Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
When evaluating a patient with developmental dysplasia of the hip (DDH), there is a standardized treatment protocol that is followed prior to pursuing closed reduction of the hip. It is important to take a detailed history, as not all patients should undergo bracing or closed reduction. This is particularly true for those with stiff, teratologic dislocations such as in arthrogryposis or for those with excessive ligamentous laxity, which will likely remain unstable with closed treatment. Infants who are not following the typical developmental timeline may need to be considered for genetic testing, as hip dislocations are a common feature in a number of genetic conditions. For most centers in the United States, the Pavlik harness is the recommended first-line treatment for persistent dysplasia, subluxation, or dislocation in all infants younger than 6 months of age. Pavlik harnesses used in this age group are reported to have a success rate between 75% and 97%. These rates of success are dependent on several factors including patient age, clinical reducibility of the hip, time of the diagnosis, and underlying pathologies. Possible complications of this treatment modality include skin breakdown, avascular necrosis (AVN) of the femoral head, and femoral nerve palsy. Studies have demonstrated that excessive hip flexion in the harness, larger infants, and higher-grade hip dislocations are risk factors for developing a femoral nerve palsy. Early recognition and management of this complication are critical, as the occurrence is strongly predictive of failure of treatment and increased likelihood of the need for surgical intervention. If treatment with a Pavlik harness fails to reduce or stabilize the hip, an effective second-line treatment is a rigid abduction orthosis, such as an Ilfeld brace. Ilfeld bracing has been shown to successfully improve DDH in approximately 80% of failed Pavlik cases, with fewer infants developing AVN than in closed reduction. For those infants who do not respond to a harness or rigid bracing, or for those infants who present beyond 6 months of age, closed reduction under general anesthesia with hip spica casting is often the next step in management.
Appropriately assessing preoperative patient characteristics may help predict outcomes following closed reduction. Although patient age and initial clinical reducibility of the femoral head impact the rate of success of bracing therapy, studies have demonstrated there is no impact on overall success for closed reduction. However, the upper age limit for closed reduction is controversial, and it has been proposed that this procedure can be performed up to approximately 18 months of age. After this age, open reduction with a pelvic osteotomy should be considered due to a diminished remodeling capacity of the acetabulum and an increased likelihood of residual dysplasia. While an attempt at bracing is important in eligible patient populations, a history of orthotic bracing was shown to have no influence on the outcome of a closed reduction. For patients who have failed bracing, however, one should consider an underlying genetic condition or excessive ligamentous laxity, especially in the presence of abnormal facies and/or delays in gross motor development.
Evaluation of infants with dysplastic hips can be performed by using the Barlow and Ortolani maneuvers. The Barlow maneuver is conducted by adducting the hips to midline and applying a posterior force to evaluate for subluxation. A notable hip clunk, or positive Barlow, correlates with femoral head subluxation and reveals underlying acetabular instability. In contrast, the Ortolani maneuver is conducted by abducting the hips while applying upward pressure at the greater trochanters. While these maneuvers are important for initially evaluating dysplastic hips, Sankar et al. revealed that preoperative femoral head reducibility does not impact closed reduction outcomes. However, other studies have reported that a negative Ortolani sign has increased risk of open reduction.
As children get older, these examinations have decreased sensitivity and specificity for hip dysplasia because of muscle development and resultant contracture around the hip joint. Instead, clinicians should evaluate for altered hip abduction, Trendelenburg gait, leg length discrepancies, or positive Galeazzi sign. For any patients who have positive examination findings, further evaluation via radiographs is warranted.
A systematic approach to the use of imaging in infantile DDH is imperative in stratifying patient outcomes and guiding treatment and timing of follow up. For infants who are under 4 months of age, the imaging modality of choice is ultrasonography. Due to the cartilaginous nature of the infant hip, this imaging modality allows for clear visualization of the relative locations of the femoral head, acetabulum, and acetabular roof. Although the imaging can be performed in both static and dynamic view, the vast majority of hip pathology can be appreciated in a static coronal flexion view.
