Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Colonic intussusception is a rare diagnosis in adults. This process occurs when a proximal segment of intestine (intussusceptum) invaginates into a distal segment of intestine (intussuscipiens) with 86% to 90% associated with a pathologic lesion as the lead point. The exact mechanism of intussusception in adults is not completely understood. It is proposed that the presence of a stimulus in the lumen of the bowel induces constriction of the bowel proximal to the stimulus and relaxation of the bowel wall distally allowing for invagination of the proximal segment. Intussusception is categorized into two discrete categories: enteric in which solely the jejunum or ileum are involved, and colonic, which includes ileocolic, colocolonic, and colorectal configurations. Often, the stimulus responsible for intussusception in adults is a gastrointestinal (GI) neoplasm with 56% of colonic intussusceptions attributed to malignancy and approximately 19% of enteric intussusceptions related to malignancy. Benign causes include benign GI neoplasms, adhesive disease, Meckel diverticulum, sprue, human immunodeficiency virus (HIV), or idiopathic intussusception.
Intussuception accounts for 1% of bowel obstructions and symptoms of complete obstruction occur in fewer than 20% of cases. Unlike the presenting classic triad of abdominal pain, palpable abdominal mass, and heme-positive stools described in the pediatric population, adult patients rarely present with signs of acute obstruction. The most common presenting symptoms are crampy abdominal pain (71%), nausea and emesis (68%), abdominal distention (45%), and tenderness (60%). Most patients have a history of subacute partial obstruction or intermittent obstruction occurring over days to years. For this reason, misdiagnosis is common, with a majority of cases diagnosed at the time of laparotomy.
Plain radiographs can be helpful to identify cases of enteric intussusception without colonic involvement. Contrast studies subsequently delineate the site of intussusception. In cases of enteric intussusception, upper GI series will show a “stacked coin” or “coiled spring” appearance.
Barium enema can subsequently be used to identify colonic obstruction, which will demonstrate a cup shaped filling defect representing the distal extent of the intussusceptum within the lumen of the colon. It is important to note that hydrostatic pressure should not be used in adults as an attempt to reduce the intussusception due to the risk of underlying malignancy and risk of perforation. Barium studies are contraindicated if there is concern for bowel perforation or ischemia.
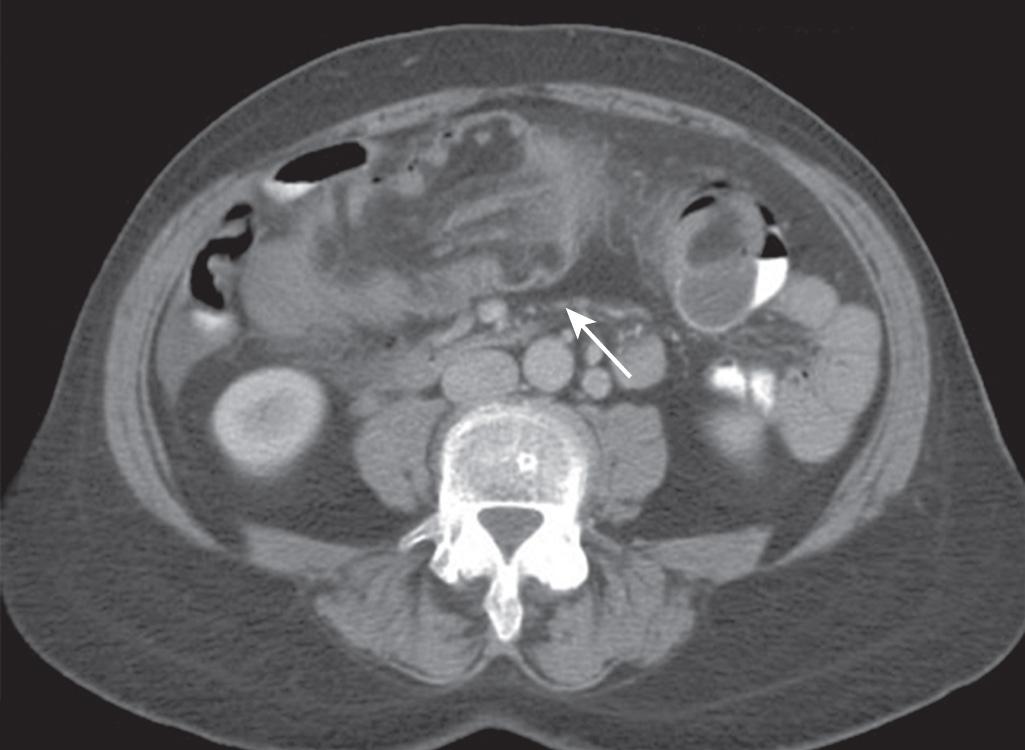
Computed tomorgraphy (CT) scan is the most accurate imaging modality for the diagnosis of intussusception and is often the imaging of choice for patients who present with the nonspecific symptoms of intussusception including obstruction or palpable abdominal mass. Characteristic findings on CT include a “target sign” in which the intussusceptum and associated mesentery is seen within the lumen of the intussuscipiens in axial view. This “bowel-within-bowel” configuration where mesenteric vessels can be seen compressed between the walls of the small bowel is pathognomonic for intussusception ( Fig. 155.1 ).
