Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acknowledgment: The authors gratefully acknowledge the contributions of Dr. Ayan Gulgonen and Dr. Kagan Ozer, who authored the chapter on compartment syndrome in the sixth edition of Green’s Operative Hand Surgery.
Acute compartment syndrome (ACS) of the extremity is a diagnosis requiring emergent surgical intervention. ACS is characterized by sustained elevation of tissue pressure within an osseofascial or fascial compartment that exceeds tissue perfusion pressure. This results in local circulatory impairment, ischemia, cellular anoxia, and ultimately tissue death. ACS occurs in the acute phase following injury during which time surgical intervention can reduce the extent of irreversible muscle and tissue injury. Timely diagnosis and treatment are critical to reduce the extent of permanent changes within muscle and nerve tissue. Even with emergent treatment, there may be permanent disability in the affected extremity and a subsequent need for additional surgery, including amputation. , Volkmann’s ischemic contracture represents the late sequelae of compartment syndrome. This disorder has a spectrum of fixed muscle contractures and neurologic impairments. Numerous authors have contributed to our understanding and treatment of this condition. Table 51.1 summarizes some of the historical events in the recognition of this entity including etiology, pathologic findings, and sequelae.
| Author and Year | Development |
|---|---|
| Volkmann, 1881 | First thorough description of this entity with attribution of the cause to muscle ischemia |
| Leser, 1884 | Animal investigations concluded that the pathologic findings were a result of oxygen deprivation |
| Hildebrand, 1890 | First to use the term Volkmann’s contracture; now sometimes referred to as Volkmann-Leser contracture |
| Bardenhauer, 1906 | Release of internal pressure through a forearm fasciotomy to treat an impending Volkmann’s contracture |
| Brooks, 1922, 1925 , Jepson, 1926 | Animal model used to reproduce compartment syndrome through vascular occlusion; muscle necrosis could be prevented by surgical decompression of the muscle compartment |
| Griffiths, 1940 | Emphasized arterial injury and reflex spasm of the collateral vessels as the sole source of muscle ischemia; minimized the role of tight external dressings as the cause of muscle ischemia |
| Seddon, 1956 and 1964 | Described the pattern of muscle infarction common in compartment syndrome (ellipsoid infarct) and treatment with infarct excision; also highlighted the importance of ischemic injury to nerves |
| Mavor, 1956 | First to describe chronic exertional compartment syndrome in the leg (the anterior tibial syndrome) |
| Holden, 1975, 1979 , | Reestablished both intrinsic and extrinsic causes of muscle ischemia; distinguished two patterns of injury leading to muscle ischemia: Type 1: Arterial insult proximal to the site of ischemia Type 2: Elevated intrinsic pressure within the compartment from either internal or external sources |
| Matsen, 1975 | Unified concept of compartment syndrome |
| Whitesides, 1975 | Tissue pressures as a determinant of the need for fasciotomy |
ACS occurs when tissue pressures rise high enough within an osseofascial compartment to cause tissue ischemia. The resultant tissue injury can range from reversible muscle swelling to permanent tissue necrosis depending on the magnitude and duration of tissue pressure elevation. When pathologic tissue pressure elevation has been present for less than 4 hours, ACS is in the early stage ; when pathologic tissue pressure elevation has been present for more than 4 hours, ACS is in the late stage.
