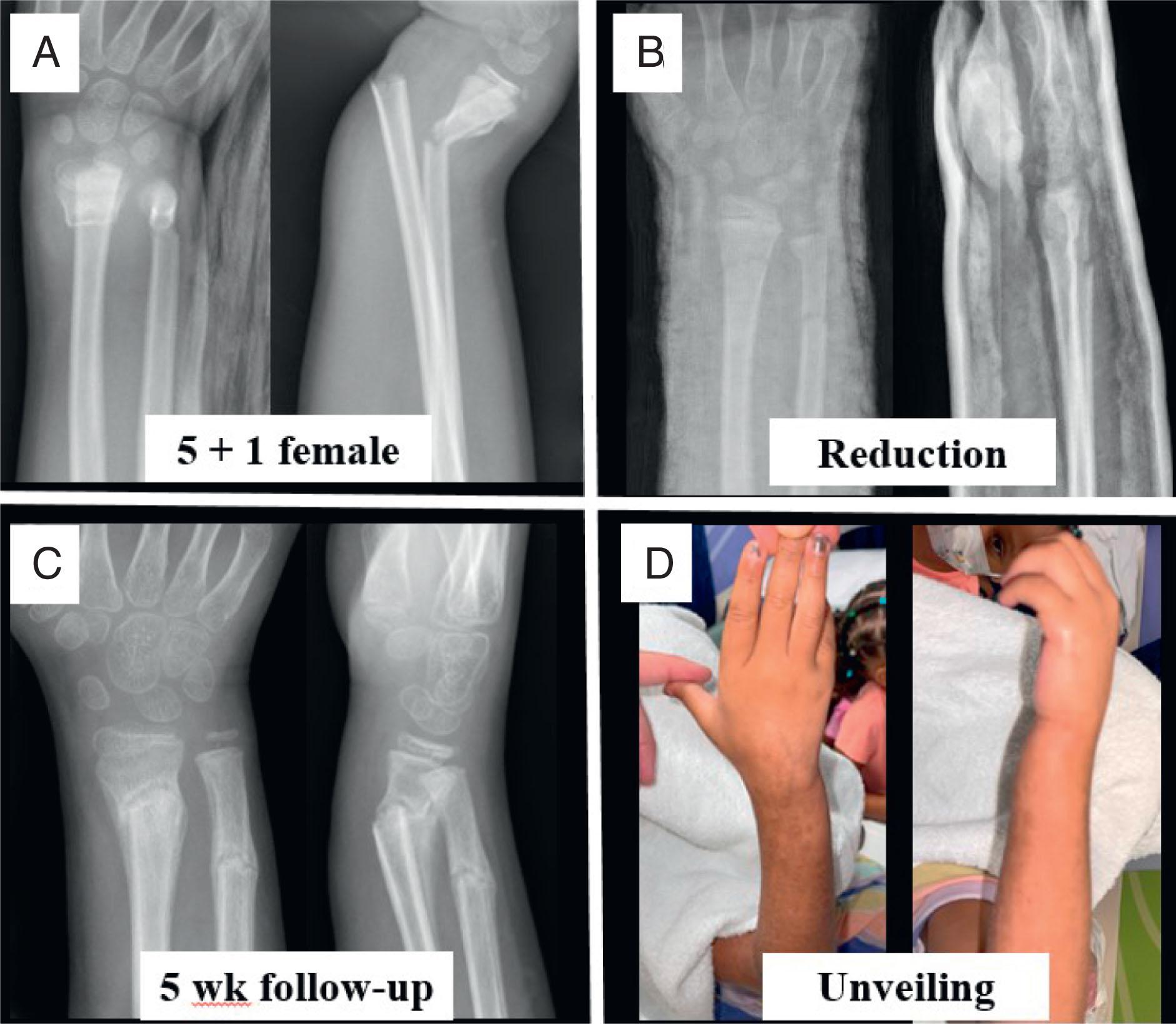
The truest definition of the amount of radiographic deformity that requires intervention is virtually any radiographic deformity associated with clinical deformity that the parent is convinced they can see and are bothered by. This decision can only be arrived at by performing the previously mentioned “unveiling.” It has been suggested by some authors that, in children less than about 10 to 12 years of age, isolated sagittal plane angulation of about 15 degrees does not require any reduction. Survey data from hand, pediatric, and general orthopaedic surgeons has revealed significant variation in opinions as to how much pediatric distal radial fracture imperfection is acceptable ( Table 6.2 ). This research highlights the influence of both patient age and specialty-specific tendencies upon the treatment of distal radius fractures in children. Literature-based recommendations do exist. Because the parents neither have read nor care about your summary of this research, they wish to know what is the best treatment for their child. Thus the early fracture treatment goal becomes achieving and maintaining acceptable alignment that satisfies both the doctor and the parents.
