Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
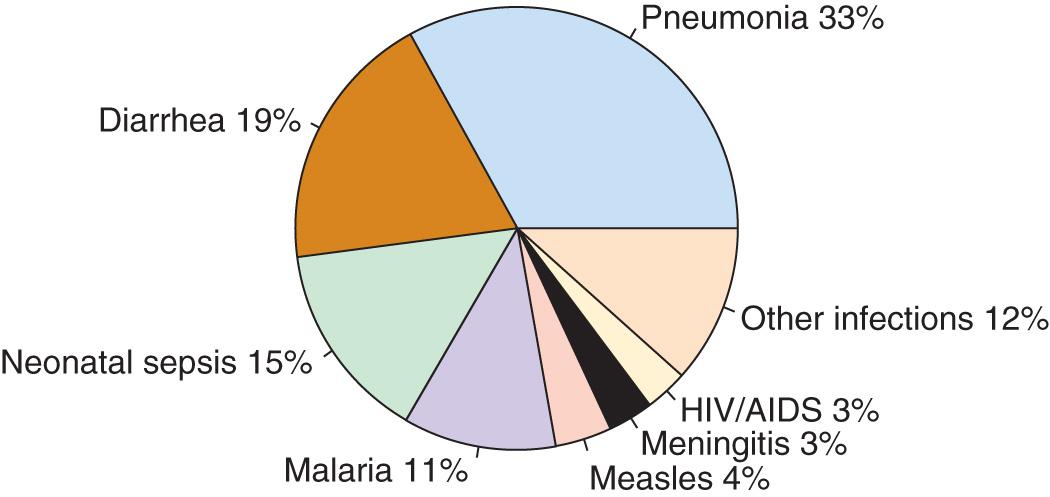
Pneumonia, defined as inflammation of the lung parenchyma, is the leading infectious cause of death globally among children younger than 5 yr, accounting for an estimated 920,000 deaths each year ( Fig. 428.1 ). Pneumonia mortality is closely linked to poverty. More than 99% of pneumonia deaths are in low- and middle-income countries, with the highest pneumonia mortality rate occurring in poorly developed countries in Africa and South Asia ( Table 428.1 ).
| UNICEF REGIONS | PNEUMONIA CASES IN CHILDREN YOUNGER THAN 5 YR OF AGE | PNEUMONIA MORTALITY RATE (UNDER-5 DEATHS PER 1,000 LIVE BIRTHS) |
|---|---|---|
| West and Central Africa | 298,000 | 16.2 |
| Sub-Saharan Africa | 490,000 | 13.7 |
| Eastern and Southern Africa | 177,000 | 10.9 |
| South Asia | 282,000 | 7.9 |
| Middle East and North Africa | 46,000 | 4.1 |
| East Asia and the Pacific | 81,000 | 2.7 |
| Latin America and the Caribbean | 23,000 | 2.1 |
| Least Developed Countries | 363,000 | 12.0 |
| World | 920,000 | 6.6 |
In the United States, mortality from pneumonia in children declined by 97% between 1939 and 1996. This decline likely resulted from the development of antibiotics and vaccines and the expansion of medical insurance coverage for children. Effective vaccines against measles (see Chapter 273 ) and pertussis (see Chapter 224 ) contributed to the decline in pneumonia-related mortality during the 20th century. Haemophilus influenzae type b (see Chapter 221 ) was also an important cause of bacterial pneumonia in young children but became uncommon following licensure of a conjugate vaccine in 1987. The introduction of pneumococcal conjugate vaccines (PCVs) (see Chapter 209 ) has been an important contributor to the further reductions in pneumonia-related mortality achieved over the past 15 yr.
Although most cases of pneumonia are caused by microorganisms, noninfectious causes include aspiration (of food or gastric acid, foreign bodies, hydrocarbons, and lipoid substances), hypersensitivity reactions, and drug- or radiation-induced pneumonitis (see Chapter 427 ). The cause of pneumonia in an individual patient is often difficult to determine because direct sampling of lung tissue is invasive and rarely performed. Bacterial cultures of sputum or upper respiratory tract samples from children typically do not accurately reflect the cause of lower respiratory tract infection. Streptococcus pneumoniae (pneumococcus) is the most common bacterial pathogen in children 3 wk to 4 yr of age, whereas Mycoplasma pneumoniae and Chlamydophila pneumoniae are the most frequent bacterial pathogens in children age 5 yr and older . In addition to pneumococcus, other bacterial causes of pneumonia in previously healthy children in the United States include group A streptococcus ( Streptococcus pyogenes ; see Chapter 210 ) and Staphylococcus aureus (see Chapter 208.1 ) ( Tables 428.2, 428.3, and 428.4 ). S. aureus pneumonia often complicates an illness caused by influenza viruses.
