Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The modern battlefield is a highly complex and deadly arena that continues to drive innovation and advancements in both civilian and military trauma care. Prior to World War I, the vast majority of battlefield morbidity and mortality was due to infectious and other medical diseases. Simultaneous advances in medicine and weaponry subsequently resulted in trauma becoming the predominant focus of battlefield medicine. The historical practice of deploying civilian health care personnel who were activated only during times of war has given way to the development of a full-time dedicated military medical service that maintains constant readiness to provide comprehensive battlefield trauma care. The terrorist attacks of September 11, 2001, resulted in the first large-scale and prolonged forward deployment of military medical assets since the Vietnam War. Although a full description of the breadth and depth of trauma experience gained from these conflicts is not possible here, the purpose of this chapter is to highlight some of the major lessons learned (and relearned) over the past two decades of sustained combat and other forward medical operations.
Although the exact configuration and personnel requirements vary widely between specific types of units and the military services (Army, Navy, Air Force, etc.), they all follow some basic principles of organization and capabilities. This allows for both the flexibility and stability required to function in a variety of combat environments and circumstances. Battlefield medicine always starts at the point of injury, with immediate care provided by fellow soldiers (“buddy aid”) and combat medics or corpsman. Formal medical care is then organized in a series of Roles (also commonly referred to as “Levels” or “Echelons”), from Role 1 through Role 5 as outlined in Table 1 . Surgical care is first available at Role 2 facilities and focuses on damage control and stabilization. Of note, an important lesson learned is that the more severely injured patient should be transported immediately to the most appropriate facility, which often means bypassing Role 1 or even Role 2 and going directly to a Role 3 facility. In addition, a variety of smaller “austere surgical teams” have now been pushed further forward (to the traditional Role 1 environment) in select situations or missions.
| Echelon | Example | Surgical Capability | Other Capabilities | Comments |
|---|---|---|---|---|
| Role 1 | Battalion aid station, shock trauma platoon | None | “Aid bag,” limited supplies, maybe ultrasound | Medics and PA or primary care MD; no hold capability |
| Role 2 |
|
Yes, general and orthopedics; sustained OR capability for 24–48 hours | Damage control surgery, basic lab, basic radiograph and ultrasound, oxygen, limited blood product supply | Focus on damage control and immediate MEDEVAC to Level 3; team may move to follow operational unit or split to cover two areas |
| Role 3 |
|
Yes, general and orthopedic surgery, surgical and medical subspecialties | Multiple specialists, advanced lab and blood product support, advanced radiology and CT, physical therapy | Damage control surgery and definitive management; stabilization and evacuation portal to Level 4 |
| Role 4 | Regional medical center (Landstuhl, Germany) | Extensive, excellent subspecialty support | Major medical center capabilities | More definitive surgical intervention; burns may bypass directly to Brooke Burn Center |
| Level 5 | CONUS national medical centers (Walter Reed, Bethesda, Balboa, Brooke) | Full tertiary care | Full rehabilitation and specialty intervention | Performs most delayed and reconstructive care |
An understanding of the predominant injury mechanisms, patterns, and anatomic wound distributions is critical to adequately deploying and maximizing battlefield medical assets. These may be unique to each combat theater and may even vary significantly by the phase of operations. This was seen in the recent combat operations in Iraq and Afghanistan, with a marked difference in wounding mechanisms and lethality between the initial invasion phase and the subsequent insurgency and stabilization phases. Unlike civilian trauma, battlefield injuries are characterized by a predominance of penetrating and often high-velocity mechanisms, severe multisystem trauma, mangled and amputated extremities. The majority of these injury types require some type of operative intervention. One of the defining factors of modern combat operations has been the widespread use of the improvised explosive device, or IED ( Fig. 1 ). These devices can be assembled around almost any explosive source and vary widely in size, triggering mechanisms, and resultant blast force ( Fig. 2 ). In contrast to previous conflicts, only a small portion of traumatic wounds in the current conflicts are from firearms (25%), while the majority (60%) has been from explosive mechanisms. The resultant combination of explosive injury with associated blast, blunt force trauma, and penetrating fragment wounds often creates a severe and complex battle injury that has no true civilian counterpart.