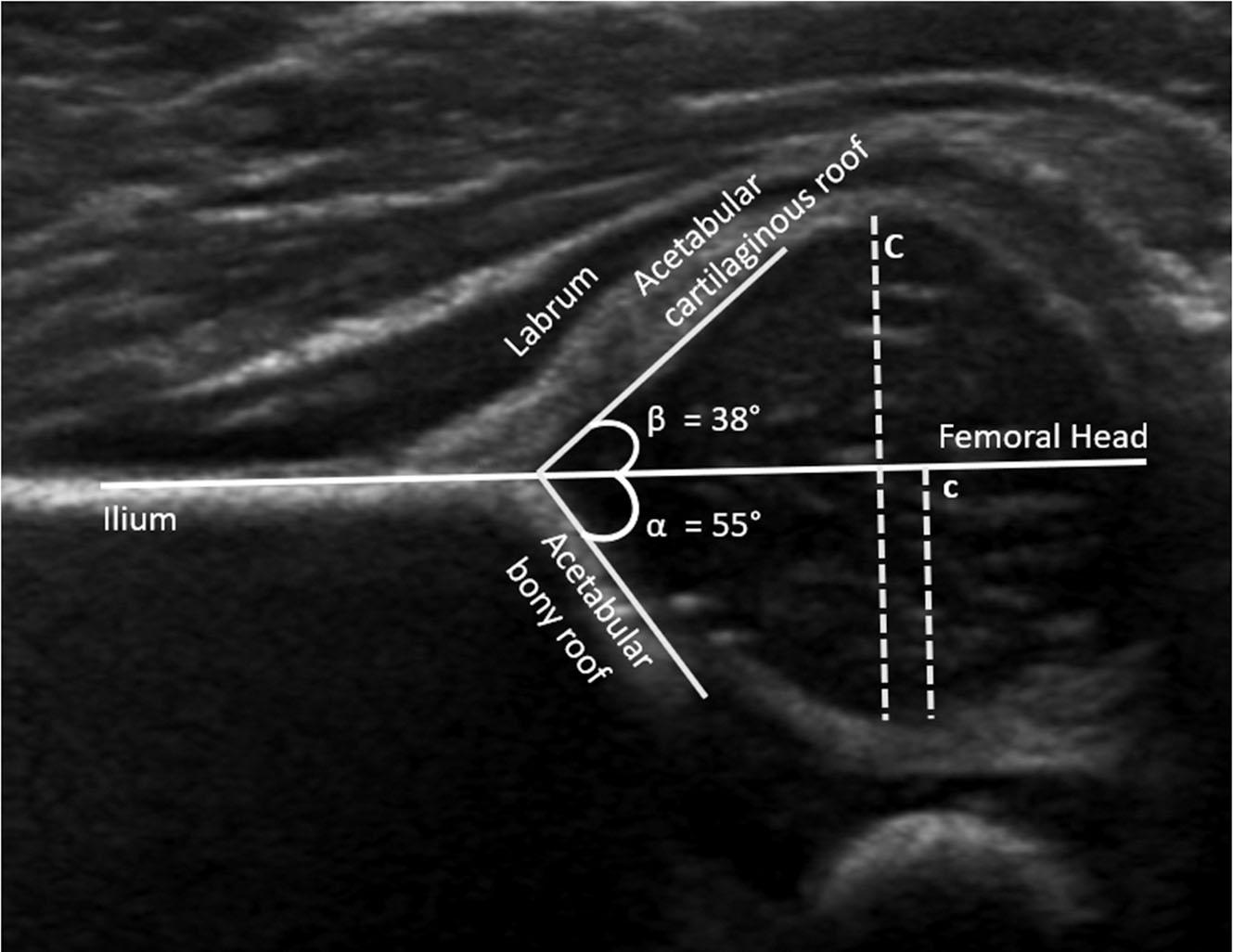
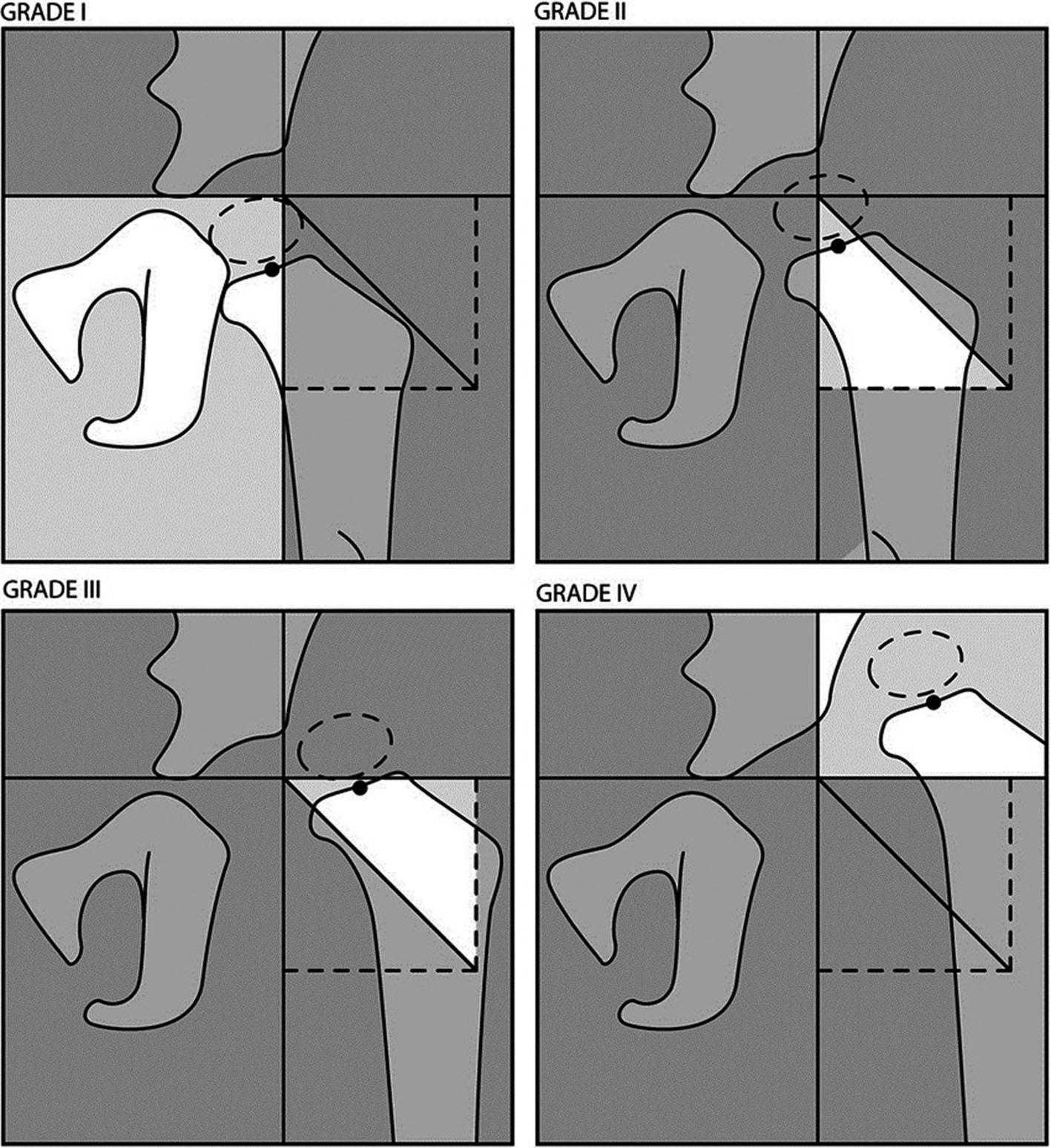
The coronal flexion view should be carefully assessed for femoral head coverage, bony acetabular anomalies, and the specific alpha and beta angles between the acetabulum and ilium, and ilium and labrum, respectively ( Fig. 26.1 ). Graf classifications are a measure of overall severity of disease and take into account the preceding anatomic evaluations ( Table 26.1 ). This classification system is useful to guide treatment recommendations. Previous studies have demonstrated specific radiographic features, such as children with Graf IV hips on initial ultrasound (US) and preoperative International Hip Dysplasia Institute (IHDI) grade III–IV radiographic dislocations ( Fig. 26.2 ), increase the likelihood of failing closed reduction and requiring a future open reduction.
| Graf Classification | ||||
|---|---|---|---|---|
| Class | Alpha Angle | Beta Angle | Description | Treatment |
| I | >60 degrees | <55 degrees | Normal | None |
| II | 43–60 degrees | 55–77 degrees | Delayed ossification | Variable |
| III | <43 degrees | >77 degrees | Subluxated | Pavlik harness |
| IV | Unmeasurable | Unmeasurable | Dislocated | Pavlik harness or closed vs. open reduction |
Ultrasonography can be used for both initial infant screening of DDH and monitoring of patients with DDH undergoing active treatment until around 4 to 6 months of age. After this time, the femoral head ossific nucleus is visible radiographically, and radiographs become the preferred method of evaluating and monitoring DDH ( Fig. 26.3 ). The radiographic presence of the ossific nucleus was historically regarded as having a protective role against developing AVN. Recent studies have shown there is not an association with the size of ossific nucleus and AVN, making the benefit to delaying a closed reduction until femoral head ossification unclear. While the protective impact of ossification center remains uncertain, Wu et al. recently demonstrated that the diameter of the femoral head negatively correlates with risk of AVN, with a larger femoral head showing lower risk of AVN after closed reduction.
