Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
I would like to thank Satyan B. Sreenath, MD for his work on this chapter and figure production
Both benign and malignant tumors may originate within or around the maxillary sinus and hard palate. These tumors may arise from the epithelial surfaces of the oral cavity (hard palate or alveolar ridge) or the sinonasal mucosa (within the maxillary sinus or lateral nasal wall). Tumors that involve the maxillary sinus can also arise from adjacent structures such as the skin, orbit, lacrimal system, infratemporal fossa, ethmoid sinuses, and anterior skull base. Squamous cell carcinoma is the most common malignant histology encountered in the maxillary sinus. The second most common malignant pathology is a variety of adenocarcinomas.
The primary treatment paradigm for all tumors of the maxillary sinus involves surgical resection, once appropriate clinical evaluation and staging have been completed. The exceptions to this management plan are lymphomas or plasmacytomas, which are very radiosensitive tumors and do not require surgery. In addition, symptomatic or rapidly growing benign tumors may often need surgery but do not require obtaining wide margins or having radical resection as a surgical goal. Regarding surgical planning, complete removal of the tumor with negative margins is the goal, but one must also consider concurrent reconstructive planning. Reconstruction depends on the extent of the defect, but the mainstays of reconstructive techniques include palatal obturator or vascular tissue reconstruction. After primary surgery, malignant tumors of the maxillary sinus often undergo postoperative radiation or chemoradiation.
Surgical goals depend on the tumor histology and tumor location.
Types of maxillectomy include:
Infrastructure (mainly used in the treatment of tumors of the oral cavity that involve the maxillary sinus)
Superstructure (mainly used to treat tumors of the anterior facial skin without palate involvement or rarely tumors from the lacrimal system/orbit)
Medial (mainly used to treat tumors from the nasal cavity that come from or extend to the lateral nasal wall such as inverted papillomas)
Complete (primarily used to treat tumors that originate within and fill the maxillary sinus). This chapter will focus on a complete maxillectomy with obturator placement.
Complete with orbital exenteration
Extended (complete that also includes significant adjacent structures such as facial skin, anterior skull base, and/or infratemporal fossa)
Accurate preoperative assessment of the extent of disease is important, and the complementary information provided by computed tomography (CT) and magnetic resonance imaging (MRI) should not be underestimated.
May present with primary symptoms including but not limited to nasal congestion, lesion of the palate or alveolar ridge, epistaxis, facial numbness, abnormal tearing diplopia, or loss of vision. Patients may present with nodal metastasis (<10% of time), although the metastasis rate for squamous cell carcinoma of the alveolar ridge and hard palate may be as high as 35%. Symptoms of advanced disease include trismus, airway compromise, complete loss of vision or ophthalmoplegia, and lower cranial nerve palsies.
A complete examination of the head and neck must be carried out. Special attention should be paid to:
Examination of the oral cavity including the dentition, hard palate, buccal mucosa, and soft palate mobility. Loss of sensation of the palate is an important finding, since it would suggest either perineural spread into the palatine canals or involvement of the pterygopalatine fossa. Trismus is associated with invasion of the infratemporal fossa.
Cranial nerve examination: Special attention should be paid to cranial nerves III, IV, V, and VI, with a focus on testing extraocular motion and infraorbital nerve function.
Eye examination: Hyperglobus may represent lesion expansion and not necessarily invasion; however, severe extra ocular muscle restriction and loss of visual acuity are almost always due to direct intraconal invasion. Abnormal tearing can be due to invasion of the lacrimal system or invasion of the pterygopalatine fossa by disruption of Vidian nerve supply.
Examination of the neck: The rate of metastasis to the cervical lymph nodes is generally low for squamous cell carcinoma (10% to 35%) but can be present. Usually levels 1 or 2 and facial nodes are the levels most commonly involved.
Facial skin changes: Invasion through the anterior wall of the maxillary sinus represents advanced cancer and is important for postsurgical reconstructive considerations.
Nasal endoscopy is also warranted to examine the floor of the nose (nasal side of the hard palate) and the lateral nasal wall. Additionally, involvement of the ethmoid can be identified in the middle meatus. If there is a tumor present in the nasal cavity, endonasal biopsy may be warranted.
Accurate preoperative assessment of the extent of disease is important, and the complementary information provided by CT and MRI should not be underestimated. This will drive the extent of any planned surgery and should be reviewed with the patient so he or she understands the extent of the operation, as well as any functional consequences that should be expected, such as oral competency, eye involvement, potential for vision loss, or hypoglobus.