Ultrasound is a readily available noninvasive method of evaluation that is typically used in diagnosis of pediatric intussusception. Ultrasound has less accuracy for the diagnosis of intussusception in adults but can identify characteristic findings including the “target” and “donut” sign when evaluating the intussusception in transverse view. The “pseudo-kidney” sign is seen when evaluating the intussusception longitudinally. The quality of ultrasound imaging may be variable depending on the experience of the operator, the body habitus of the patient, and the presence of bowel gas that may obscure underlying structures.
Flexible sigmoidoscopy or colonoscopy can be used in the case of subacute or chronic colonic obstruction as a means of diagnosis of a suspected colonic malignancy. In cases of chronic tissue ischemia or necrosis, biopsy or polypectomy is not recommended.
Surgery is the primary treatment for adult intussusception. There is no role for nonoperative or endoscopic management given the high likelihood of malignancy as the underlying cause, especially so in patients over the age of 60. Resection allows for removal of a potentially malignant lesion and prevents recurrence of intussusception. Resection should proceed as a formal oncologic resection including lymphadenectomy of the affected small bowel or colon segment.
For this reason, reduction of colonic intussusception is discouraged. Care should be taken to avoid trauma to the already compromised bowel wall and prevent perforation with seeding of the peritoneal cavity. Often the intussuscepted bowel is inflamed, edematous, or ischemic, which increases the risk of perforation. Enteric intussuception has a lower associated malignancy rate of 19% but has been reported to be up to 47% in some case series. Although some reports advocate for reduction in the setting of enteric intussusception, others recommend that reduction should be avoided unless benign etiology is confirmed or radical resection would render the patient at risk for short gut syndrome. In cases of postoperative or adhesion related intussuception, the intussusception can be reduced as benign etiology is assumed.
Colonic volvulus represents 1.9% of cases of large bowel obstruction in the United States and up to 10% to 50% of cases in Africa, the Middle East, and South America. Volvulus occurs when a segment of colon undergoes torsion along its own mesentery (mesenterioaxial) resulting in obstruction. Torsion of 180 degrees results in clinical obstruction, and further torsion to 360 degrees causes strangulation with venous gangrene, ischemia, and eventual perforation. As the volvulized segment enlarges, it becomes trapped in the confines of the abdominal wall and is unable to spontaneously detorse. Perforation occurs in areas of necrosis at the point of torsion, within the closed loop, or in the proximal thin-walled cecum.
Segments of colon that are redundant with an elongated mesentery and narrow base are more likely to undergo torsion; for this reason, the sigmoid, cecum, and the transverse colon are most commonly susceptible to volvulus.
In both subtypes, acquired changes to the sigmoid colon and mesocolon result in lengthening of colon between two relatively close points of mesenteric fixation: the distal descending mesocolon and the mesorectum at the rectosigmoid junction. In anatomic studies, Bhatnagar et al. describes the “dolichomesocolic colon,” one that is vertically longer than it is wide. This anatomic configuration is more commonly found in male subjects and people over the age of 30. The incidence of sigmoid volvulus peaks in the mid-70s for both men and women suggesting that this process is secondary to chronic changes. Other theories support congenital configurations that predispose to volvulus owing to its relative frequency within certain tribes and its propensity for the male gender. Ultimately the exact reason for why this anatomic configuration occurs is not completely understood and may be multifactorial.
Sigmoid volvulus is also the most common cause of intestinal obstruction in pregnancy, accounting for 45% of obstructions in this group. The vague presenting symptoms of sigmoid volvulus contribute to a higher rate of misdiagnosis with maternal mortality reported at 5% but up to 50% in the setting of perforation. Fetal demise approaches 30% and is secondary to reduction in placental blood flow due to mass effect from a massively dilated sigmoid. Other conditions that predispose to sigmoid volvulus include postoperative adhesions and megacolon, in particular Hirschsprung disease, due to massive dilation of the colon.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here