| <9 years old | ≥9 years old | |
|---|---|---|
| Hand Surgeon | 88% | 58% |
| Pediatric orthopaedic surgeon | 90% | 64% |
| General orthopaedic surgeon | 69% | 29% |
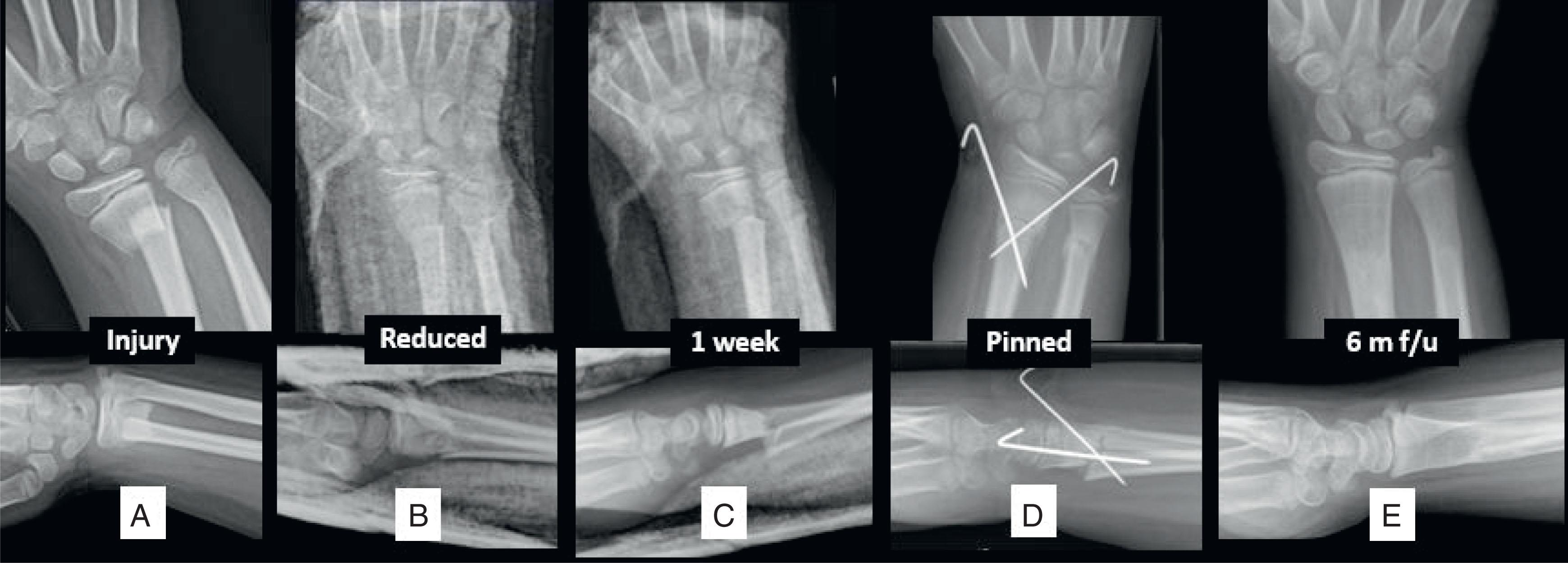
When the complication of significant metaphyseal fracture malalignment occurs early in fracture treatment (usually within the first couple of weeks), several treatment options are available to the orthopaedic surgeon. An appropriate remodeling speech may be delivered to receptive parents, along with collective trust being placed in Mother Nature (with the caveat that, if at the end of 1 year satisfactory remodeling has not occurred, surgery remains an option). Cast wedging may be undertaken in the outpatient clinic. Following cast removal where unveiling has produced a negative parental reaction, a new effort at reduction can be undertaken as part of recasting (also in the outpatient clinic). Finally, if other options are not viable or if the deformity is severe and/or the healing response somewhat advanced, repeat closed reduction (open reduction if indicated) and Kirschner wire internal fixation remains an alternative ( Fig. 6.12 ). It is amazing how rarely this is actually needed. The completely displaced radius with intact or relatively intact ulna is a notorious fracture pattern that is difficult to reduce and is associated with early loss of reduction. Although extremely rare, it should not be forgotten that pinning of such fractures exposes the patient to new categories of complications: infection and nerve injury. More advanced fracture callus formation may require true osteoclasis with or without intrafocal pinning assistance.
