Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Septic arthritis of the hip can be a devastating process to the pediatric patient, and failure to effectively treat may result in severe patient morbidity and create late sequelae to hip function. Septic arthritis of the hip most commonly affects younger children between 2 and 6 years of age, though it may affect neonates and young adults alike. The incidence in the United States is around 1.07 out of 100,000 children, though this is substantially higher in other countries (between 5 and 20 out of 100,000 children). Males are disproportionally affected compared to females, with a male-to-female radio of 3:1. Some 50% of children diagnosed with septic arthritis of the hip are under the age of 2 years.
An age-dependent relationship exists between commonly cultured pathogens and patient age at diagnosis. The majority of cases of septic hip arthritis in the United States are secondary to Staphyloccous aureus , Streptococcus pneumoniae , and Kingella kingae , with S. aureus being the most common. Accurate identification of the infectious organism is critical to preventing complications. For instance, recent data suggest that the presence of methicillin-resistant S. aureus is a significant predictor for requirement of additional surgical procedures in children with osteoarticular infections.
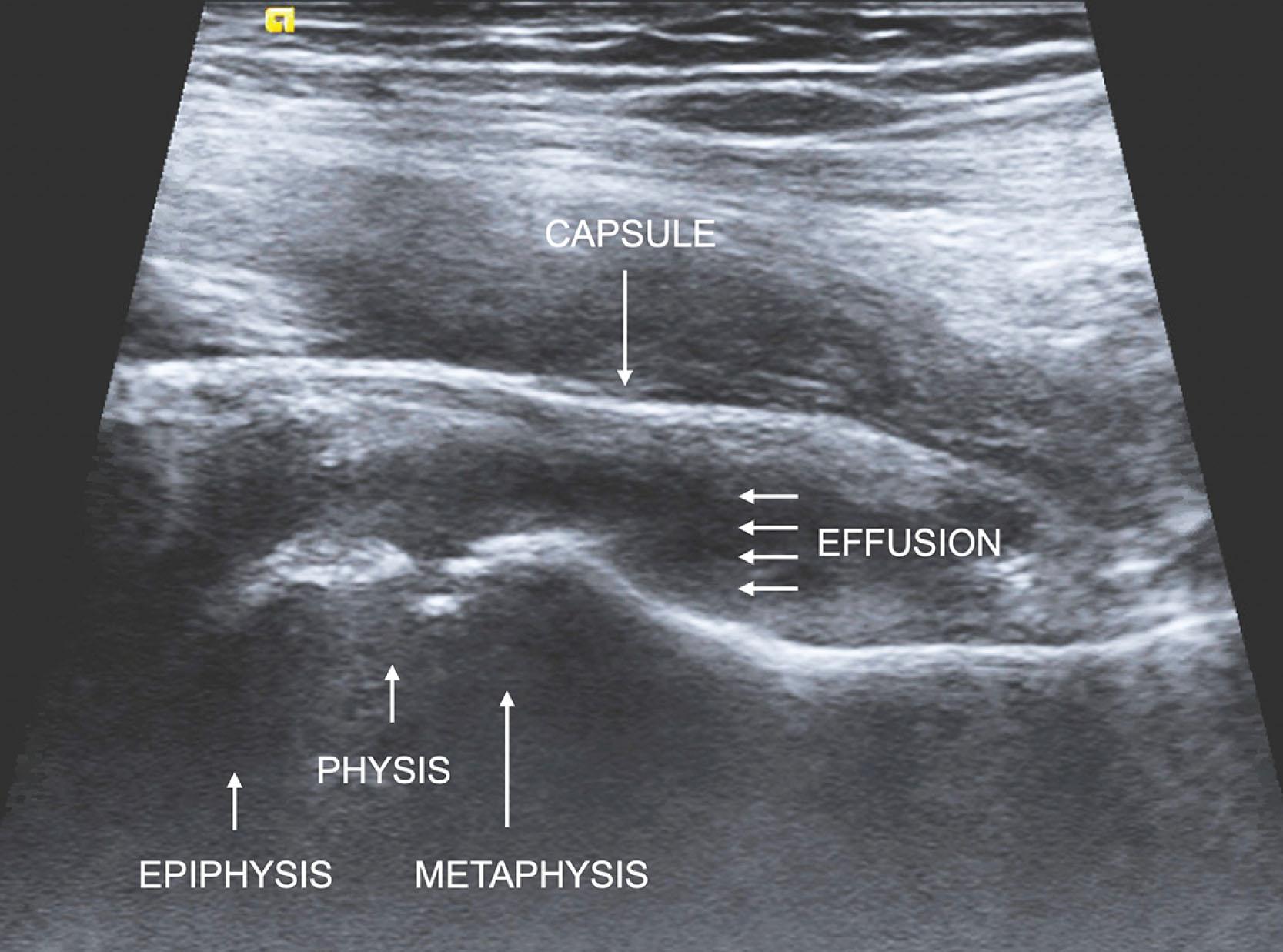
Furthermore, although several mechanisms of inoculation of the hip joint have been described––including hematogenous seeding, direct inoculation, and local spread from proximal femur metaphyseal osteomyelitis––hematogenous seeding appears to be the most common causative pathway. Several means exist to aid in the diagnosis, including clinical history, physical exam, and imaging studies such as magnetic resonance imaging (MRI) or ultrasound ( Fig. 25.1 ). In addition, numerous authors have developed various clinical criteria to aid in the diagnosis, the most common of which include a history of inability to bear weight, fever, elevated erythrocyte sedimentation rate (>40 mm/h), and an elevated serum white blood cell (WBC) count (>12,000 cells/mm 3 ). In conjunction with these diagnostic criteria, hip aspiration results––including culture, cell count, and advanced polymerase chain reaction––frequently are obtained and aid in diagnosis.