| BACTERIAL | |
|---|---|
| COMMON | |
| Streptococcus pneumoniae | Consolidation, empyema |
| Group B streptococci | Neonates |
| Group A streptococci | Empyema |
| Staphylococcus aureus | Pneumatoceles, empyema; infants; nosocomial pneumonia |
| Mycoplasma pneumoniae * | Adolescents; summer–fall epidemics |
| Chlamydophila pneumoniae * | Adolescents |
| Chlamydia trachomatis | Infants |
| Mixed anaerobes | Aspiration pneumonia |
| Gram-negative enterics | Nosocomial pneumonia |
| UNCOMMON | |
| Haemophilus influenzae type b | Unimmunized |
| Moraxella catarrhalis | |
| Neisseria meningitidis | |
| Francisella tularensis | Animal, tick, fly contact; bioterrorism |
| Nocardia species | Immunocompromised patients |
| Chlamydophila psittaci * | Bird contact (especially parakeets) |
| Yersinia pestis (plague) | Rat contact; bioterrorism |
| Legionella species * | Exposure to contaminated water; nosocomial |
| Coxiella burnetii * (Q fever) | Animal (goat, sheep, cattle) exposure |
| VIRAL | |
| COMMON | |
| Respiratory syncytial virus | Bronchiolitis |
| Parainfluenza types 1-4 | Croup |
| Influenza A, B | High fever; winter months |
| Adenovirus | Can be severe; often occurs between January and April |
| Human metapneumovirus | Similar to respiratory syncytial virus |
| UNCOMMON | |
| Rhinovirus | Rhinorrhea |
| Enterovirus | Neonates |
| Herpes simplex | Neonates, immunocompromised persons |
| Cytomegalovirus | Infants; immunocompromised persons (particularly HIV-infected infants) |
| Measles | Rash, coryza, conjunctivitis |
| Varicella | Unimmunized; immunocompromised persons |
| Hantavirus | Southwestern United States, rodents |
| Coronaviruses [severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS)] | Asia, Arabian Peninsula |
| FUNGAL | |
| Histoplasma capsulatum | Ohio/Mississippi River valley; bird, bat contact |
| Blastomyces dermatitidis | Ohio/Mississippi River valley |
| Coccidioides immitis | Southwestern United States, Great Lakes states |
| Cryptococcus neoformans and C. gattii | Bird contact; immunocompromised; Northwestern United States (C. gattii) |
| Aspergillus species | Immunocompromised persons; nodular lung infection |
| Mucormycosis | Immunocompromised persons |
| Pneumocystis jiroveci | Immunocompromised persons (particularly HIV-infected infants); steroids |
| RICKETTSIAL | |
| Rickettsia rickettsiae | Tick bite |
| MYCOBACTERIAL | |
| Mycobacterium tuberculosis | Travel to endemic region; exposure to high-risk persons |
| Mycobacterium avium complex | Immunocompromised (particularly HIV-infected) persons |
| Other non-tuberculous mycobacteria | Immunocompromised persons; cystic fibrosis |
| PARASITIC | |
| Various parasites (e.g., Ascaris , Strongyloides species) | Eosinophilic pneumonia |
* Atypical pneumonia syndrome; may have extrapulmonary manifestations, low-grade fever, patchy diffuse infiltrates, and poor response to β-lactam antibiotics.