At least four French centers have advocated for percutaneous callus osteoclasis (“calloclasis”) when there is concern for malunion in the early healing phase. In a retrospective multicenter series of 21 patients who presented with distal radius malunion at 2 to 6 weeks from injury, the authors reported uniform success with this technique. Under fluoroscopic guidance, a pin is inserted through a small incision to the fracture site, where multiple perforations are performed in postage stamp–like manner. The pin is then advanced intrafocally once the fracture is mobile, and a closed reduction maneuver performed via levering on the pin. The pin is finally advanced through the far cortex of the metadiaphysis to provide stabilization. A standard period of immobilization and subsequent bedside pin removal may follow.
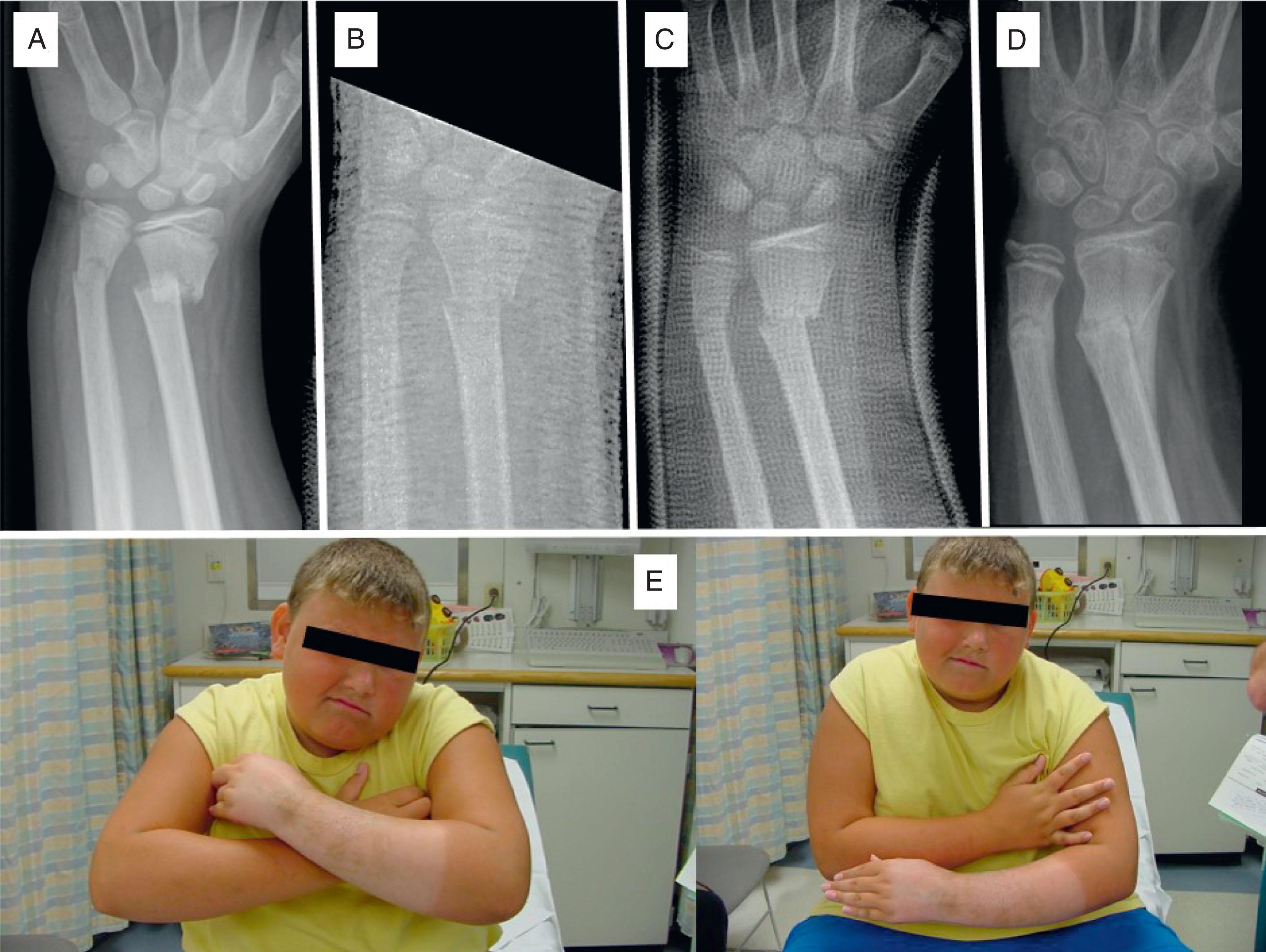
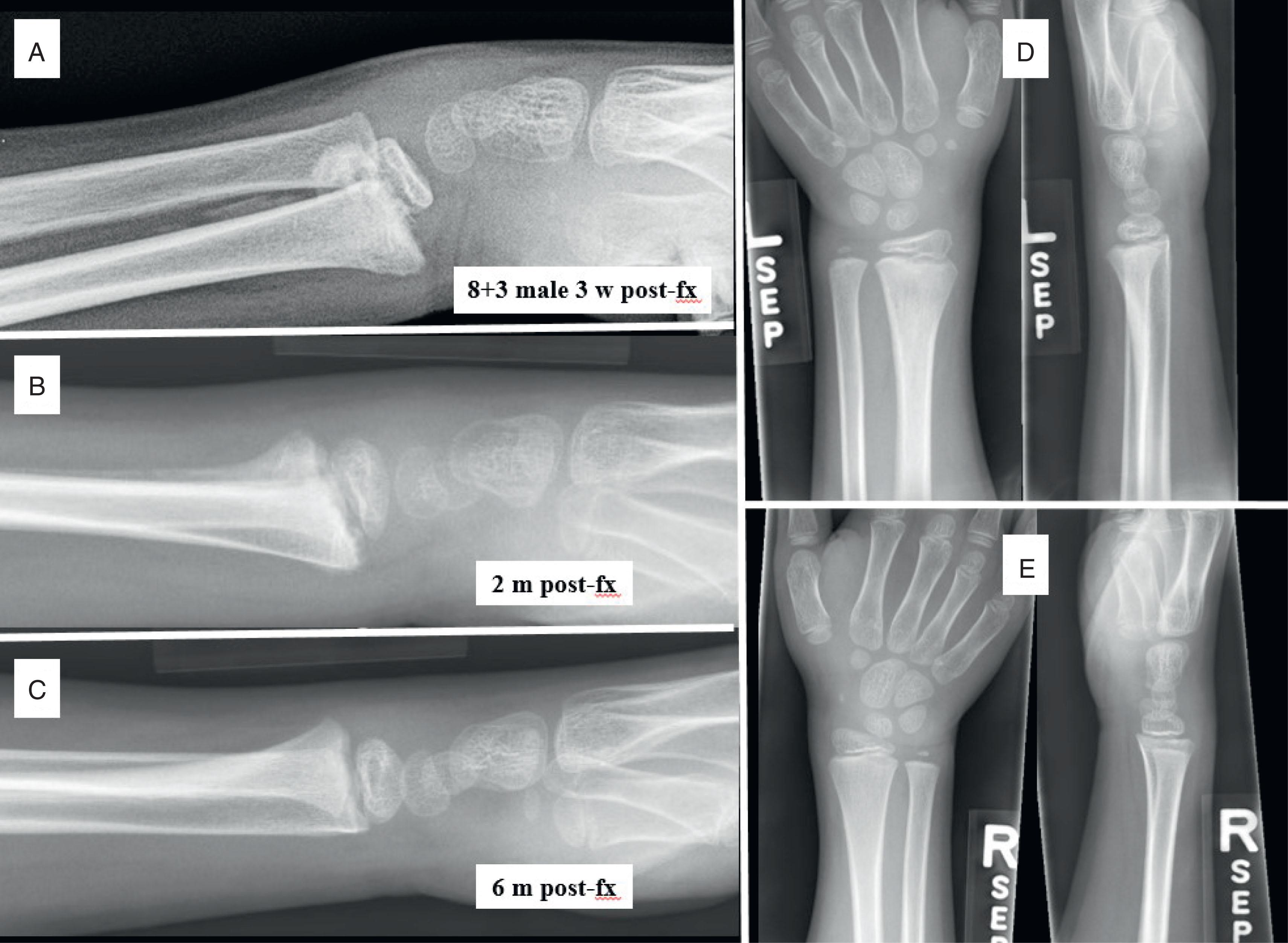
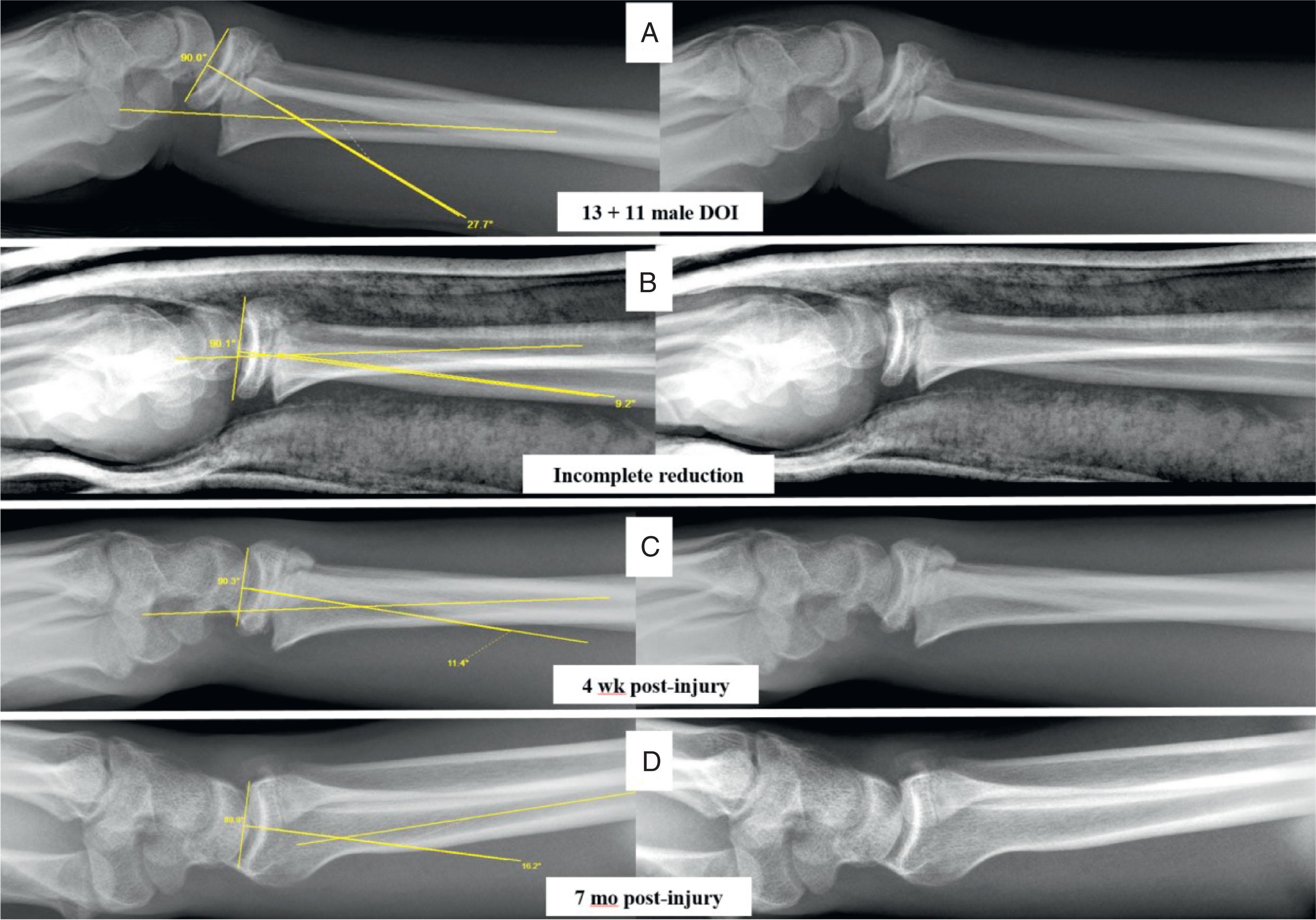
Special mention of unreduced distal radius growth plate fractures or those with early residual malalignment is in order. Cannata et al. reported that this loss of otherwise well-reduced distal radius growth plate fractures occurs at least 16% of the time. Those in children with wide open physes and those nearing skeletal maturity demand very different treatment approaches. The remodeling potential of the distal radial growth plate of a young patient (typically <10 years of age) borders on extreme. Certainly up to 50% translation on the lateral can be expected to remodel completely ( Fig. 6.13 ). The distal radius does this so reliably that, with virtually no exceptions, the strong recommendation is to not attempt fracture reduction of displaced growth plate fractures beyond 7 to 10 days of injury. This is based on fear of excessive fracture manipulation creating a distal radius growth arrest. By the same token the older patient nearing skeletal maturity presents the opposite problem: very limited remodeling potential in a patient who paradoxically still has an open growth plate. If anything other than anatomic alignment of a displaced distal radius growth plate fracture is not achieved in a girl 12 years of age or older or a boy 14 years of age or older, then remodeling should not be expected ( Fig. 6.14 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here