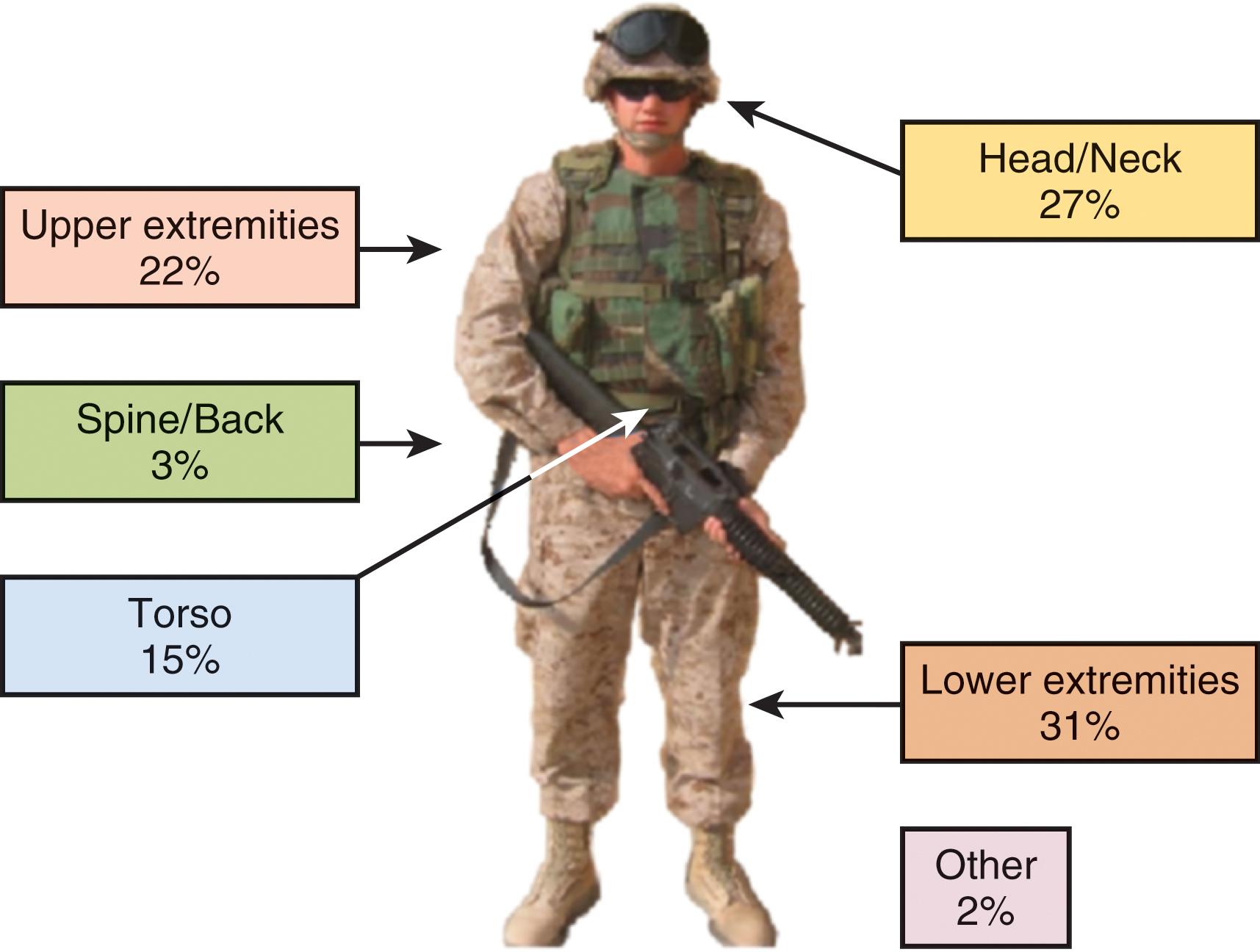
As a result of the detailed and thorough collection of wounding data, therapy, and outcomes with the Joint Theater Trauma Registry, the anatomic distribution and severity of combat injuries can be analyzed and used to drive real-time changes in prevention and treatment. Modern developments such as advanced body armor, explosive-resistant vehicles, and changes in operational tactics have been partially based on this data. Figure 3 shows the composite distribution of anatomic sites of battlefield injuries seen during the current combat operations, and Table 2 shows the various anatomic wound distributions compared with previous conflicts. The exact distribution and severity will also be greatly dependent on individual factors, such as the presence of body armor, vehicular or dismounted injury, and the wounding mechanism.