Despite a thorough understanding of the epidemiology of septic arthritis of the hip in pediatric patients, its pathological process, the common offending organisms, validated diagnostic criteria, and treatment modalities, septic arthritis of the hip may be associated with potentially devastating complications in the pediatric patient, even when appropriately managed. Complications are reported in 10% to 25% of cases of septic arthritis of the hip in pediatric patients. These complications may be related to several different stages of care. For instance, complications in management of septic arthritis of the hip may occur early in the diagnosis stage or years later after operative intervention. Specifically, complications may be divided among the following treatment stages: diagnosis, intraoperative care, early postoperative care, and late postoperative care ( Table 25.1 ). In addition, unique complications related to psychological and social (“psychosocial”) concerns may also present distinct treatment issues that must be addressed for an optimal clinical outcome. Finally, recognizing and avoiding complications before they occur is critical.
| Phase of Care | Complications |
|---|---|
| Preoperative | Delay in diagnosis, missed intramuscular abscess or osteomyelitis, misdiagnosis, missed diagnosis |
| Intraoperative | NV injury, incomplete debridement, cartilage or labral injury, femoral head blood supply injury |
| Early postoperative | Hematoma, wound complication, return to OR, medication reaction, sepsis, multiorgan failure, death |
| Late postoperative | Subluxation, dislocation, late recurrence, deformity, physeal separation, femoral head AVN |
| Psychosocial | Prolonged hospitalization, illness-related anxiety, lost socialization and school experiences, family stressors |
A delay in diagnosis of septic arthritis of the hip represents the earliest major complication during the diagnostic phase of care. A delay in presentation may often occur, making expedient diagnosis of a septic hip joint more critical to an excellent outcome. The differential diagnosis for a child presenting with lower extremity pain and limp is broad, and includes traumatic, infectious, oncologic, and abuse-related diagnoses. All of these must be considered and appropriately ruled out in the process of considering a diagnosis of septic arthritis of the hip. A thorough clinical history and physical exam will help narrow the initially broad differential diagnosis. Differentiating septic arthritis from transient synovitis may be especially challenging. As mentioned, several studies have demonstrated various clinical predictors that may be used to differentiate septic arthritis from transient synovitis and other common pediatric hip pathologies ( Table 25.2 ).
