Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
It seems as if surgeons have always debated the “proper” treatment of colorectal injuries, including the following issues:
When should continuity be restored, and when should diversion be implemented?
Should left-sided colon injuries be treated differently from right-sided colon injuries?
Are drains useful in rectal injuries?
Should direct repair be a standard component of surgical management of rectal trauma?
Is rectal washout a helpful or a harmful procedure?
Answers to these seemingly straightforward questions are controversial. Our goal in this chapter is to provide answers based on the current evidence and experience.
Colon and rectal trauma occurs in 0.1% to 15% of injured patients, depending on the underlying mechanism of the injury and the environment in which it occurs. Similar to trauma in other organ systems, the causes of colorectal trauma can be divided into blunt and penetrating. Hollow-viscus injuries are less common after blunt force trauma than with penetrating wounds and typically occur only with high-energy transfer. As such, they are often accompanied by concomitant abdominal, thoracic, neurologic, and orthopedic injuries. Injury patterns also differ between civilian life and wartime. With combat zone experiences, in general, a higher incidence of colonic injuries is reported (5% to 15%), whereas most civilian series cite rates of less than 5%. Rectal injuries may occur as a result of a direct injury from a projectile, as a result of bony fragments from pelvic fractures, or via foreign body insertion. Finally, blast injuries, such as those seen in a war zone or explosion, are becoming more commonplace and may result in damage to the colon or rectum from either the pressure wave itself or from shrapnel caused by the explosion.
Assessment begins with a standard evaluation using Advanced Trauma Life Support guidelines. After the primary survey and concomitant resuscitation, a specific evaluation for colon and rectal injuries involves an abdominal examination with emphasis on identification of injuries, exposed intra-abdominal contents, or peritonitis that may mandate an urgent exploration ( Fig. 67-1 ). Rectal examination is performed to assess sphincter tone, presence of blood, a high-riding prostate (i.e., a possible urethral injury), or fragments that may indicate a bony injury to the rectal wall. Digital rectal examination (DRE) has had varying success in detecting rectal injury. In a series of 77 patients who sustained penetrating pelvic wounds, DRE was compared with rigid sigmoidoscopy. Overall sensitivity for the detection of injury was higher with rigid sigmoidoscopy (78% vs. 51%), with rates even higher for extraperitoneal (88%) versus intraperitoneal (58%) locations. This low sensitivity with DRE has caused some investigators to question its utility as a part of the secondary evaluation; rather, they promote reliance on a high index of suspicion using other clinical factors such as the presence of gastrointestinal bleeding, urethral disruption, or spinal cord injury. Furthermore, DRE alone has had poor correlation with determining the presence of concomitant injuries, with one series reporting an accuracy of 23% (95% confidence interval [CI], 16% to 30%). Despite these concerns, DRE has little downside, can demonstrate soft tissue or sphincter injuries that may need treatment ( Fig. 67-2 ), and when combined with rigid proctosigmoidoscopy, has the ability to identify injuries that otherwise may not be found with imaging alone. Therefore, although a negative examination doesn’t necessarily rule out an injury, a positive examination is critical, and surgeons should always have a high index of suspicion for injuries.


Imaging plays a major role in diagnosing colon and rectal injuries. Similar to other hollow-viscus injuries, perforation of the colon or intraperitoneal rectal wall may cause a pneumoperitoneum that is best seen on an upright chest radiograph. In contrast, damage to the extraperitoneal rectum or retroperitoneal portion of the colon (such as that seen in flank stab wounds) may not demonstrate any free air.
A focused assessment with sonography for trauma (FAST), although not specific for colorectal trauma, may provide information that can indicate a possible injury. Demonstration of intra-abdominal free fluid in the absence of a defined solid organ injury, especially when it is more than trace pelvic fluid, correlates with higher rates of therapeutic laparotomy after blunt trauma is sustained. Other concomitant findings such as a seat belt sign or a Chance-type spinal fracture in this setting of free fluid should lead to an even higher degree of suspicion for an underlying clinically significant visceral injury. Ultrasonography also can be useful in perineal injuries to confirm or identify suspected sphincter injuries ( Fig. 67-3 ). Similar to a tear during obstetric delivery, disruption of the external sphincter ( Fig. 67-4 ) can be demonstrated by a lack of a continuous hyperechoic ring.


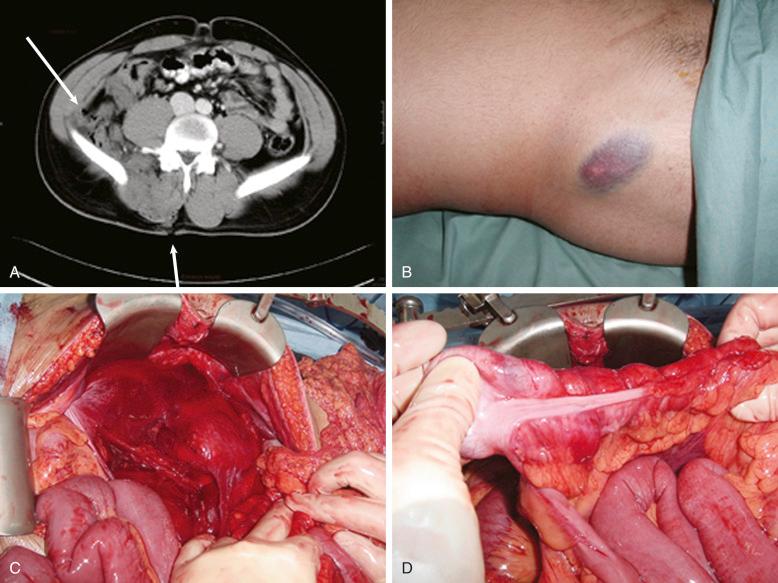
Computed tomography (CT) remains the mainstay of radiologic testing for colorectal injuries. Most imaging pathways utilize CT in hemodynamically stable patients directly or after identification of free fluid upon FAST examination. Sensitivities, specificities, negative predictive value, and accuracy rates of greater than 95% have been reported in many studies. With the widespread availability of multi-row detector CT scans, scanning times have significantly shortened, and thin slicing has allowed demonstration of both direct bowel wall damage and secondary signs of injury (i.e., free fluid, inflammation, contrast extravasation, free air, and bony fragments). In addition, the improved technology allows for evaluation of the tract of a projectile/bullet, which can provide some insight as to potential injuries ( Fig. 67-5, A-D ). Various protocols are in place, including the use of oral, rectal, and intravenous (IV) contrast material. In general, CT of the head, chest, abdomen, and pelvis with IV contrast material is used initially and permits identification of concomitant injuries.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here