| Body Surface Area (%) | WWII (%) | Korea (%) | Vietnam (%) | OIF/OEF (%) | |
|---|---|---|---|---|---|
| Head/neck | 12 | 21 | 21 | 16 | 30 |
| Thorax | 16 | 14 | 10 | 13 | 6 |
| Abdomen | 11 | 8 | 8 | 9 | 9 |
| Extremities | 61 | 58 | 60 | 61 | 55 |
Battlefield deaths are a particular point of interest and have been analyzed in great detail over the past decade of combat operations. Two excellent analyses of autopsy and clinical data from Operation Iraqi Freedom (OIF)/Operation Enduring Freedom (OEF) have described the predominant mechanisms (blast and gunshot) and injury sites (head and trunk) resulting in death on the battlefield. Of interest, up to 28% of deaths were deemed to be potentially survivable with the majority of those (80%) being due to hemorrhage. Another analysis of these data has demonstrated that the case fatality rate (CFR) for Iraq/Afghanistan was approximately half of that seen in prior conflicts (10.5% vs 20.2%), possibly attributed to improved protective equipment, evacuation capability, and prehospital care. However, there has been a concurrent increase in those who died of wounds (DOW) after reaching a medical facility, from 3% in World War II and Vietnam to as high as 5% for Afghanistan. This concerning statistic likely reflects the ability to get more severely injured patients quickly evacuated to a medical facility and highlights the need for forward medical facilities and personnel prepared to deal with these high-acuity injuries. A detailed analysis of in-hospital deaths from a Combat Support Hospital in Iraq highlights the need for rapid definitive intervention, with the majority of deaths even at the in-hospital level occurring within the first hour of arrival (78%) and attributable to hemorrhage (62%).
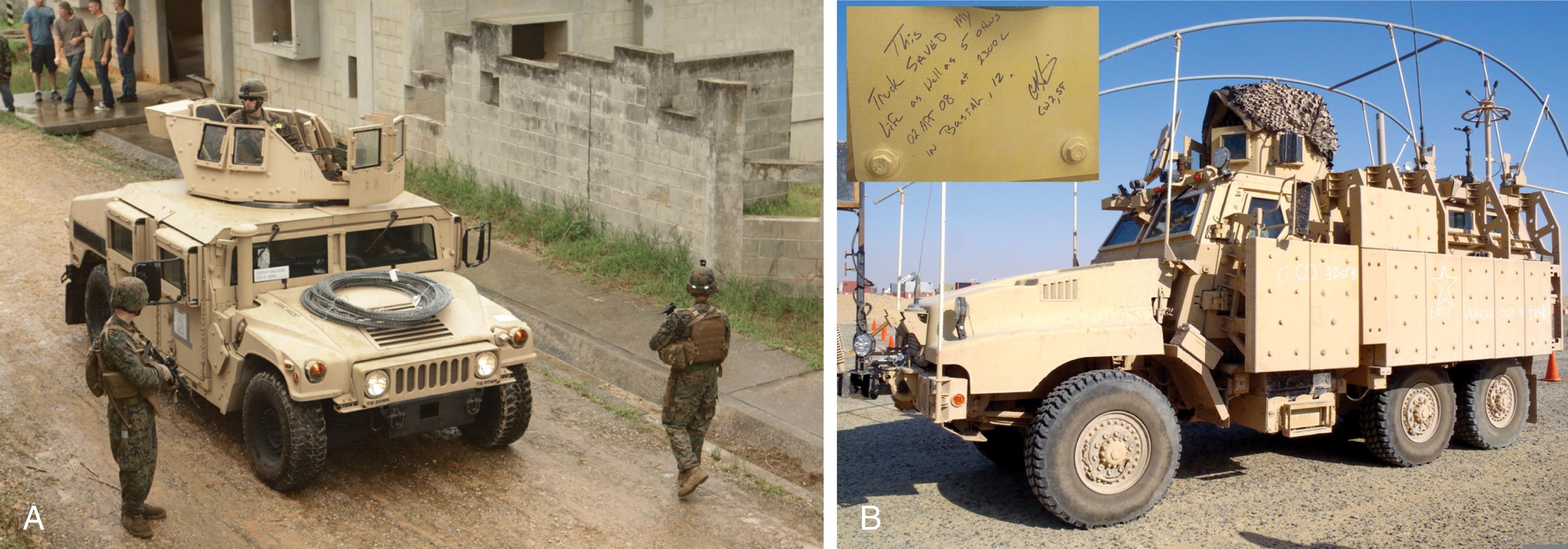
The sharp decline in killed in action and case-fatality ratios during recent combat operations is multifactorial and has been attributed to both improvements in personal protective equipment and vehicles as well as improved medical care. Initial improvements to enhance survivability from IED blasts included modifications to currently available military vehicles, followed by the deployment of new vehicles (Mine-Resistant Ambush Protected or MRAP) specifically designed to withstand larger explosive forces ( Fig. 4 ). Although definitive data are lacking, there appears to be a significant (up to 90%) reduction in IED-related fatalities among passengers in MRAP-type vehicles. Arguably, an equally important factor in improving battlefield survival in OIF/OEF has been the massive investment in equipping and training military first responders and medical evacuation (MEDEVAC) personnel. The Tactical Combat Casualty Care (TCCC) course is the military adaptation of the widely used civilian prehospital trauma courses and provides realistic and up-to-date training and information aimed at maximizing survival on the battlefield. Unlike most civilian settings, combat medics have to deliver initial care in a hostile environment and often while receiving direct or indirect fire from enemy forces. The TCCC course outlines principles and priorities for three phases of prehospital care: (1) care under fire, (2) tactical field care, and (3) tactical evacuation care as shown in Table 3 . In distinction from the commonly taught ABC (airway, breathing, circulation) for civilian trauma, combat medics are trained to prioritize hemorrhage control (C) first, and then move on to airway and breathing issues. This change in ideology is slowing making its way into the protocols of many civilian trauma centers and prehospital organizations.