| Multivariate Predictor | Regression Coefficient | Likelihood Ratio | P Value | Adjusted Odds Ratio | 95% Confidence Interval |
|---|---|---|---|---|---|
| History of fever | 3.7 | 29.51 | <0.0001 | 38.6 | 10.8–137.0 |
| Nonweightbearing | 3.2 | 10.77 | 0.0009 | 24.3 | 5.6–85.2 |
| Erythrocyte sedimentation rate ≥40 mm/h | 3.3 | 19.09 | <0.0001 | 25.9 | 6.5–112.6 |
| Serum white blood cell count >12,000 cells per mm 3 (12.0 × 10 9 cells per L) | 2.7 | 14.61 | 0.0001 | 14.4 | 4.0–51.5 |
Once laboratory data and imaging studies are obtained and the clinical picture remains suspicious for septic arthritis of the hip, an aspiration is frequently obtained. Although the usual diagnostic threshold for joint fluid aspiration cell count is 50,000 WBCs/mm 3 , some authors suggest that lower values may need to be considered in septic arthritis of the hip in pediatric patients. For instance, one study evaluated children undergoing hip aspirations and found that 17% of patients with cell counts of 25,000 to 50,000 WBCs/mm 3 were ultimately diagnosed with septic arthritis of the hip, demonstrating that clinical intuition is of utmost significance, particularly when laboratory results return cell counts below 50,000 WBCs/mm 3 . Furthermore, hip aspirations with no-volume or low-volume