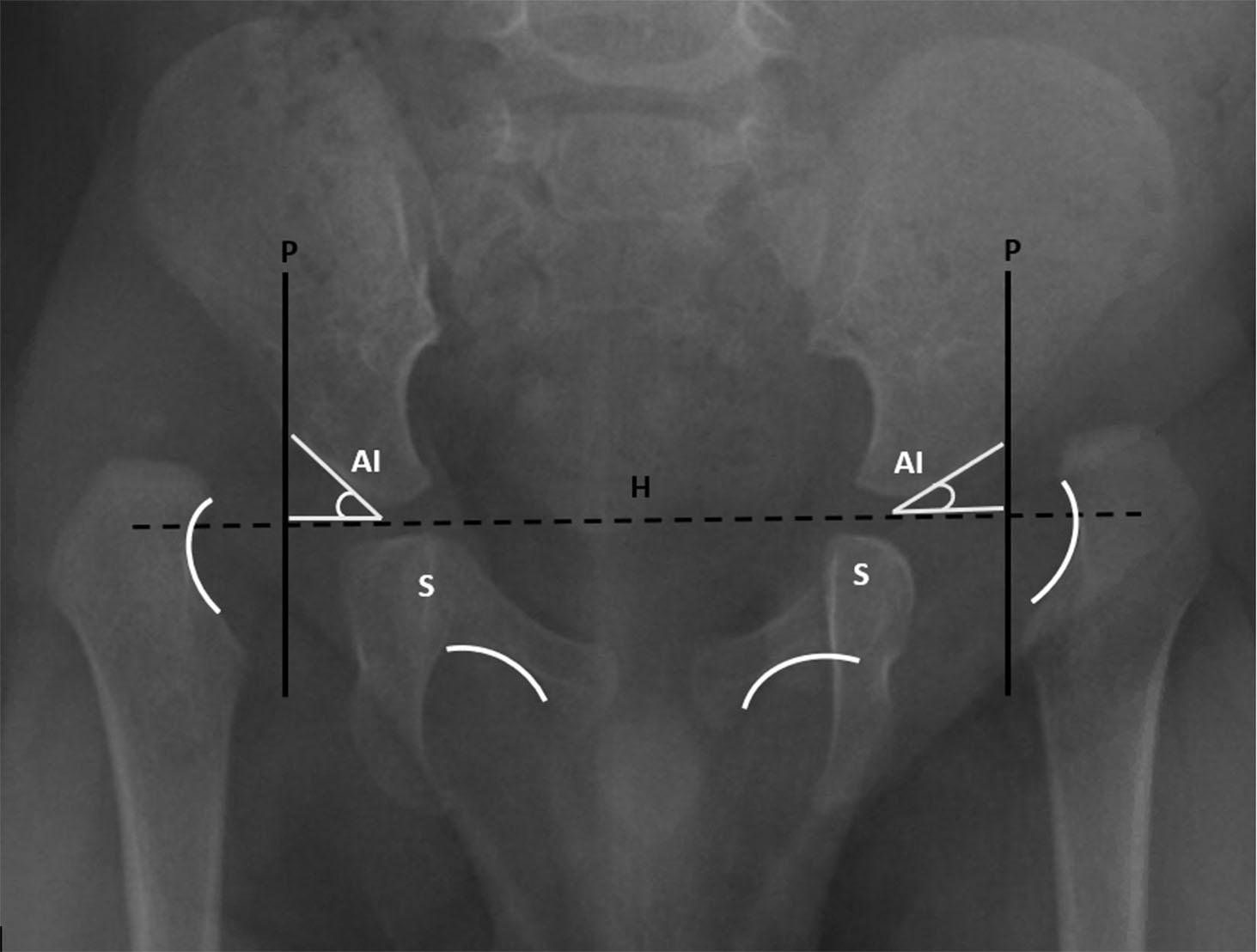
Another radiographic measure that predicts the success of closed reduction is the acetabular index ( Fig. 26.3 ). Li et al. revealed that the acetabular index is the best predictor of final radiographic outcomes in DDH treated by closed reduction. Repeat surgery to prevent late residual acetabular dysplasia was indicated for patients who had an acetabular index greater than 28 degrees 1 year following closed reduction or an acetabular index greater than 25 degrees 2 to 4 years after closed reduction. For patients with satisfactory outcomes after closed reduction, the acetabular index can improve until around 7 years after surgery, whereas those with unsatisfactory outcomes had improvement up to 4 years postoperatively.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here