Impending compartment syndrome represents a clinical setting in which a compartment syndrome is at risk of developing; however, tissue pressure is not yet sufficiently elevated to cause muscle ischemia. Clinical scenarios in which this may occur include limb reperfusion after prolonged ischemia, posttraumatic swelling of a limb, or high-energy injuries.
Both acute and chronic exercise-induced compartment syndrome have been described (AECS and CECS). Most exercised-induced compartment syndrome is chronic and represents a reversible tissue ischemia due to a noncompliant fascial compartment that is unable to accommodate muscle expansion occurring during exercise. It has been described in both the upper and lower extremities and is different from ACS in that the symptoms are reversible after cessation of exercise. Emergent surgery is not usually indicated unless symptoms do not abate with cessation of the activity as can be seen in AECS. Traditional fasciotomy and endoscopic fasciotomy have been used to treat exercise-induced compartment syndrome.
Crush injury is the external compression of an extremity, as might occur in a building collapse or in an obtunded patient who lays on an extremity for a prolonged period. The compression of the extremity leads to muscle ischemia and reperfusion injury once the compression is relieved. This process of events can lead to compartment syndrome. Crush syndrome is a localized crush injury with systemic manifestations. Reperfusion of the affected extremity can rapidly release muscle breakdown products (rhabdomyolysis) into the system, which can lead to renal failure or death. ,
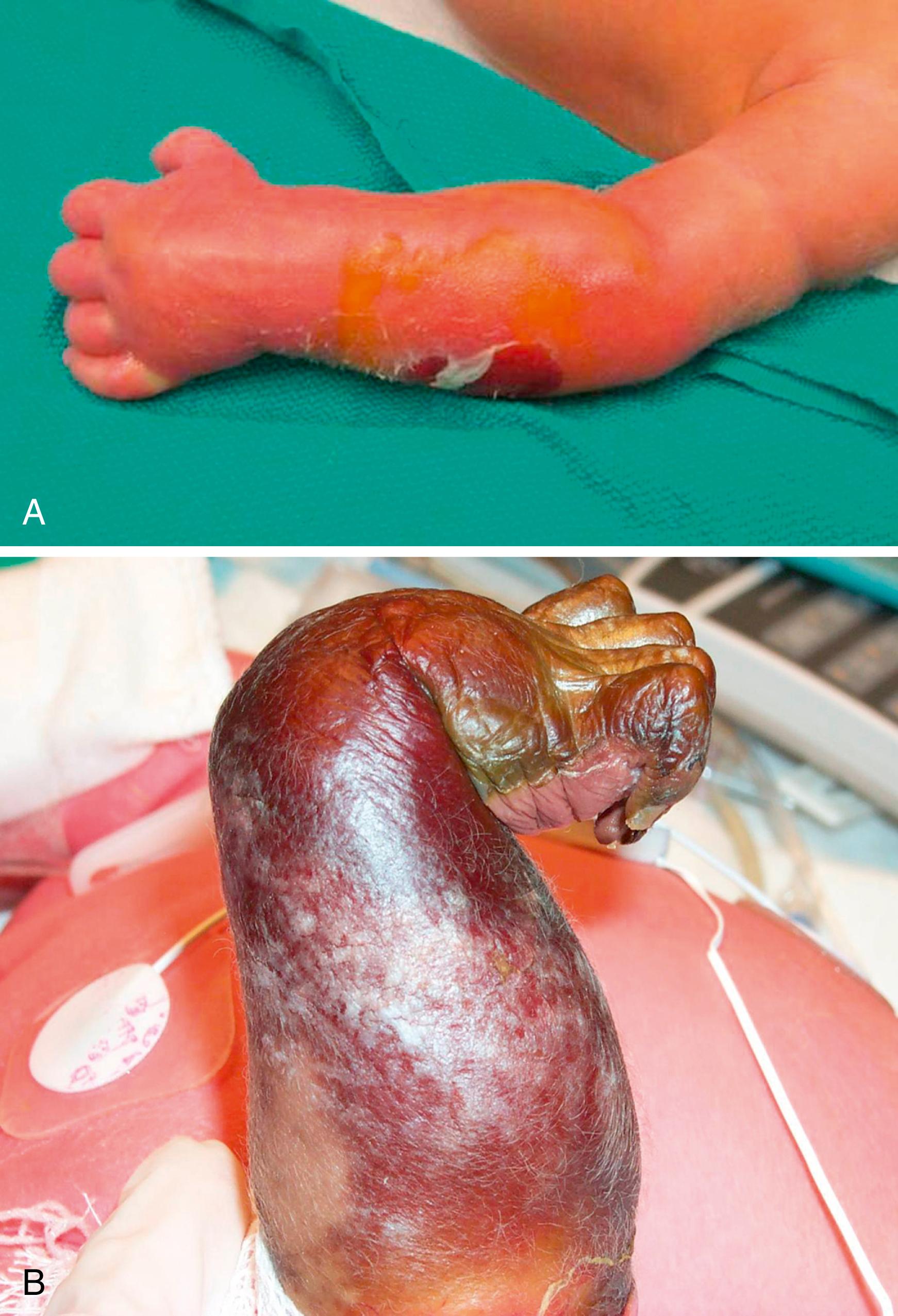
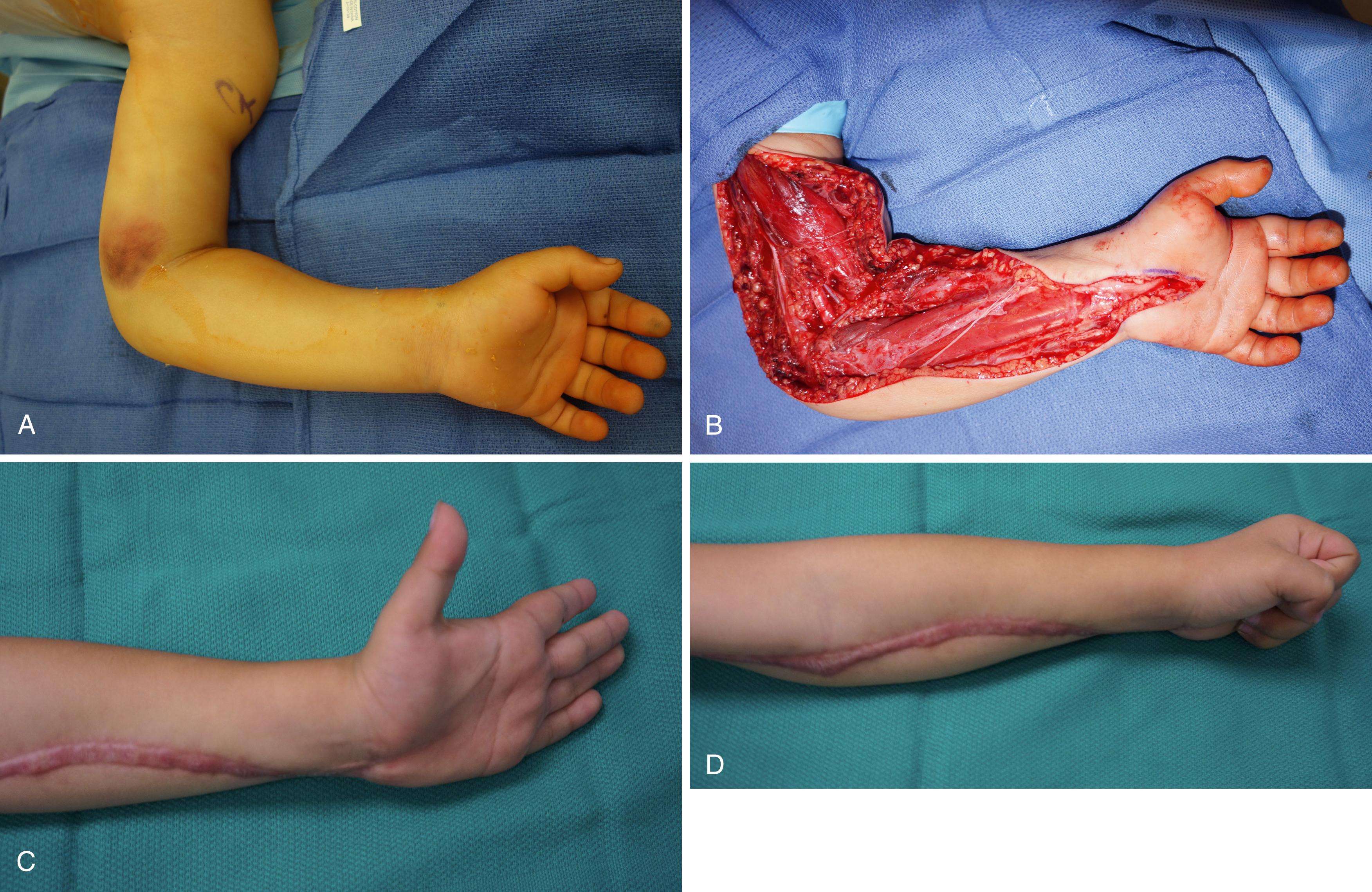
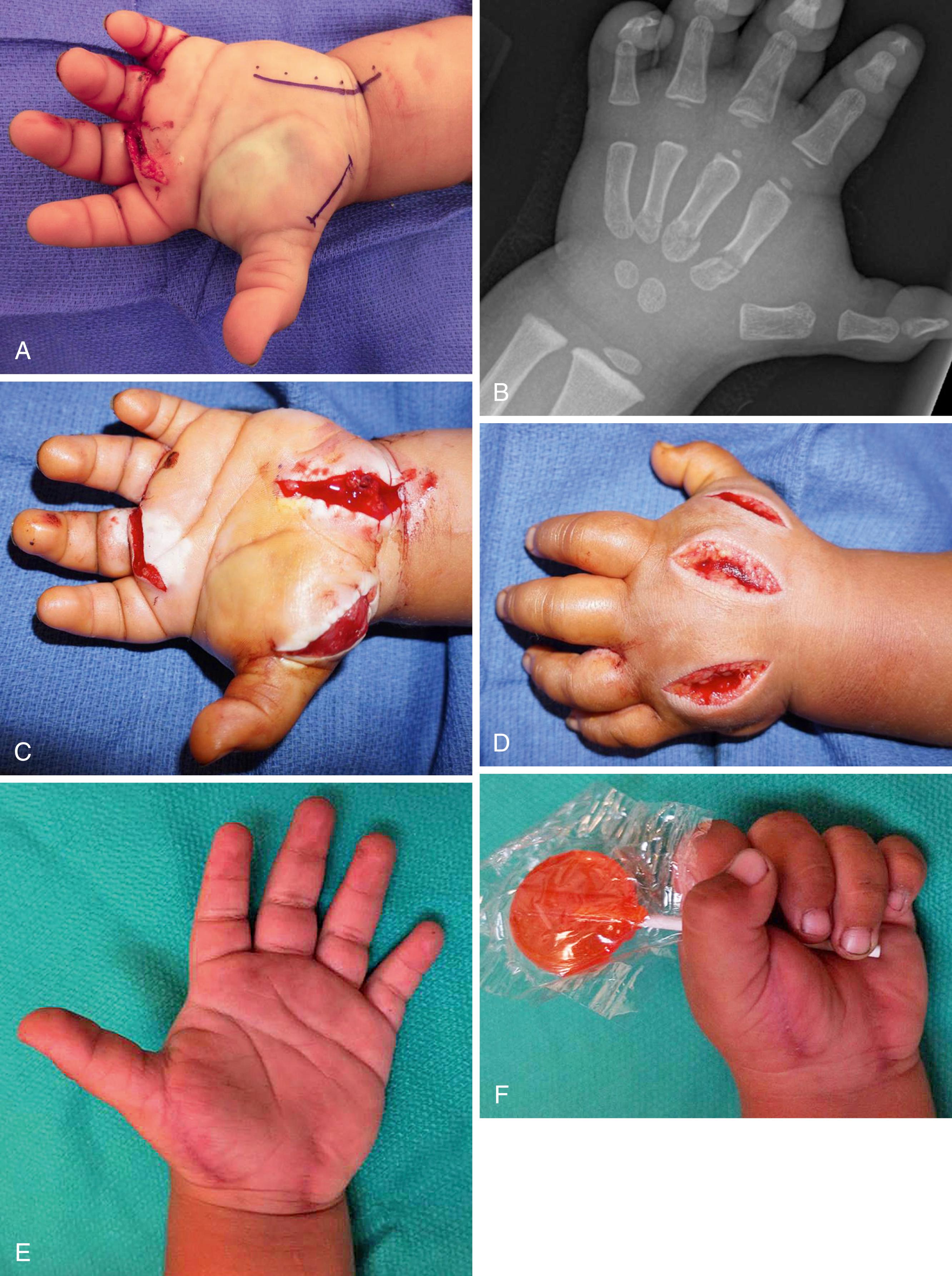
Both neonatal compartment syndrome and neonatal Volkmann’s contracture have been reported. Awareness of this diagnosis is important because early recognition and treatment can improve the functional outcome and growth in neonatal compartment syndrome. The forearm is most commonly affected. In addition to forearm swelling, there is often a characteristic skin lesion on the proximal lateral arm, known as the sentinel lesion of neonatal compartment syndrome. Established neonatal Volkmann’s contracture cannot be improved by early intervention. The infant is frequently misdiagnosed with an arterial injury or amniotic band. A correct diagnosis helps the family cope with the injury and eliminates any underlying questions, concerns, and guilt ( Fig. 51.1 A and B ).
Volkmann’s ischemic contracture is the end result of prolonged ischemia and is associated with irreversible tissue necrosis. The ischemic contracture has a spectrum of presentations.
Pseudo-Volkmann’s contracture has a similar clinical appearance of a Volkmann’s contracture, except the etiology is unrelated to an ischemic event. Active extension of the fingers is limited with the wrist positioned in neutral or dorsiflexion. However, when the wrist is in volar flexion, active extension of the fingers can be performed. The etiology is underlying scarring or tethering of the muscle and/or tendons at the fracture site or surgical implants. Releasing the tethered muscle and/or tenolysis can resolve the problem ( Case Study 51.1 ).