fluid leading to false-negative findings may lead to poorer outcomes. A false-negative aspiration in neonates may lead not only to a delay in treatment but also to subsequent hip capsule perforation with resultant hip instability and extracapsular purulent material collections. Neonates presenting with fewer than 24 hours of symptoms may present with false-negative aspirations, given limited time for effusions to form.
Neonatal sepsis or an identified infection in other joints or areas is an indication for hip ultrasound in infants under 6 months old. Such protocol may prevent a missed septic hip that is often clinically hidden in the neonate.
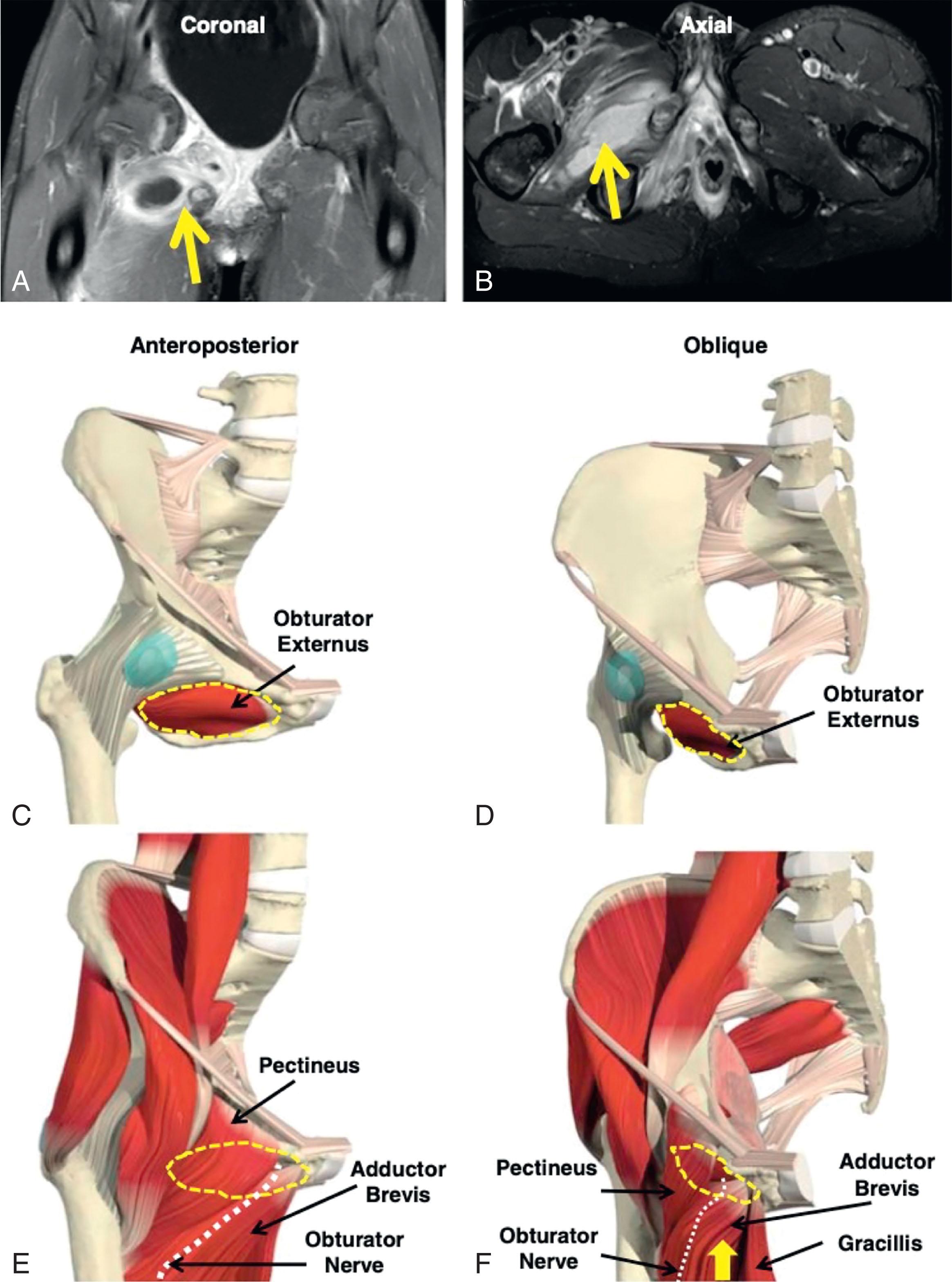
In addition, other clinical entities––intra-abdominal abscess, obturator muscular abscess, infectious pelvic pyomyositis, appendicitis, psoas abscess, osteomyelitis, and spine-related infection––exist that may mimic septic arthritis of the hip ( Figs. 25.2 and 25.3 ). These abscesses may ultimately communicate with the hip joint ( Fig. 25.4 ). In these scenarios, too narrow of a differential diagnosis and too early a focus of clinical workup centered around the hip may result in a delay of other significant infectious diagnoses that may be life-threatening. Toren et al. described a psoas abscess