| AGE GROUP | FREQUENT PATHOGENS (IN ORDER OF FREQUENCY) |
|---|---|
| Neonates (<3 wk) | Group B streptococcus, Escherichia coli, other Gram-negative bacilli, Streptococcus pneumoniae, Haemophilus influenzae (type b, * nontypeable) |
| 3 wk-3 mo | Respiratory syncytial virus, other respiratory viruses (rhinoviruses, parainfluenza viruses, influenza viruses, human metapneumovirus, adenovirus), S. pneumoniae, H. influenzae (type b, * nontypeable); if patient is afebrile, consider Chlamydia trachomatis |
| 4 mo-4 yr | Respiratory syncytial virus, other respiratory viruses (rhinoviruses, parainfluenza viruses, influenza viruses, human metapneumovirus, adenovirus), S. pneumoniae, H. influenzae (type b, * nontypeable), Mycoplasma pneumoniae, group A streptococcus |
| ≥5 yr | M. pneumoniae, S. pneumoniae, Chlamydophila pneumoniae, H. influenzae (type b, * nontypeable), influenza viruses, adenovirus, other respiratory viruses, Legionella pneumophila |
* H. influenzae type b is uncommon with routine immunization.
| EXPOSURE HISTORY | INFECTIOUS AGENT |
|---|---|
| Exposure to concurrent illness in school dormitory or household setting | Neisseria meningitidis, Mycoplasma pneumoniae |
| ENVIRONMENTAL EXPOSURES | |
| Exposure to contaminated aerosols (e.g., air coolers, hospital water supply) | Legionnaires' disease |
| Exposure to goat hair, raw wool, animal hides | Anthrax |
| Ingestion of unpasteurized milk | Brucellosis |
| Exposure to bat droppings (caving) or dust from soil enriched with bird droppings | Histoplasmosis |
| Exposure to water contaminated with animal urine | Leptospirosis |
| Exposure to rodent droppings, urine, saliva | Hantavirus |
| Potential bioterrorism exposure | Anthrax, plague, tularemia |
| ZOONOTIC EXPOSURES | |
| Employment as abattoir work or veterinarian | Brucellosis |
| Exposure to cattle, goats, pigs | Anthrax, brucellosis |
| Exposure to ground squirrels, chipmunks, rabbits, prairie dogs, rats in Africa or southwestern United States | Plague |
| Hunting or exposure to rabbits, foxes, squirrels | Tularemia |
| Bites from flies or ticks | Tularemia |
| Exposure to birds (parrots, budgerigars, cockatoos, pigeons, turkeys) | Psittacosis |
| Exposure to infected dogs and cats | Pasteurella multocida, Q fever (Coxiella burnetii) |
| Exposure to infected goats, cattle, sheep, domestic animals, and their secretions (milk, amniotic fluid, placenta, feces) | Q fever (C. burnetii) |
| TRAVEL EXPOSURES | |
| Residence in or travel to San Joaquin Valley, southern California, southwestern Texas, southern Arizona, New Mexico | Coccidioidomycosis |
| Residence in or travel to Mississippi or Ohio river valleys, Great Lakes States, Caribbean, Central America, or Africa | Histoplasmosis, blastomycosis |
| Residence in or travel to southern China | SARS, avian influenza |
| Residence in or travel to Arabian peninsula | MERS-CoV |
| Residence in or travel to Southeast Asia | Paragonimiasis, melioidosis |
| Residence in or travel to West Indies, Australia, or Guam | Melioidosis |
S. pneumoniae, H. influenzae, and S. aureus are the major causes of hospitalization and death from bacterial pneumonia among children in developing countries, although in children with HIV infection, Mycobacterium tuberculosis (see Chapter 242 ), non-tuberculous mycobacteria (see Chapter 244 ), Salmonella (see Chapter 225 ) , Escherichia coli (see Chapter 227 ), Pneumocystis jiroveci (see Chapter 271 ), and cytomegalovirus (see Chapter 282 ) must be considered. The incidence of pneumonia caused by H. influenzae or S. pneumoniae has been significantly reduced in areas where routine immunization has been implemented.
Viral pathogens are the most common causes of lower respiratory tract infections in infants and children older than 1 mo but younger than 5 yr of age. Viruses can be detected in 40–80% of children with pneumonia using molecular diagnostic methods (e.g., polymerase chain reaction [PCR]). Of the respiratory viruses, respiratory syncytial virus (RSV; see Chapter 287 ) and rhinoviruses (see Chapter 290 ) are the most commonly identified pathogens, especially in children younger than 2 yr of age. However, the role of rhinoviruses in severe lower respiratory tract infection remains unclear as these viruses are frequently detected with co-infecting pathogens and among asymptomatic children. Other common viruses causing pneumonia include influenza viruses (see Chapter 285 ), human metapneumovirus (see Chapter 288 ), parainfluenza viruses (see Chapter 286 ), adenoviruses (see Chapter 289 ), and enteroviruses (see Chapter 277 ). Infection with more than one respiratory virus occurs in up to 20% of cases. The age of the patient can suggest the likely pathogens (see Table 428.3 ).