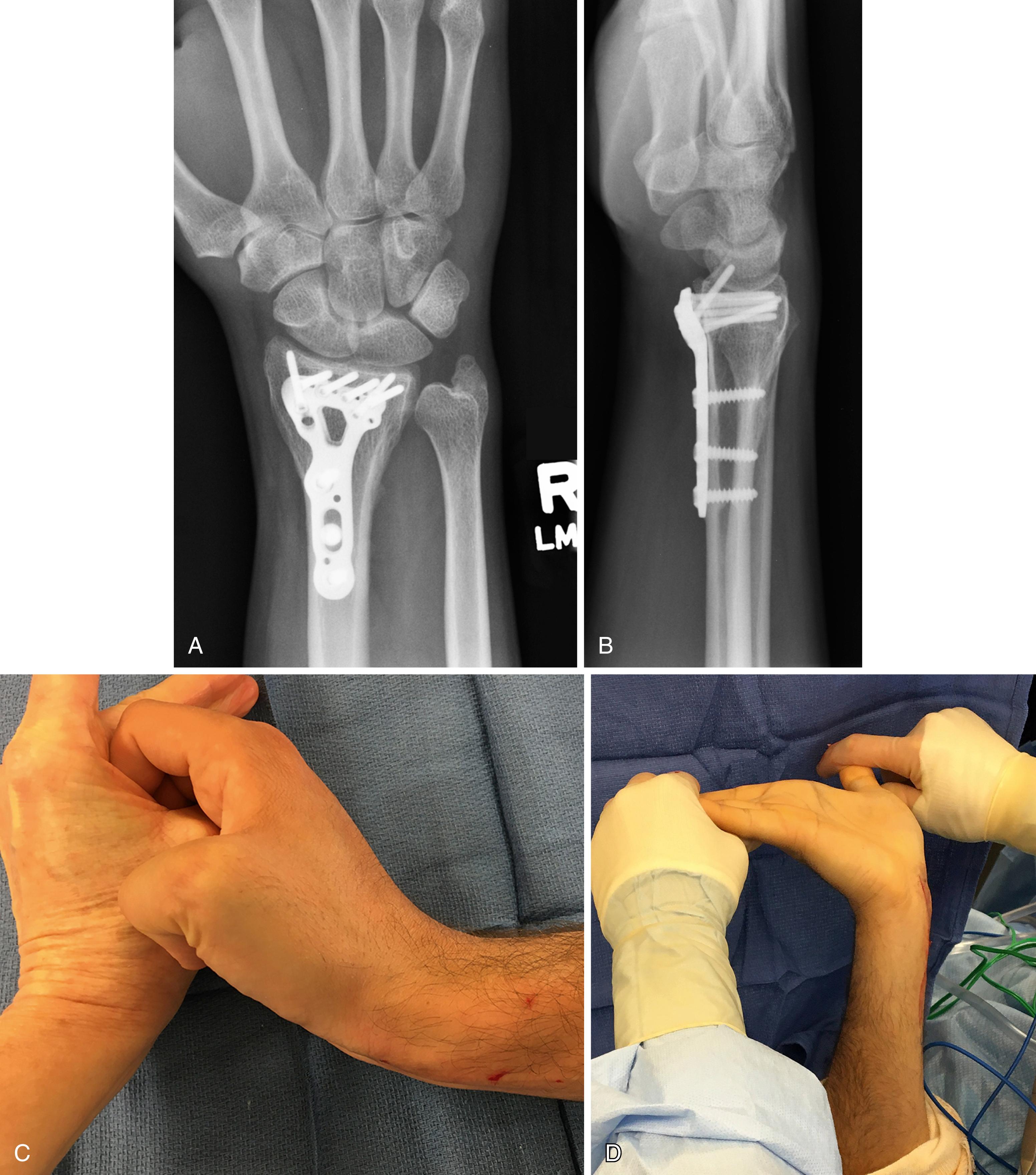
A 32-year-old respiratory therapist presented 3 years after surgical stabilization of the distal radius. He complained of inability to simultaneously extend his wrist and fingers. He would flex his wrist to achieve full finger extension. He did not have any history of atypical pain at the time of his original injury. At surgery, the flexor tendons were densely scarred around the distal edge of the volar plate. Following hardware removal and tenolysis, the patient had combined full passive extension of the wrist, fingers, and thumb ( eFig. 51.1 ).
Compartment syndrome in the upper extremity is most commonly associated with trauma. A variety of conditions and injuries can lead to ACS. These include fractures, penetrating trauma, closed soft tissue injuries, infection, animal and insect bites, extravasation injuries, ischemia-reperfusion injury, external compression by tight dressings or casts, burns, or crush injuries. Compartment syndrome in the absence of fracture should raise concern about an infection, underlying bleeding disorder, or medication-related coagulopathy ( Case Study 51.2 ; Fig. 51.2 ). In these settings, preoperative laboratory analysis and intraoperative cultures are very important. Rhabdomyolysis is considered a sequela of compartment syndrome, but it can also be a precipitant. Medications can cause rhabdomyolysis leading to atraumatic ACS. These include statins, selective serotonin inhibitors, alcohol, and angiotensin receptor agonists.

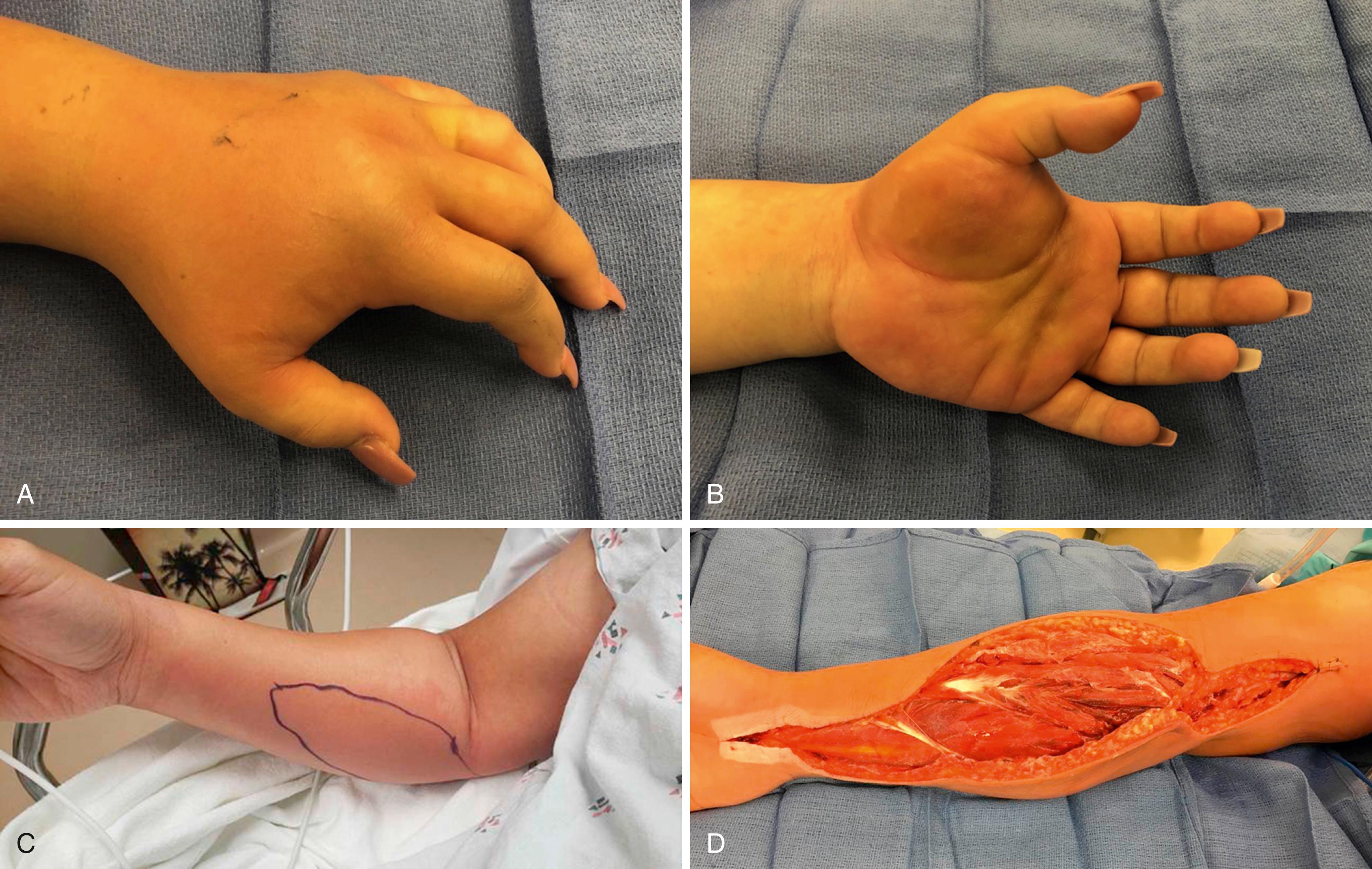
Patient 1 is a 32-year-old woman who presented 1 week postpartum with no history of left-hand trauma. She reported 3 days of pain and swelling in the hand, acutely worse in the 12 hours prior to presentation. She had a clinical picture of a left-hand compartment syndrome with pain, swelling, firm compartments, and pain with passive extension of the fingers ( eFig. 51.2A and B ). She was afebrile, with white blood cell (WBC) count of 7.5K. She had a platelet count of 22, elevated liver function test (LFT), and elevated creatinine. At surgical decompression and fasciotomy, there was no abscess. There was some cloudy fluid in the area of the first dorsal web space and in the thenar space. Gram stain was positive for gram positive. She subsequently grew group A streptococcus (GAS) from her hand and from blood cultures. Her clinical picture was presumed toxic shock syndrome from GAS.
Patient 2 ( eFig. 51.2C and D ) presented with 12 hours of evolving and progressively worsening forearm pain. He had light erythema and clinical signs of compartment syndrome with pain, anxiety, and pain with passive extension of the wrist and fingers. At surgical decompression and fasciotomy, there were microabscesses in the pronator teres and flexor carpi radialis. There was significant bulging of the muscles on release of the compartments. His wound and blood cultures were positive for GAS. His clinical picture was also that of toxic shock syndrome, and his labs normalized as the infection was controlled.