diagnosis delayed by 12 days secondary to an intensive workup of right hip pain for septic arthritis in a pediatric patient. Several other reports exist of delayed diagnosis of various life-threatening infections secondary to inappropriate workup of other pathology, such as septic arthritis of the hip. In patients presenting with clinical exam and laboratory findings concerning for septic arthritis of the hip, one study found the incidence of infection of the muscular tissue surrounding the hip to be greater than twice that of septic arthritis.
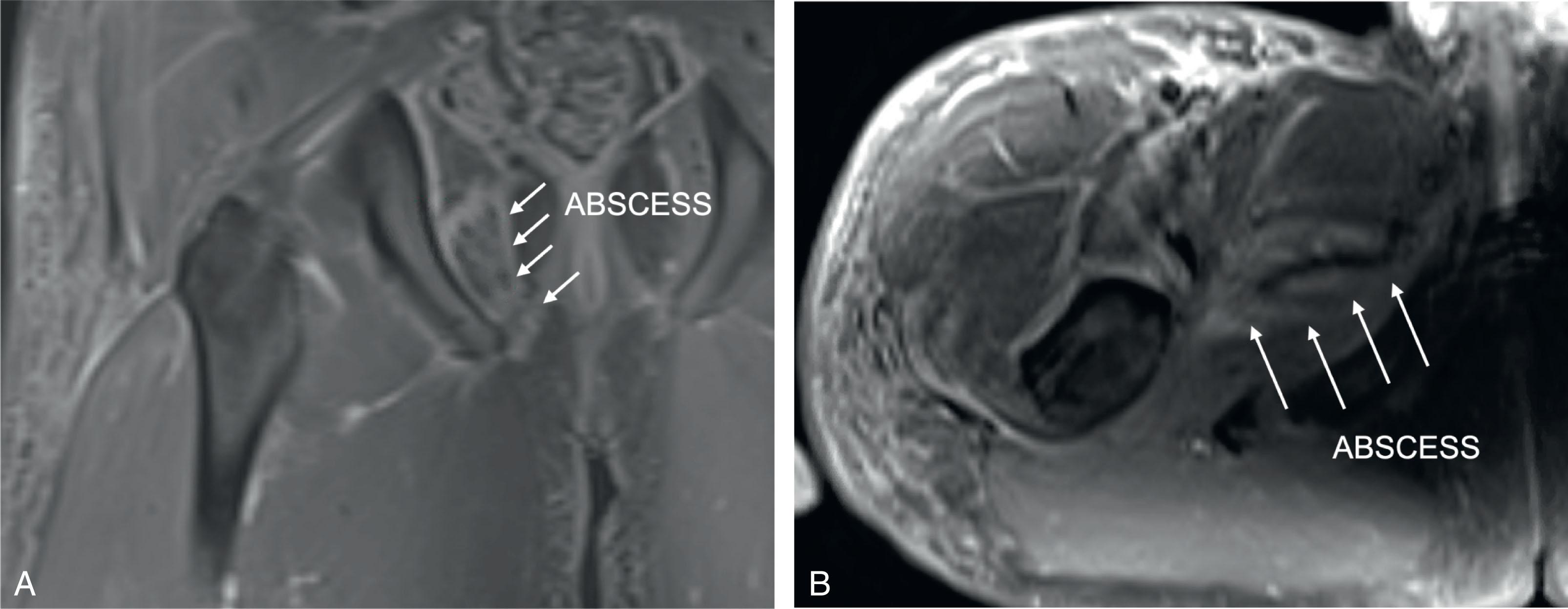
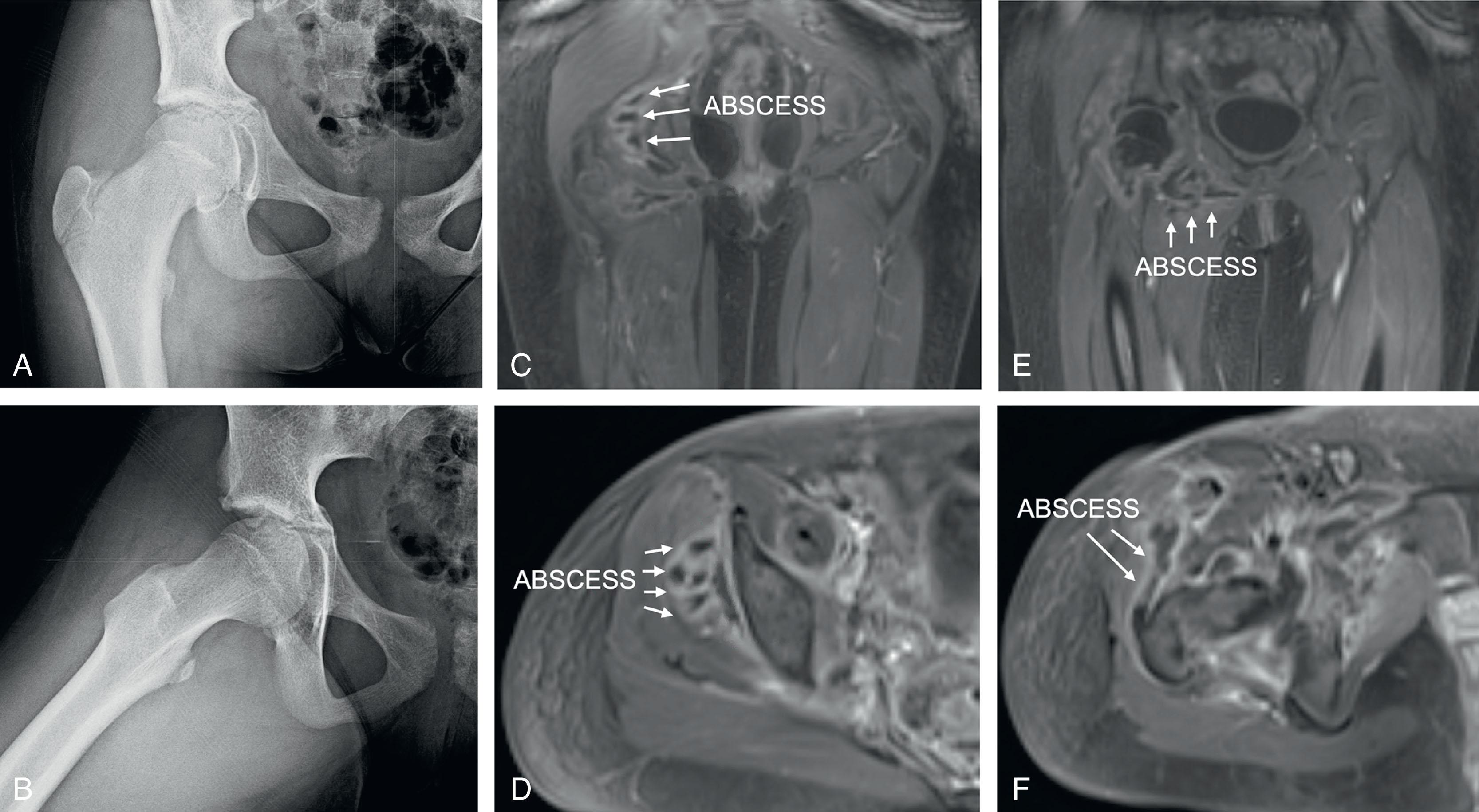
In addition, concomitant muscular and/or surrounding soft tissue infection presenting with an intra-articular hip infection may complicate the clinical scenario. A connection between the iliopsoas bursa and the hip joint exists in approximately 15% of patients and may aid in the spread of infection. Furthermore, a concomitant obturator abscess is a commonly encountered clinical scenario that is diagnosed using MRI and usually managed surgically through a medial approach ( Fig. 25.5 ). Finally, in addition to a delay in diagnosis and the possibility of serious life-threatening infection progression, a missed obturator abscess may also lead to serious late complications such as protrusion acetabula.