CT ( Fig. 107.1A ): Defines the bony boundaries as well as bone invasion of the palate and posterior wall of the maxillary sinus or orbital floor
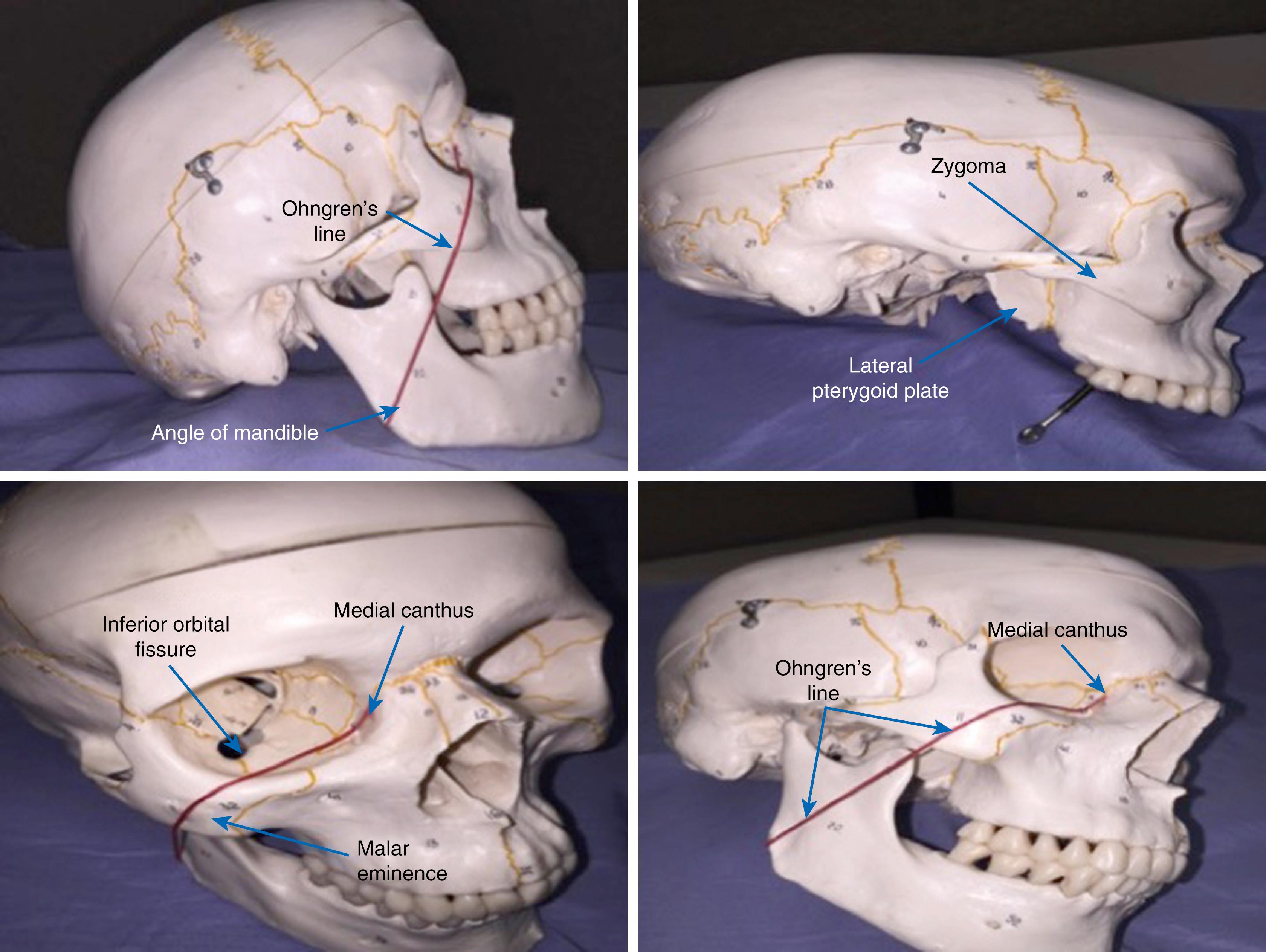
Ohngren’s line ( Fig. 107.2 ): An imaginary line drawn from the medial canthus of the eye to the angle of the mandible. It divides the maxillary sinus into an anterior/inferior portion and a posterior/superior portion. This line helps give relative prognostic value (with anterior/inferior being better) as well an idea of adjacent structures at risk for potential spread.