The incidence of upper extremity compartment syndrome is difficult to determine. The estimated incidence in pediatric upper extremity fractures ranges from 0.2% to 1%. , In a large series of trauma patients, the incidence of fasciotomy associated with all upper extremity traumas was 0.41%. In a large database query of the National Trauma Data Bank, specific to forearm fractures, the incidence of associated fasciotomy was 1.2%. Fasciotomy rates associated with traumatic arterial injury ranged from 6.7% to 16%. , In the military Afghanistan war experience, fasciotomy rates of up to 25% were performed based on the injury severity scores, suggesting the prophylactic role of fasciotomy in high-energy injuries. Their incidence of compartment syndrome was 2.8%. ,
Historically, ACS of the upper extremity in the pediatric population was most commonly reported in association with supracondylar humerus fractures in children ( Case Study 51.3 ). Likely, this was related to the historical treatment methods of casting with the elbow in hyperflexion for fracture reduction. Currently, trauma remains the most frequent cause of compartment syndrome in children. Pediatric fracture patterns in the upper extremity most associated with forearm compartment syndrome are both-bone forearm fractures and supracondylar humerus fractures associated with distal radius fractures (i.e., floating elbow injury). , , In adults, the most common upper extremity fractures associated with compartment syndrome are distal radius fractures and both-bone forearm fractures. ,
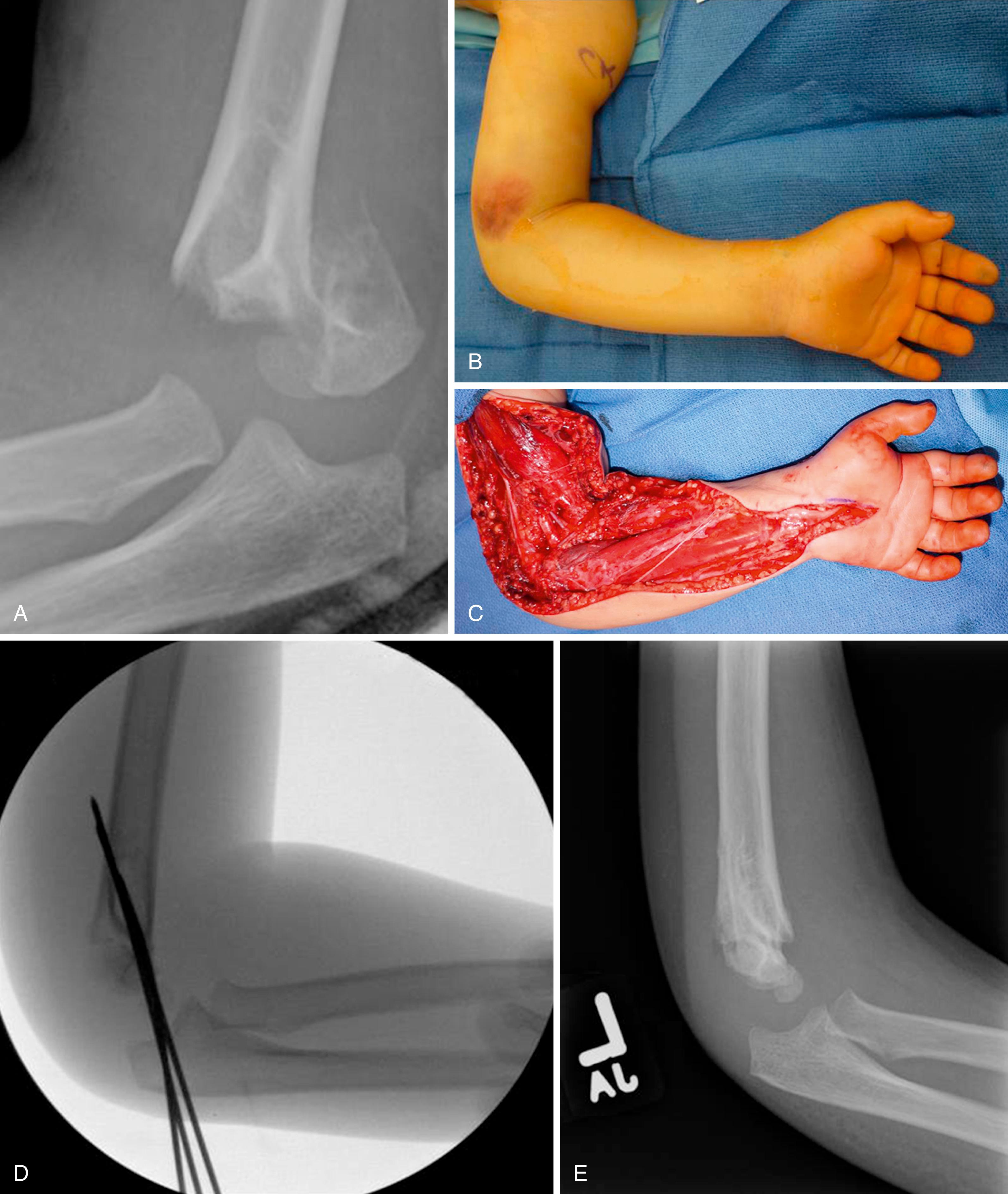
A 9-year-old boy fell from his bicycle and presented to the emergency department with a type 4 Gartland supracondylar humerus fracture. He had severe pain and swelling, with clinical examination consistent with compartment syndrome ( eFig. 51.3A and B ). He was taken emergently for surgical stabilization and fasciotomy ( eFig. 51.3C to E ). Clinical outcome at 5 years is shown in eFig. 51.3F to I .
In adults, compartment syndrome is more prevalent in males younger than 35 years of age, penetrating trauma, open fractures, elbow dislocations, and vascular injuries. , , , , The need for surgical fasciotomy increases dramatically when a vascular injury is present. , Compartment syndrome in the hand is most commonly associated with intravenous injections. Hand compartment syndrome can also occur from infection, following crush injuries, or after a bite or envenomation.
Intravenous infiltration or extravasation injuries are a common source of concern to nurses and physicians, frequently resulting in consultation from the orthopedic or hand service. Most of these infiltrations resolve spontaneously and do not require more than observation and symptomatic treatment. Contrast agents used for radiologic studies have a higher incidence of causing an ACS, particularly higher osmolar ionic contrast agents ( Case Study 51.4 ). Risk factors for IV infiltration include puncture of a vein upstream from the catheter, multiple venipunctures, placement of an IV near a joint flexion crease, vasculopathies, lymphedema, and peripheral vascular disease.
A 38-year-old man undergoing surgery for a ruptured cerebral aneurysm under total IV anesthesia (TIVA) was noted to have lost intraoperative monitoring signals in the right upper extremity. He was noted to have an infiltrated IV at the site of his propofol pump infusion. Clinically his forearm compartment was moderately tight. Based on possible obtundation from rupture cerebral aneurysm in conjunction with intraoperative loss of monitoring signal, we elected to proceed with right forearm fasciotomy ( eFig. 51.4A and B ). Propofol was found throughout his forearm and tracking to the carpal tunnel as well as proximally into the medial arm. On postoperative day 3, he was returned to the operating room for repeat irrigation and debridement and delayed primary wound closure ( eFig. 51.4C ) Clinical outcome at 3 months is shown in eFig. 51.4D .

Although electrical shock injuries are not common, most have involvement of the upper extremity. A high index of suspicion for compartment syndrome or impending compartment syndrome should exist for these patients.
The pathophysiology of ACS is complex. Several theories and models have been developed. The common prerequisite is an external or soft tissue structure (usually fascia) that prevents muscle expansion when the muscle is exposed to increased fluid volume. In all cases, the final common pathway is cellular anoxia. It is the gradient between arterial pressure and tissue pressure that drives tissue perfusion. When tissue pressure, which is normally between 3 to 8 mm Hg, increases, the gradient decreases, and tissue perfusion decreases.
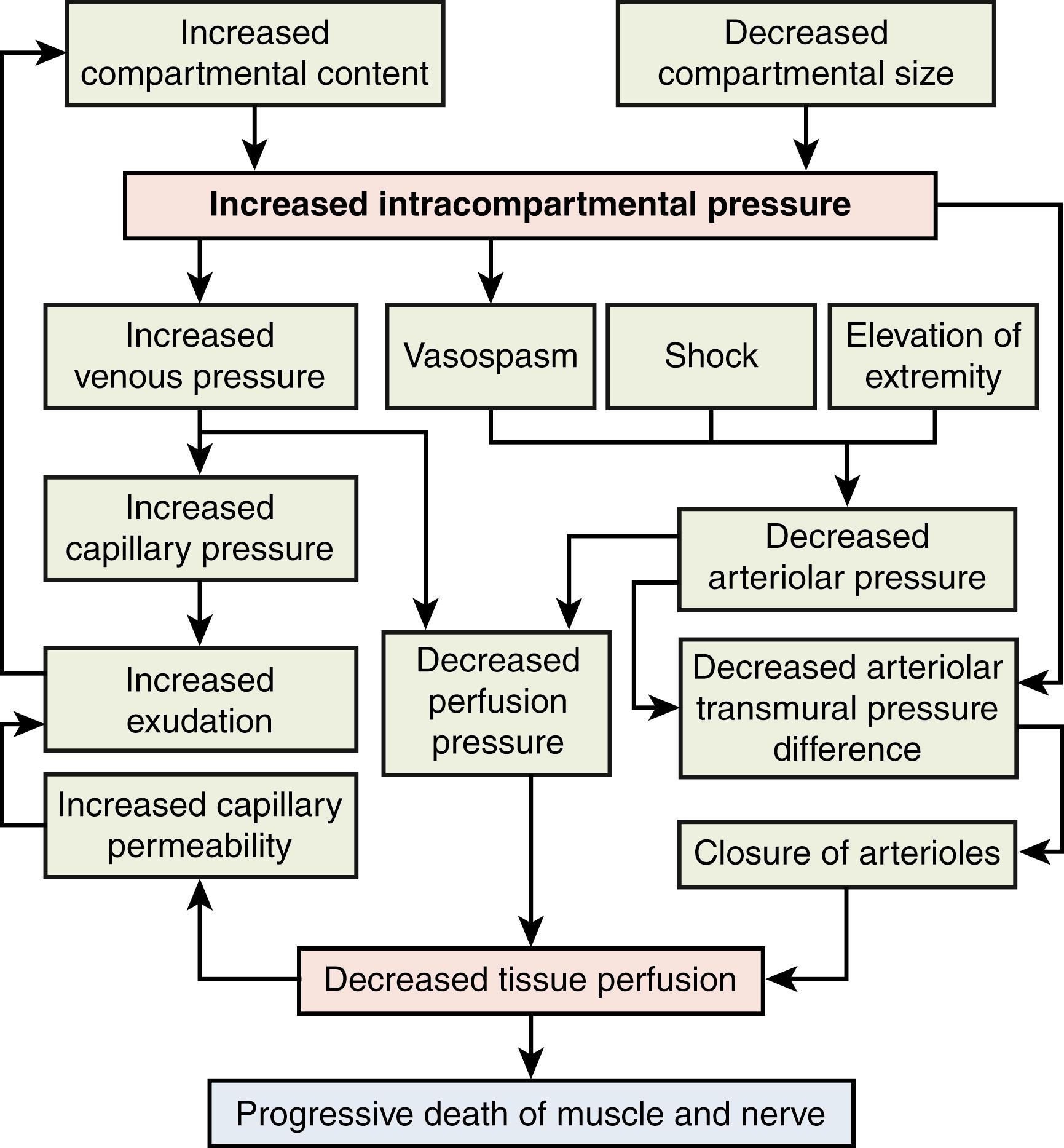
Matsen presented a “unified concept” of compartment syndrome that incorporates several mechanisms of vascular compromise, all leading to cellular injury. Increased compartmental pressure occurring from either internal injury (edema, reperfusion, or bleeding) or external injury (tight cast or dressing, pressure garment) causes a decreased perfusion gradient between arteriole and venous pressures and a resultant decrease in local tissue perfusion. Decreased tissue perfusion results in further tissue insult, increased capillary leakage, and further increase in compartmental pressure. This causes a vicious cycle of increasing cellular ischemia leading to further capillary leakage and swelling and increasing compartment pressures ( Fig. 51.3 ).