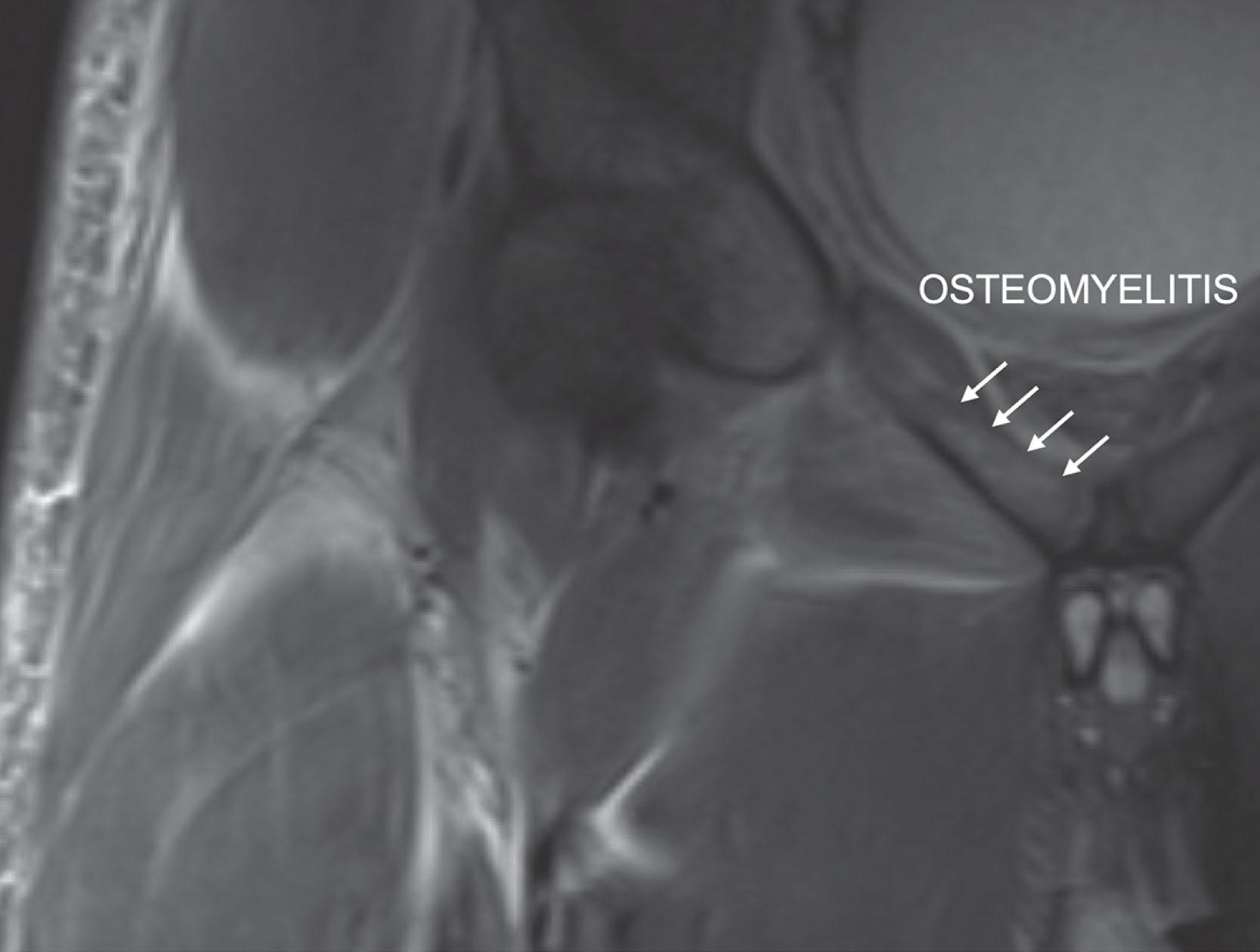
Unfortunately, just as true septic arthritis of the hip in the pediatric patient may masquerade as other infectious pathologies, the reverse is also true, and a reliable diagnostic algorithm and team approach are necessary to avoid the complication of misdiagnosis that commonly results in delayed care and poorer outcomes. For example, in a review of pelvic osteomyelitis, permanent disability (defined as recurrent osteomyelitis or permanent deformity) resulting from an average delay of 12 days was shown to occur in 3.4% of cases. As such, an accurate and timely diagnosis of an infectious pathological process is critical to prevent late disability. In cases of diagnostic uncertainty, advanced imaging (computed tomography, MRI) should be sought to evaluate for perihip infections. Numerous studies have demonstrated the value of a dedicated pediatric musculoskeletal infection pathway with routine use of MRI in the diagnostic workup. Determining the extent of pathology in the preoperative phase is similarly important in predicting prognosis. A recent study demonstrated that septic arthritis with contiguous osteomyelitis portends significantly increased risk of adverse outcomes than primary septic arthritis alone.
Once an accurate diagnosis of septic arthritis of the hip is obtained and the decision to intervene operatively is made, several complications may occur secondary to the operative intervention itself. An anterior Smith-Peterson approach to the hip remains the most widely utilized surgical exposure for adequate hip joint irrigation and debridement. Routine use of tractionless hip arthroscopy has been proposed in some centers, but it requires presence of specialized equipment and familiarity with technique. Commonly encountered complications during the standard anterior approach are rare, though neurovascular injury is possible, particularly with distal extension of the direct anterior approach incision. Specifically, the ascending branch of the lateral femoral circumflex artery and the lateral femoral cutaneous nerve are at risk. Although the incidences of femoral nerve palsy and lateral femoral cutaneous nerve palsy after septic hip irrigation and debridement in the pediatric patient are poorly reported in the literature, they are 1.1% and 11.7%, respectively, in the adult population after employment of the direct anterior approach. Careful surgical exposure and an accurate understanding of anatomy in this region will prevent these complications.