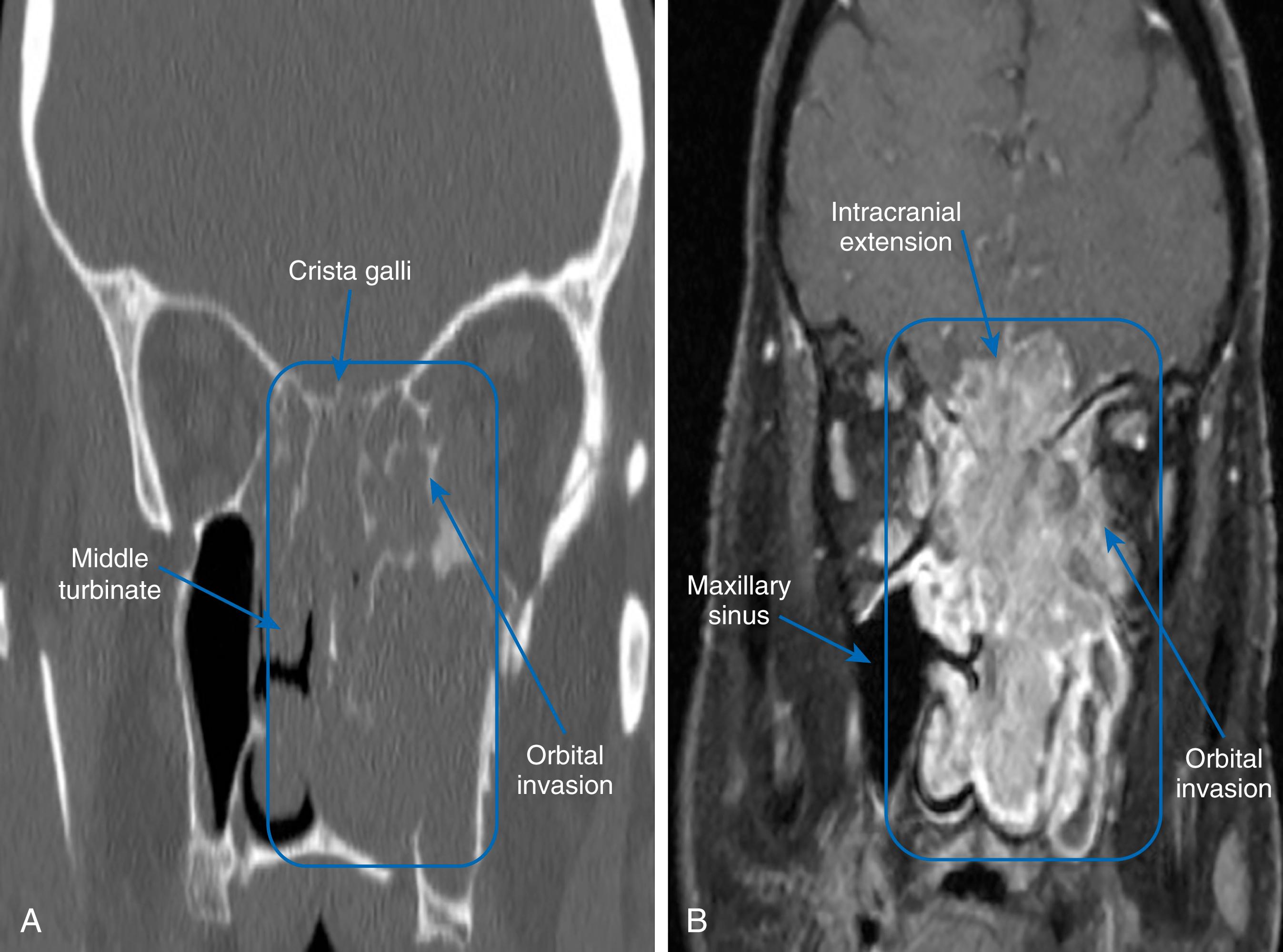
MRI (see Fig. 107.1 ): Delineates affected soft tissue and provides information on perineural spread, characteristic of some malignant neoplasms. This study provides the best information regarding the orbit, skull base, intracranial extension, and anterior facial skin.
Regional and distant staging: Usually completed with either contrasted CTs of the neck and chest or positron emission tomography (PET) CT.
Angiography: Rarely indicated—only needed when there is a presumed vascular malformation or if the tumor has invaded the carotid artery on the primary site imaging
Malignant tumors
Benign tumors that are either symptomatic or growing
Symptom relief
Patient factors: Inability to undergo general anesthesia or have major blood loss
Unresectable tumors (unless palliative surgery indicated)
Diffuse distant metastasis
Lymphomas, plasmacytomas, or other tumors that are highly radiation or chemotherapy sensitive
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here