Ongoing ischemia eventually leads to cell death and lysis of the myocyte. Degradative enzymes are activated and released into the interstitial tissues, causing further tissue necrosis. The extent of muscle injury depends on the duration of ischemia and the metabolic rate of the tissue. Prolonged ischemia can ultimately lead to liquefactive necrosis of the muscle compartment. Nerve ischemia has similar effects, with prolonged ischemia leading to nerve infarct and irrecoverable nerve function.
The diagnosis of ACS is principally based on clinical examination. Maintenance of a high index of suspicion, particularly in the setting of at-risk injuries and conditions, aids in the prompt recognition and treatment of this condition. In a survey of orthopedic trauma surgeons, most felt that in an awake patient, the diagnosis should be based on the clinical examination. Compartment syndrome can be an evolving diagnosis. The importance of serial clinical examinations with documentation, especially in the high-risk patient or patient with an indeterminate examination, is critical in making an appropriate treatment decision.
Although compartment syndrome is frequently associated with fractures, many other pathologies can lead to ACS as previously discussed. Etiologies are commonly separated into intrinsic causes (typically, bleeding or swelling into a compartment) and extrinsic causes (applied external pressure preventing a compartment from expanding) ( Box 51.1 ). The atraumatic etiologies of compartment syndrome should always be considered, as ACS not associated with fracture frequently has a delayed diagnosis and subsequent worse clinical outcome. , The timing of presentation can vary from within the first few hours of injury to several days following injury. ,
High-energy fracture, usually in young male (open fractures more at risk than closed fractures)
Childhood supracondylar fracture of humerus, especially one associated with distal radius fracture ,
Childhood both-bone forearm fractures (intramedullary nailing of pediatric both-bone and radial head fractures is associated with difficult reduction and prolonged tourniquet times)
Upper extremity fractures associated with vascular injury
Soft tissue or blunt trauma without fracture
Penetrating trauma (usually from bleeding into otherwise closed compartment)
Vascular injury
Iatrogenic procedures, such as venipuncture or arterial blood draw
Reperfusion after prolonged ischemia
Prophylactic fasciotomy should be considered after vascular repair ,
Burns
Edema associated with burn injury
Electrical burns associated with deep muscle damage and edema
Systemic inflammation and fluid resuscitation
Animal and insect bites (e.g., snake bite)
Intravenous fluid extravasation (especially hypertonic fluids such as intravenous contrast material or intraoperative fluid extravasation, particularly in patients where the arm position does not allow easy visualization of the extremity, and when infusion pumps are used)
Infection
Bleeding disorders (coagulation disorders such as hemophilia)
Anticoagulation therapy
Compressive casts or dressings
Burn eschar (circumferential inelastic eschar)
Crush injury
Prolonged laying on the arm, especially in obtunded patient following drug or alcohol overdose or resulting from coma, seizure, or hypoglycemic episode
Building collapse
Intraoperative positioning (prone or lateral positioning with poorly positioned axillary or chest roll causing axillary artery occlusion; also seen in the lower extremity with prolonged lithotomy position)
The hallmarks of diagnosis of ACS have classically been described as the six P ’s of compartment syndrome ( Table 51.2 ): pain, pressure, paresthesias, pallor, paresis, and pulselessness. Some authors have added or substituted poikilothermia of the extremity as one of the P ’s. This use of the term poikilothermia is not completely accurate but indicates that the affected extremity is cooler than body temperature. In most series, pain has been the earliest and most reliable finding, particularly pain disproportionate to the clinical findings. However, pain peaks at 2 to 6 hours of ischemia and then gradually subsides as nerve function becomes increasingly impaired. Patients with a late presentation of or late diagnosis of compartment syndrome have less pain than those with an earlier presentation. Certainly, in cases of impending compartment syndrome, an escalation in pain or pain medication use indicates an emergent need for reevaluation and possible fasciotomy. It is exceedingly important that nursing staff is aware of the need for conveying escalating pain medication requirements to the physician.
| Sign or Symptom | Description |
|---|---|
| Pain | Described as deep, constant, often poorly localized pain that is disproportionate to the physical findings; often poorly responsive to analgesics. Pain is accentuated with passive stretching of the involved compartment. Although this is the most consistent and reliable finding, cases of “silent” compartment syndrome of the lower extremity have been reported and likely also occur in the upper extremity, as suggested by Piñal. , Pain usually peaks at around 2–6 hours of ischemia and then subsides. Patients who present late with acute compartment syndrome may not report as much pain. |
| Pressure | Affected compartment(s) are firm and noncompressible, often described as “rock hard.” |
| Paresthesias | Numbness or “pins-and-needles” sensation in the cutaneous distribution of the nerves that traverse the affected compartment. |
| Pallor | Usually pale, but the extremity may also appear blotchy and often cool (see poikilothermia). |
| Paralysis | Late and unreliable finding. Muscle paralysis may be pain related. When true paralysis is present, this is a poor prognosticator for recovery. |
| Pulseless | Also usually a late finding and poor prognosticator for recovery. |
It has been suggested that in pediatric patients, “it’s the A ’s, not the P ’s” that signal ACS. These A ’s are an increasing requirement for analgesia, the presence of anxiety (or restlessness), and the presence of agitation (or crying). , Children are unable to articulate the feeling of paresthesias, and sensibility testing is unreliable. In children, pain relief requiring minimal analgesia should follow fracture fixation. Persistent or increasing pain is a warning symptom for ACS.
Certain conditions can make the clinical diagnosis of ACS challenging. Altered levels of consciousness as can occur in head trauma, a medically induced coma, or obtundation from other causes can obscure the pain response that is an early symptom of compartment syndrome. Similarly, distracting pain following polytrauma, neurologic injury in the affected limb, and/or regional anesthetic block can mask the signs and symptoms of compartment syndrome. Diagnosis is also more difficult in children and infants who have difficulty cooperating with the examination, may be nonverbal, and are frequently apprehensive and crying. The thicker layer of subcutaneous fat in children may contribute to a false sense of a soft compartment on palpation. In these circumstances, diagnosis or exclusion of compartment syndrome on clinical grounds alone is extremely difficult.
If the clinician is uncertain of the diagnosis based on equivocal physical findings, compartment pressure can be measured ( Table 51.3 ). Several different methods can be used. Continuous pressure measurements can be obtained with a wick catheter or connection to a continuous pressure monitor. , Newer devices with intracompartmental placement of a micro sensor can provide real-time information to physicians through a cloud-based application, allowing ongoing assessment of compartment pressures. Single recording digital devices are the most commonly used tool to assess the compartment pressure. These devices are sensitive to patient motion and should not supplant repeat clinical examinations. The risks of iatrogenic injury to nerves or vessels should be considered when deciding to take a pressure measurement. Ultrasound-guided placement may help mitigate the risk. Although controversial, the thresholds/indications for fasciotomy are an absolute pressure greater than 30 to 40 mm Hg or pressures within 20 to 30 mm Hg of either the diastolic blood pressure or the mean arterial pressure. , In children, obtaining a compartment pressure measurement can be difficult, and may be better done in the operating room under sedation with plans to proceed to fasciotomy if necessary.
| Aspect of Measurement | Considerations |
|---|---|
| Patient position | Supine Measured extremity should be at heart level Measurements in uncooperative patients and children should be made with the patient sedated or in the operating room with the patient sedated |
| Needle | 18-g straight, side-port, slit catheter, or wick |
| Transducer | Handheld digital (Stryker pressure transducer) Arterial line monitor |
| Needle placement | Perpendicular to muscle belly Several readings at multiple depths Near fracture site Near area of maximum tension |
| Threshold pressure | 30–40 mm Hg Within 30 mm Hg of diastolic blood pressure or mean arterial pressure |
| Contraindications to measuring compartmental pressure | Underlying neurovascular structures at risk Coagulopathy Diffuse cellulitis |
Pulse oximetry of the affected extremity has not been found to be useful. , Near-infrared spectroscopy (NIRS) has been evaluated in the early diagnosis and monitoring of an impending compartment syndrome, but it has not been widely adopted. The reliability and efficacy of NIRS has yet to be proven. Creatine kinase (CK) may be a useful laboratory indicator of compartment syndrome. Levels higher than 300 U/L are strongly suggestive of compartment syndrome in the forearm.
In questionable clinical situations, unless otherwise contraindicated, the safer intervention is to perform a fasciotomy. Bulging of the muscle compartment and clinical softening of the extremity at the time of fasciotomy confirms the diagnosis. If muscle bulging does not occur, the surgical incision can be closed with minimal morbidity.