| Care under fire |
|
| Tactical field care |
|
| Tactical evacuation care |
|
Analysis of battlefield deaths and preventable deaths has resulted in rapid training and fielding initiatives to better equip military first responders. One of the most important interventions during the early phases of these conflicts was the widespread deployment of manually operated extremity tourniquets, and currently each soldier carries his or her own tourniquet so that it is readily available and applied if needed ( Fig. 5 ). In addition to the standard gauze field dressing, medics were equipped for the first time with advanced hemostatic dressing products, including the HemCon bandage (HemCon Medical Technologies, Portland, OR) and the granular agent QuikClot (Z-Medica, Wallingford, CT). Subsequently, a next-generation kaolin-coated gauze roll (QuikClot Combat Gauze, Z-Medica Inc.) with superior efficacy was widely deployed and is the current TCCC recommended hemostatic dressing. Two additional chitosan-based gauze dressings have also recently been added to the list of TCCC-approved hemostatic dressings. Current research is focused on developing the next generation of hemostatic dressings that contain active clotting factors and advanced biomaterials that may be more efficacious even in patients with major acidosis and coagulopathy. Other equipment items and changes include longer large-bore needle thoracostomy catheters (3.25 inches), intraosseous access devices, and self-contained hypothermia prevention and management (HPMK) kits. Prehospital fluid resuscitation has also undergone significant changes based on current combat experience, with a focus on low-volume initial resuscitation, avoidance of large volumes of crystalloid, and earlier use of blood products, specifically whole blood, for evidence of shock. If a rapid assessment for shock (mental status and radial pulse) is normal, then no fluids are given. If abnormal or if there are clear signs of ongoing hemorrhage, then the current TCCC resuscitative fluid of choice is whole blood. If whole blood is not readily available, then a balanced ratio of red cells to plasma is next in preference, followed by either red cells alone or plasma alone. Although previous iterations of TCCC have recommended small-volume synthetic colloid (Hextend) boluses, all crystalloids and colloids have been removed from the most recent TCCC guidelines for prehospital fluid resuscitation.

Although the military utilizes a wide variety of vehicular platforms for front-line evacuation of wounded patients, the vast majority of MEDEVAC missions in Iraq and Afghanistan are performed by rotary wing aircraft, typically utilizing the Blackhawk helicopter ( Fig. 6 ). Although the exact staffing and training of the medical evacuation (MEDEVAC) crew members varies widely between military services, there is a common focus on rapid evaluation of the patient, continuing prehospital care and resuscitation, and evacuation to a Role 2 or 3 facility as quickly as possible. Frequent challenges encountered during these missions include danger from enemy fire, heat and noise, a dirty/dusty environment, operating in low-light or blackout conditions (particularly during night operations), multiple simultaneous casualties, and the difficulty of performing in-flight advanced care or procedures. Multiple initiatives examined ways to mitigate some of these limitations and included pilot projects assessing the impact of deploying advanced skill providers (critical care nurses, physicians, surgeons) and resuscitation supplies (blood products, rapid infusers) with MEDEVAC crews to provide oversight and additional advanced “golden hour” care capabilities. These have now become standard among most deployed MEDEVAC platforms, particularly the capability for en route resuscitation with blood products for select combat casualties.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here