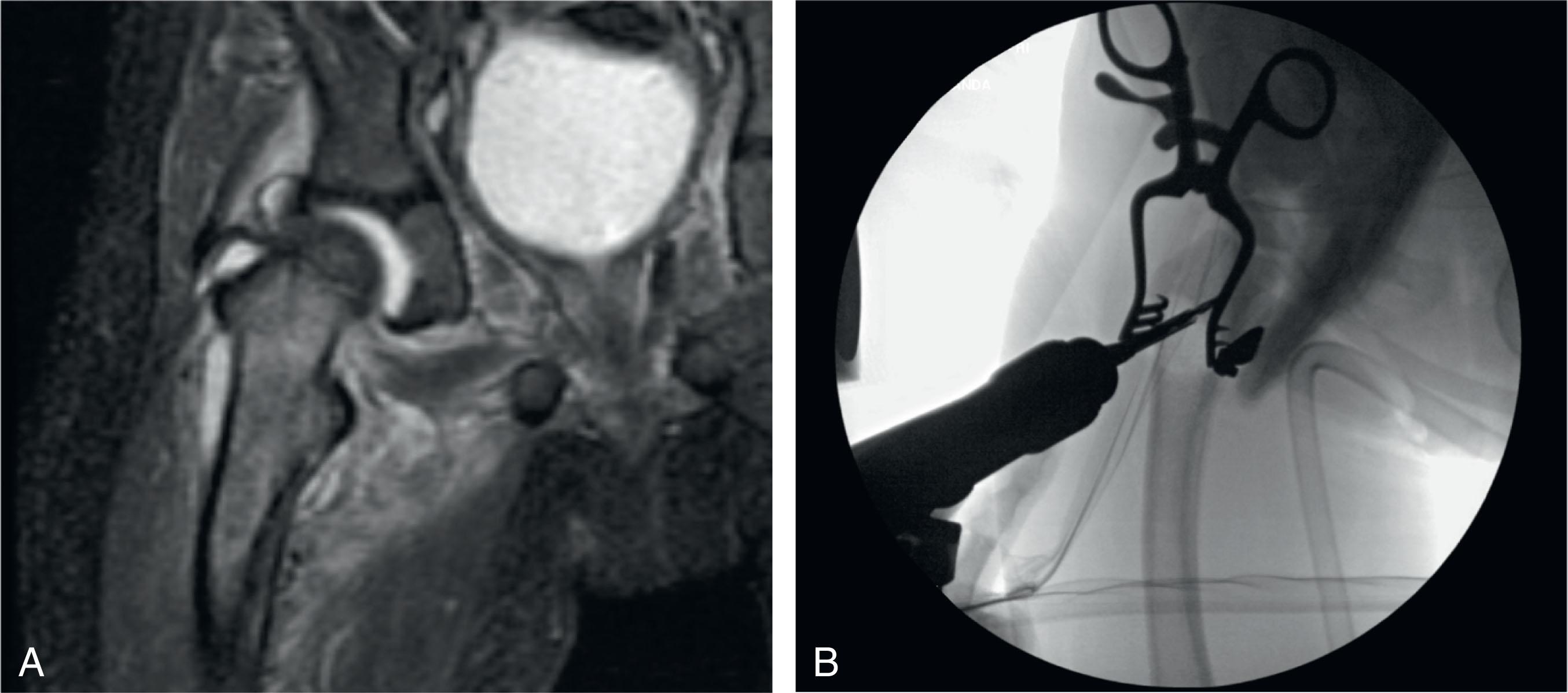
The surgeon must also pay particular attention during joint arthrotomy. Damage to the chondral surface of the femoral head and damage to the labrum are possible and should be avoided. Additionally, incomplete decompression of the joint space and failure to evacuate all purulent material using debridement and copious irrigation may result in acute or chronic recurrence. A thorough analysis of the surrounding tissues and joint space should be done at the index surgery. In addition, preoperative analysis of advanced imaging (MRI) must be done to identify concomitant metaphyseal osteomyelitis that, if present, may be managed by drilling of the proximal femur at time of surgery ( Fig. 25.6 ). Irrigation of the inferior capsular recess is essential. Any associated soft tissue infectious collections should be debrided concomitantly, and advanced imaging should be used preoperatively to evaluate for such associated pathology. After review of all available data, a preoperative plan to address the septic hip joint and surrounding tissue will help limit intraoperative complications.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here