Chronic exertional compartment syndrome of the upper extremity has been described in the flexor compartment of the forearm and isolated to various muscles including the anconeus, pronator quadratus, extensor carpi ulnaris, and adductor pollicis. , Patients with chronic exertional compartment syndrome typically complain of pain that starts as a dull ache within the first 30 minutes after starting an activity. Burning, cramping, or aching pain progresses as the activity is continued. The pain escalates to a level of discomfort where the patient can no longer continue the activity or where the pain adversely affects the patient’s performance. Recreational activities associated with exertional compartment syndrome of the upper extremity include sports such as rowing, bicycle riding, or motorcycle riding. Vocational activities involve manual labor jobs that require prolonged or repetitive grip and/or pinch. The pain and tissue firmness resolve spontaneously with cessation of the activities. Diagnostic studies have principally involved measurement of compartment pressures before, during, and after exercise. , , Magnetic resonance imaging has been used before and after exercise as a diagnostic tool. A signal change in T2 imaging in an isolated fascial compartment associated with activity supports the diagnosis of exercise-induced compartment syndrome. ,
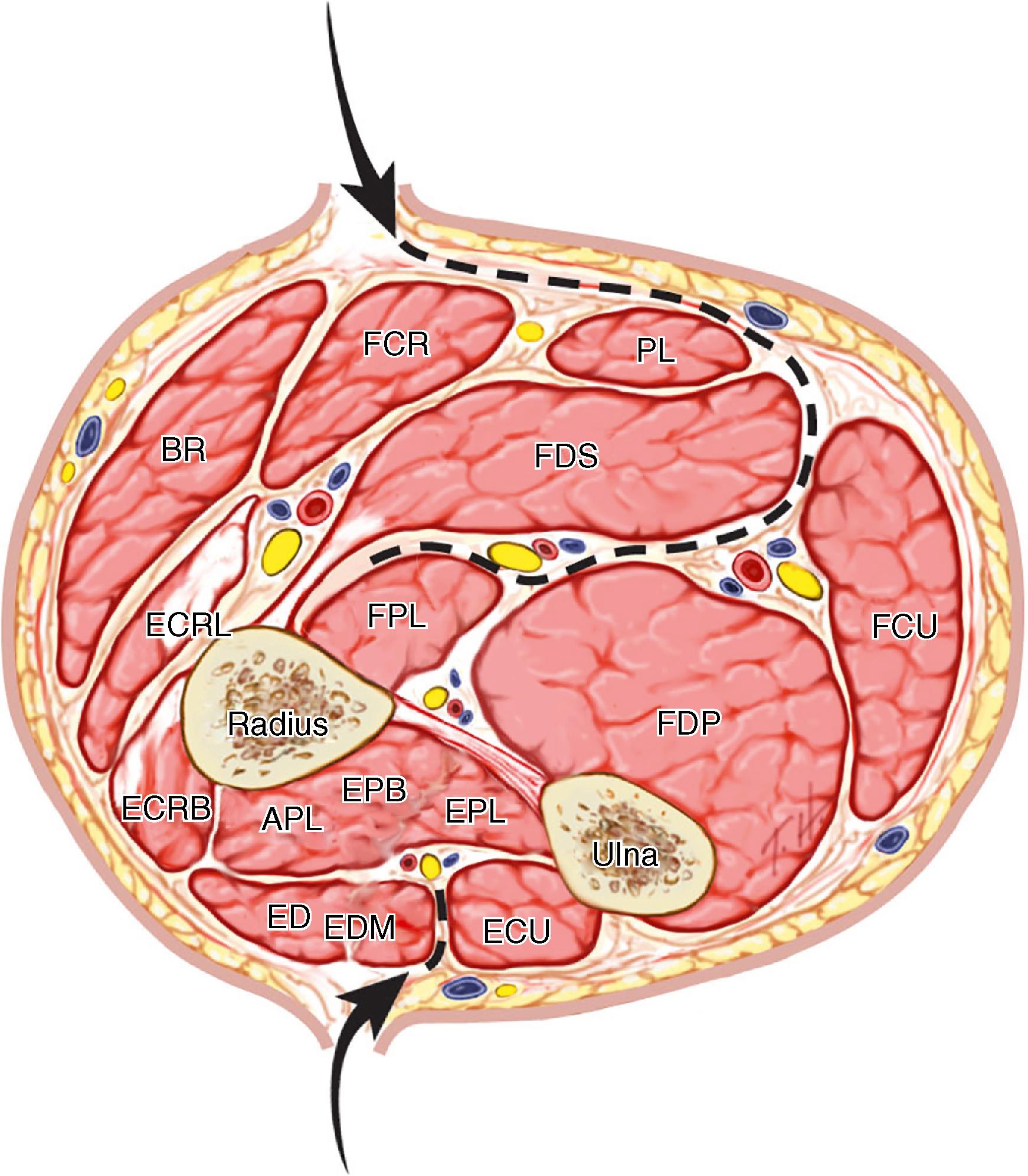
The compartments of the upper extremity are listed in Table 51.4 . Any of these anatomic spaces can be affected by tissue pressure elevation. Elevated tissue pressures are most commonly seen in osseofascial spaces. However, other tissue structures (e.g., fascia) provide a rigid barrier and are unable to expand sufficiently and accommodate swelling. In the upper extremity, the fascial components and the skin can act as barriers that require decompression at the time of surgery. In addition, portions of each compartment can be differentially affected. Some muscles involve more than one compartment, and isolated muscles or musculotendinous areas can be involved as a separate compartment that requires separate release or fasciotomy.
| Compartments | Contents | ||
|---|---|---|---|
| Arm | Anterior | Biceps and brachialis muscles, brachial artery, and median nerve | |
| Posterior | Triceps muscle and ulnar and radial nerves | ||
| Deltoid | Not technically a separate compartment but has a thick epimysium that may require decompression | Anterior, middle, and posterior heads may require separate release of each area of epimysium | |
| Forearm | Volar | Superficial | Flexor carpi radialis, palmaris longus, pronator teres, flexor carpi ulnaris, and flexor digitorum superficialis muscles |
| Deep | Flexor digitorum profundus, flexor pollicis longus, pronator quadratus muscles, a and anterior interosseous nerve and artery | ||
| Dorsal | Mobile wad | Brachioradialis, extensor carpi radialis longus, and extensor carpi radialis brevis muscles | |
| Extensor | Extensor digitorum communis, extensor carpi ulnaris, extensor pollicis longus, abductor pollicis longus, extensor pollicis brevis, and supinator muscles, b and posterior interosseous nerve | ||
| Anconeus a | Anconeus | ||
| Hand | Thenar | Abductor pollicis brevis, opponens pollicis, and flexor pollicis brevis muscles | |
| Hypothenar | Abductor digiti minimi, flexor digiti minimi, and opponens digiti minimi muscles | ||
| Adductor pollicis | Adductor pollicis muscle (two heads) | ||
| Dorsal interossei (4) | Each is a separate compartment | ||
| Volar interossei (3) | Each is a separate compartment | ||
| Fingers c | |||
a Reported isolated involvement in exertional compartment syndrome.
b The supinator muscle is not typically a component of the extensor compartment, but decompression can be done through the brachioradialis/extensor carpi radialis longus interval.
c Compression of the neurovascular structures by the rigid Cleland and Grayson ligaments can lead to skin necrosis and/or loss of the finger.
The goal of treatment is to prevent tissue necrosis, avert neurovascular compromise, and avoid permanent functional deficits. These complications can be minimized or avoided with early recognition and prompt intervention.
The first step in treatment is to remove all possible extrinsic causes of pressure, including circumferential dressings, cast padding, and casts. Casts have been shown to restrict compartment expansion by 40%. Release and spreading of the cast reduces pressure elevation by 40% to 60% depending on the presence of dry or wet blood on the cast padding. Cast padding filled with blood is a rigid structure and referred to as a “blood cast.” This cast padding must be split. The limb should be elevated only to heart level. Although limb elevation may decrease swelling, it can also reduce perfusion to the affected limb and exacerbate tissue ischemia.
In cases of atraumatic ACS, a more detailed history is necessary. The history should include a list of medications, recent activities, exposure to sick individuals, any bleeding diathesis, and any periods of intoxication or obtundation with prolonged pressure on the extremity.
Laboratory evaluation may be indicated in ACS. CK is a predictor and prognosticator in ACS. CK levels more than 300 U/L are strongly suggestive of ACS following forearm injury. Levels higher than 10,000 U/L after forearm injury are associated with a poor outcome. Baseline complete blood count (CBC) and renal laboratory values (blood urea nitrogen [BUN] and creatinine) should be obtained. In cases of atraumatic ACS, laboratory evaluation should include tests for coagulopathy (prothrombin time [PT], partial thromboplastin time [PTT], CBC, liver function tests), infection (white blood cell [WBC] count, erythrocyte sedimentation rate [ESR], C-reactive protein [CRP], lactic acid), indicators of muscle injury (CK), and baseline renal function (BUN and creatinine). Urinalysis for myoglobin, serum electrolytes, creatinine, and myoglobin should be obtained in the setting of prolonged ischemia, crush injury, or ischemia-reperfusion injury. If there is a suspicion of a bleeding disorder, a hematologist should be consulted.
Medical management of shock, hypoxia, metabolic acidosis, and electrolyte imbalance should be addressed immediately. Supportive care with vigorous hydration, correction of metabolic function, and treatment of hyperkalemia is necessary to prevent sequelae such as renal failure, shock, hypothermia, cardiac arrhythmias, or cardiac failure. Supportive care should be initiated in the emergency room but should not delay surgical treatment.