Lower respiratory tract viral infections are much more common in the fall and winter in both the northern and southern hemispheres in relation to the seasonal epidemics of respiratory viruses that occur each year. The typical pattern of these epidemics usually begins in the fall, when parainfluenza virus infections appear and most often manifest as croup. Later in winter, RSV, human metapneumovirus, and influenza viruses cause widespread infection, including upper respiratory tract infections, bronchiolitis, and pneumonia. RSV is particularly severe among infants and young children, whereas influenza viruses cause disease and excess hospitalization for acute respiratory illness in all age groups. Knowledge of the prevailing viruses circulating in the community may lead to a presumptive initial diagnosis.
Immunization status is relevant because children fully immunized against H. influenzae type b and S. pneumoniae are less likely to have pneumonia caused by these pathogens. Children who are immunocompromised or who have certain medical comorbidities may be at risk for specific pathogens, such as Pseudomonas spp. in patients with cystic fibrosis (see Chapter 432 ).
The lower respiratory tract possesses a number of defense mechanisms against infection, including mucociliary clearance, macrophages and secretory immunoglobulin A, and clearing of the airways by coughing. Previously, it was believed that the lower respiratory tract was—in the absence of infection—kept sterile by these mechanisms, supported primarily by culture-based studies. However, recent use of culture-independent techniques, including high-throughput sequencing methods, suggests that the lower respiratory tract contains diverse microbial communities. These data have challenged the traditional model of pneumonia pathogenesis that maintained that pneumonia was the result of invasion of the sterile lower respiratory tract by a single pathogen. More recent conceptual models postulate that pneumonia results from disruption of a complex lower respiratory ecosystem that is the site of dynamic interactions between potential pneumonia pathogens, resident microbial communities, and host immune defenses.
Viral pneumonia usually results from spread of infection along the airways, accompanied by direct injury of the respiratory epithelium, which results in airway obstruction from swelling, abnormal secretions, and cellular debris. The small caliber of airways in young infants makes such patients particularly susceptible to severe infection. Atelectasis, interstitial edema, and hypoxemia from ventilation–perfusion mismatch often accompany airway obstruction. Viral infection of the respiratory tract can also predispose to secondary bacterial infection by disturbing normal host defense mechanisms, altering secretions, and through disruptions in the respiratory microbiota.
Bacterial pneumonia most often occurs when respiratory tract organisms colonize the trachea and subsequently gain access to the lungs, but pneumonia may also result from direct seeding of lung tissue after bacteremia. When bacterial infection is established in the lung parenchyma, the pathologic process varies according to the invading organism. M. pneumoniae (see Chapter 250 ) attaches to the respiratory epithelium, inhibits ciliary action, and leads to cellular destruction and an inflammatory response in the submucosa. As the infection progresses, sloughed cellular debris, inflammatory cells, and mucus cause airway obstruction, with spread of infection occurring along the bronchial tree, as is seen in viral pneumonia. S. pneumoniae produces local edema that aids in the proliferation of organisms and their spread into adjacent portions of lung, often resulting in the characteristic focal lobar involvement. Group A streptococcus lower respiratory tract infection typically results in more diffuse lung involvement with interstitial pneumonia. The pathology includes necrosis of tracheobronchial mucosa; formation of large amounts of exudate, edema, and local hemorrhage, with extension into the interalveolar septa; and involvement of lymphatic vessels with frequent pleural involvement. S. aureus pneumonia manifests as confluent bronchopneumonia, which is often unilateral and characterized by the presence of extensive areas of hemorrhagic necrosis and irregular areas of cavitation of the lung parenchyma, resulting in pneumatoceles, empyema, and, at times, bronchopulmonary fistulas.
Recurrent pneumonia is defined as 2 or more episodes in a single year or 3 or more episodes ever, with radiographic clearing between occurrences. An underlying disorder should be considered if a child experiences recurrent pneumonia ( Table 428.5 ).
| HEREDITARY DISORDERS |
|
| DISORDERS OF IMMUNITY |
|
| DISORDERS OF CILIA |
|
| ANATOMIC DISORDERS |
|
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here