Hypertonic mannitol has been used to lower intracranial pressure. The use of mannitol in decreasing extremity swelling has been described in animal models and limited case studies. Mannitol administration has not gained widespread use for treatment of impending or ACS. Nonetheless, it has been hypothesized that the use of mannitol may have played a role in the decreased incidence of compartment syndrome in trauma patients at a single medical center over a 10-year time period. Hypertonic mannitol has been found to decrease endothelial swelling and may help reduce muscle necrosis in its function as an oxygen-free radical scavenger. In one clinical report, patients were given a 100-mL bolus of 20% mannitol, followed by an infusion of 10 g/hour for 6 to 24 hours.
Emergent surgical decompression (fasciotomy, or release of the fascia overlying the affected compartments) performed quickly and safely is the treatment for ACS. Neonatal compartment syndrome must be treated with similar urgency ( Fig. 51.4 ). Early fasciotomy is associated with a lower rate of permanent functional impairment. Release of the epimysium surrounding the muscle may also be necessary. Necrotic tissue should be excised. Dead tissue is a nidus for secondary infection or it leads to subsequent fibrosis and contracture. Questionable tissue should be left in situ and reevaluated in a few days to avoid inadvertent removal of viable tissue. Late fibrosis of necrotic muscle can lead to compression of the adjacent nerves, which further impairs extremity function. Concomitant procedures may be necessary at the time of fasciotomy including fracture reduction and stabilization, vascular repair, and nerve exploration. Nerve repair or grafting is best performed at the time of definitive wound closure.

Late or delayed diagnosis increases the risk for severe complications, including infection, neurologic injury, need for amputation, and death. Previously, concerns about an increased risk of infection led to the recommendation not to perform fasciotomy after 24 hours had elapsed since the onset of symptoms. The morbidity and mortality in the lower extremity with late fasciotomy is particularly high. In the upper extremity, we do not feel that the risk of late fasciotomy outweighs potential benefits to the extremity. We no longer consider this an absolute contraindication for surgery. Currently, there are more options for wound management and antibiotic therapy. Removal of necrotic muscle can decrease the severity of subsequent muscle fibrosis and joint contracture. Debridement of nonviable muscle improves the environment for the neurovascular structures and may allow early functional reconstruction of the lost muscle(s) by means of tendon transfers or free functional muscle transfers (FFMTs).
In addition, the length of time that elevated pressure sufficient to cause tissue necrosis has been present is often unclear, and some muscle preservation may be facilitated with late fasciotomy. In some cases, good results in children have been reported following fasciotomy as late as 72 hours after the injury (within the acute swelling phase). Dramatic, essentially full recovery has been reported following compartment syndrome of the lower leg in children after delayed presentation.
The indications for surgical fasciotomy are ACS and exercise-induced compartment that is recalcitrant to nonoperative measures. Our preference is to manage questionable cases of impending compartment syndrome with surgical decompression, providing the patient is medically stable for the procedure. Prophylactic fasciotomies should be performed following vascular repair/reconstruction where ischemia time exceeds 3 hours. Shorter periods of ischemia do not eliminate the risk of developing compartment syndrome, however, and careful postoperative monitoring is necessary.
Contraindications to fasciotomy are few. Coagulopathy should be corrected prior to surgical intervention. Unstable intubated patients should be considered candidates for bedside fasciotomy using local anesthesia and sedation. This should be performed by the most senior surgeon on the team.
The surgical incision for the upper extremity is extensile from the brachium to the carpal tunnel. The extent of the release performed is tailored to the clinical and intraoperative findings. Release of the dorsal forearm and compartments of the hand requires separate incisions when indicated. A separate midaxial skin incision for each finger may also be necessary to prevent skin necrosis and loss of the fingers as the swelling can compromise the neurovascular bundle.
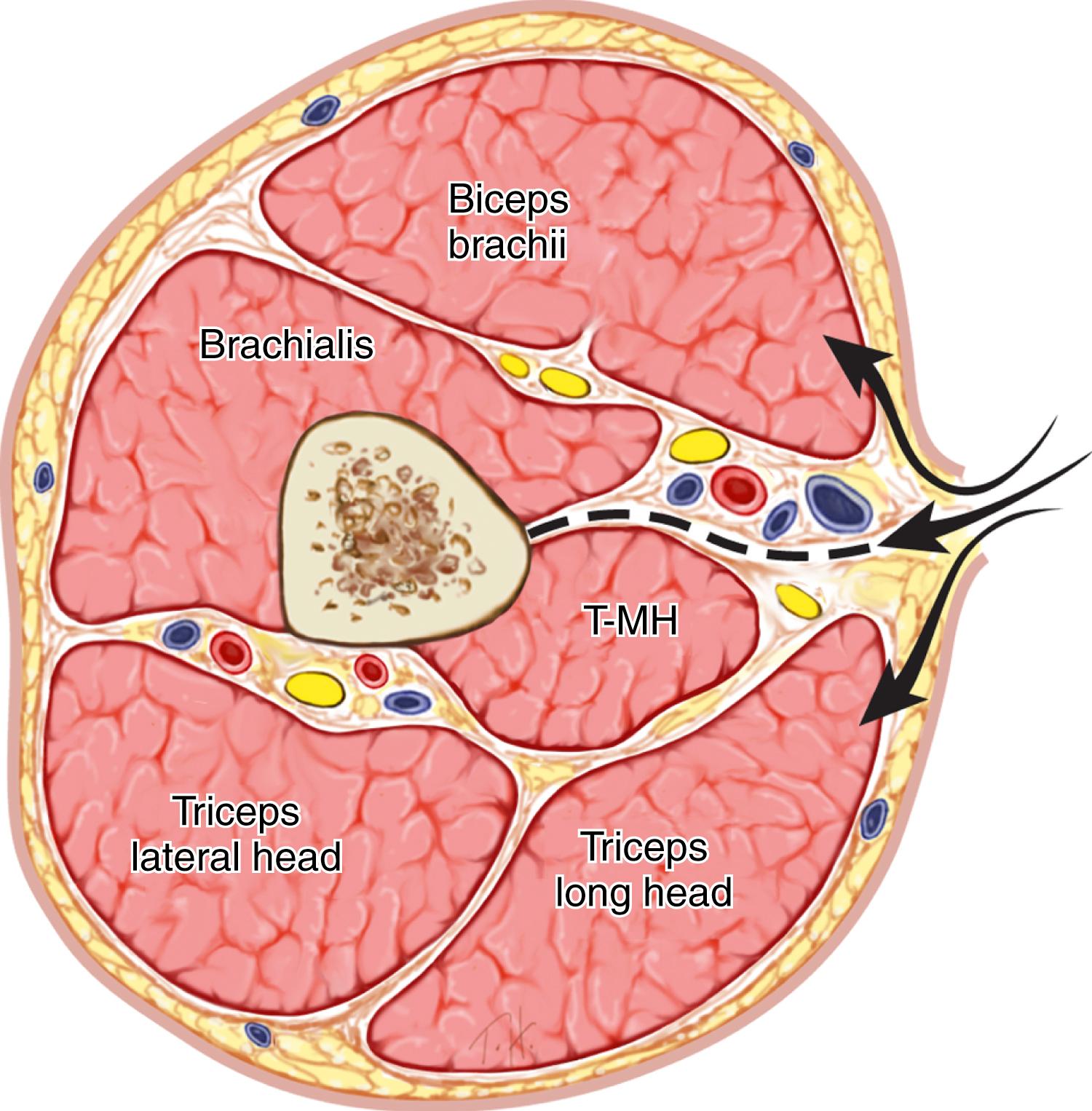
The anterior and posterior compartments of the arm can be decompressed through a single medial incision. This allows access to the neurovascular structures of the arm, the medial fascia of the biceps and brachialis in the anterior compartment, and the fascia of the triceps. Excision of the medial intermuscular septum will provide additional decompression of both compartments ( Fig. 51.5 ). The incision can be easily extended to the elbow crease and incorporated with the incision for decompression of the forearm. This also allows release of the lacertus fibrosus and access to the brachial artery. When there is no anticipated need to evaluate the brachial artery or to decompress the forearm compartments, fasciotomies can be performed through separate anterior and posterior midline incisions to decompress the flexor and extensor compartments, respectively, or through a single lateral incision.
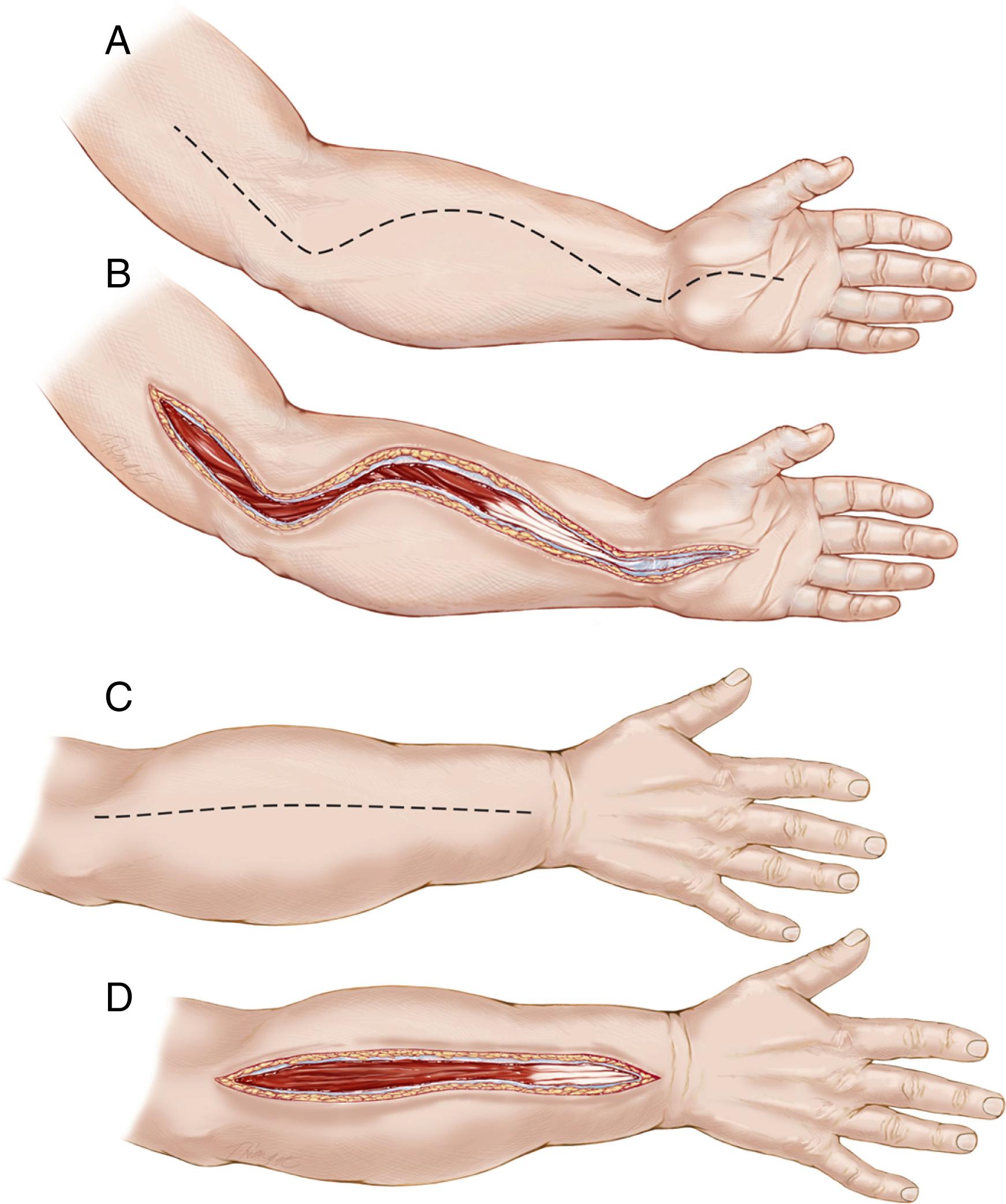
Several skin incisions have been described for the forearm. The surgical incisions are long and extensile ( Fig. 51.6 ). Because the incisions are left open, we prefer an incision that minimizes exposure of neurovascular structures and can be extended in a proximal direction into the medial arm and in a distal direction into the carpal tunnel (see Fig. 51.6 A and B). Once the skin is incised, the antebrachial fascia is opened in a longitudinal direction from the lacertus fibrosus to the wrist flexion crease ( Fig. 51.7 ). This decompresses the superficial flexor compartment. The deep flexor compartment is most easily and safely exposed through the ulnar side of the forearm. We begin at the mid to distal forearm and identify the interval between the flexor carpi ulnaris and flexor digitorum superficialis. The flexor digitorum profundus and flexor pollicis longus fasciae are exposed and released through this interval ( Fig. 51.8 ). This is a crucial component of the surgery as the deep flexor compartment is typically the most affected by the increased compartmental pressure. The susceptibility of the deep flexor compartment may be related to its single vessel angiosome. Through this same interval but deep to the flexor digitorum profundus, the fascia overlying the pronator quadratus is also released. During the dissection, if the muscles appear pale after release of the fascia, additional release of the epimysium should be performed. For these muscles, if the epimysium is not released, reperfusion injury will lead to additional swelling within the muscle and further muscle damage.
Following release of the volar compartment, clinical evaluation of the remaining tension and pressure in the dorsal forearm compartment and/or hand is performed to determine whether additional release of these compartments are necessary.
The extensor compartments are released through a midline longitudinal dorsal incision extending from the lateral epicondyle to the distal radioulnar joint. This will allow release of the mobile wad and the extensor compartment (see Fig. 51.6 C and D).
An alternative incision to release the forearm flexor compartments is the ulnar incision, which is the same incision used for the flexor pronator slide ( Fig. 51.9 ). One advantage of this incision is that it does not leave neurovascular structures exposed and is extensile into the proximal medial arm. Both the superficial and deep compartment fascia can be released. A separate incision for median nerve decompression through the carpal tunnel is required. Elevation of the dorsal soft tissue flap allows access to the fascia overlying the extensor compartment. This approach limits access for fracture or tissue repair or tissue debridement.

The hand has 10 separate compartments. Intraoperative assessment and/or measurement of compartment pressures can be used to determine the number of compartments that require release; however, when in doubt release the compartment ( Figs. 51.10 and 51.11 ).
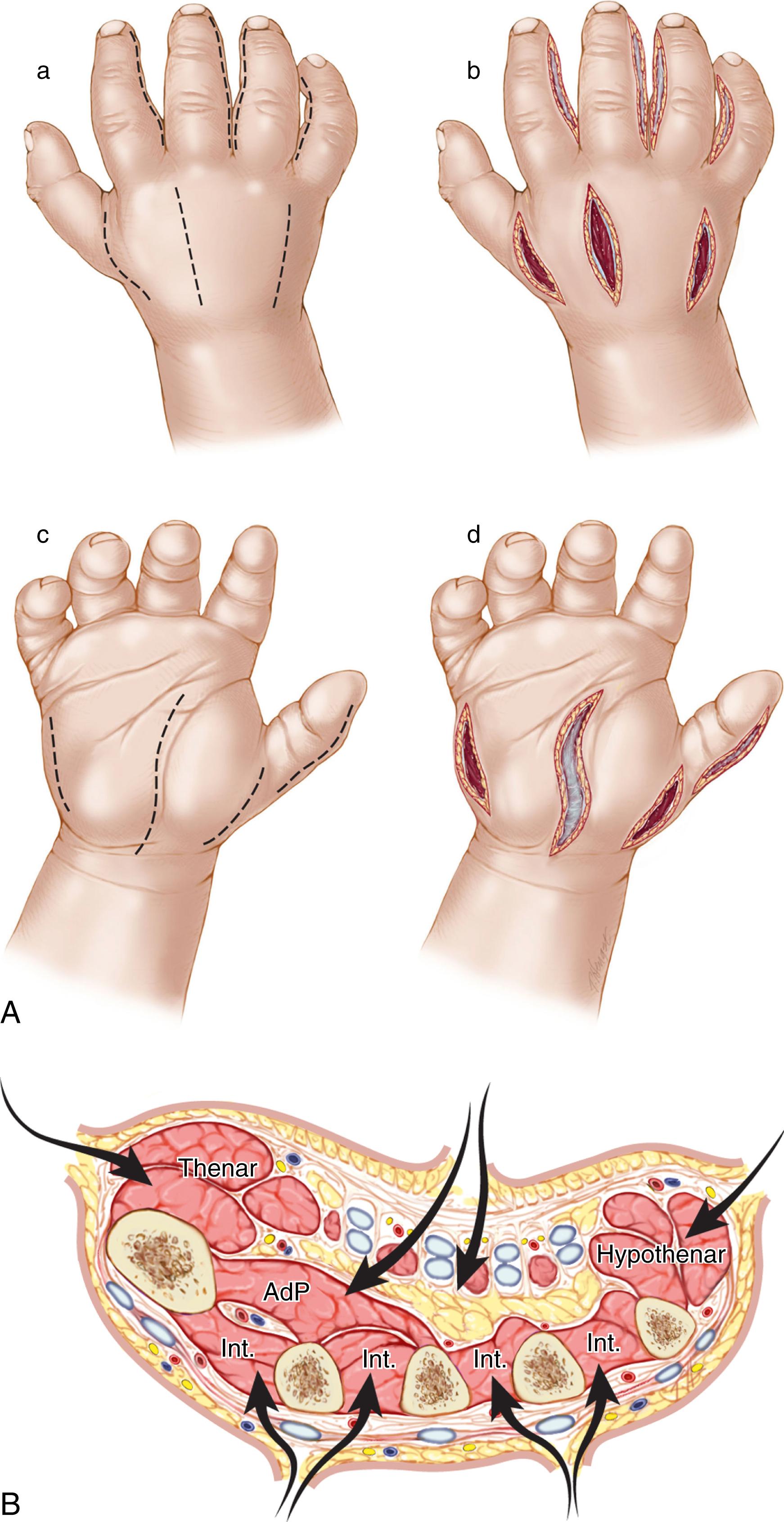
Decompression should start with an extended carpal tunnel release. Carpal tunnel release will usually adequately release the Guyon canal without division of the volar carpal ligament (roof of the Guyon canal). However, in cases where the patient has specific ulnar nerve symptoms or following a severe crush injury, formal release of the Guyon canal and the ulnar antebrachial fascia may be beneficial. The carpal tunnel incision can be extended to the second volar web space. In the distal portion of the incision, the volar fascia of the adductor pollicis muscle can be released. The fascia extending from the long finger metacarpal to the palmar fascia (separating the deep radial and ulnar midpalmar spaces) can be released; this will help decompress the volar interosseous muscles. The thenar and hypothenar muscles are decompressed through separate incisions as needed.
The dorsal interosseous muscles are decompressed through dorsal incisions between the second and third metacarpals and fourth and fifth metacarpals. The volar interossei can be reached by subperiosteal dissection along the radial and ulnar borders of the metacarpals. The first dorsal interosseous muscle is decompressed through an incision placed in the first dorsal web space or from the thenar incision. The dorsal fascia of the adductor pollicis muscle can also be released through this incision (see Fig. 51.10 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here