Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Sinonasal malignancies are rare with annual incidence rates near 1 per 100,000 in most industrialized countries and represent fewer than 4% of neoplasms arising in the head and neck. , The most common malignant tumors of the anterior skull base derive from the paranasal sinuses or nasal cavity. Although squamous cell carcinoma (SCC) represents the most common type of malignant sinonasal tumor, there are a wide variety of other histologic tumor subtypes in this location.
The World Health Organization Histologic Classification of Paranasal Sinus Malignancies includes the following:
Epithelial Malignancies
SCC
Verrucous carcinoma
Papillary SCC
Basaloid SCC
Spindle cell carcinoma
Adenosquamous carcinoma
Acantholytic SCC
Lymphoepithelial carcinoma
Sinonasal undifferentiated carcinoma
Adenocarcinoma
Intestinal-type adenocarcinoma
Non–intestinal-type adenocarcinoma
Salivary gland-type carcinomas
Adenoid cystic carcinoma
Acinic cell carcinoma
Mucoepidermoid carcinoma
Epithelial–myoepithelial carcinoma
Clear cell carcinoma not otherwise specified
Myoepithelial carcinoma
Carcinoma ex pleomorphic adenoma
Polymorphous low-grade adenocarcinoma
Neuroendocrine tumors
Typical carcinoid
Atypical carcinoid
Small cell carcinoma, neuroendocrine type
Soft Tissue Malignancies
Fibrosarcoma
Malignant fibrous histiocytoma
Leiomyosarcoma
Rhabdomyosarcoma
Angiosarcoma
Malignant peripheral nerve sheath tumor
Bone and Cartilage Malignancies
Chondrosarcoma
Mesenchymal chondrosarcoma
Osteosarcoma
Chordoma
Hematolymphoid Malignancies
Extranodal natural killer/T-cell lymphoma
Diffuse large B-cell lymphoma
Extramedullary plasmacytoma
Extramedullary myeloid sarcoma
Histiocytic sarcoma
Langerhans cell histiocytosis
Neuroectodermal Malignancies
Ewing sarcoma
Primitive neuroectodermal tumor
Olfactory neuroblastoma
Melanotic neuroectodermal tumor of infancy
Mucosal malignant melanoma
Germ Cell Malignancies
Teratoma with malignant transformation
Sinonasal teratocarcinosarcoma
These tumors pose a multitude of problems because of their diversity, rareness, propensity for late presentation, and proximity to critical structures, including the orbit, skull base, and brain. This chapter presents an overview of the considerations when performing a clinical evaluation of patients with skull base malignancies.
The clinical evaluation of a patient with a suspected skull base malignancy starts with a detailed review of the patient’s records, which includes the referring physician’s concern, laboratory values, diagnostic studies, operative reports, and pathology results.
A thorough clinical history should follow with determination and documentation of the patient’s chief complaint and review of the history of present illness.
Many symptoms on presentation are nonspecific and can make the identification of paranasal cancers and skull base malignancies difficult. Patients commonly report unilateral nasal obstruction. A retrospective review of more than 100 patients by Jackson et al. found that the most common complaints were nasal obstruction (61%), localized pain (43%), epistaxis (40%), swelling (29%), nasal discharge (26%), and epiphora (19%). Paranasal sinus tumors can have an insidious onset until involvement of adjacent structures leads to more severe symptomatology and resulting clinical presentation.
Certain symptoms may indicate the extent and spread of disease. Epiphora suggests blockage or infiltration of the lacrimal apparatus either proximally or distally. Diplopia or vision changes suggest involvement at the orbital apex or cavernous sinus. Trismus can be from tumor extension into the pterygoid musculature. Facial numbness implies involvement of the trigeminal nerve likely related to perineural invasion. Hearing loss could indicate tumor advancement into the eustachian tube. Loose, nonviable teeth indicate inferior bony involvement. Clear rhinorrhea can be a symptom of cerebrospinal fluid (CSF) leakage.
A social history should follow with a detailed review of tobacco and occupational exposures. Tobacco smoking and other lifestyle factors seem to play an overall minor role in the development of sinonasal cancers. , A number of substances and occupational exposures have been linked with the development of sinonasal malignancies. A systematic review and meta-analysis of occupational exposure and sinonasal cancer found an increased risk of sinonasal cancer from exposure to wood dust, leather dust, formaldehyde, nickel–chromium compounds, organic solvents, welding fumes, and arsenic.
Patients should be screened for overall health changes, including weight loss and fatigue, which can be indicative of an underlying malignancy.
A thorough head and neck physical examination must be conducted during the workup of these patients. The relevant components of the full head and neck physical examination are highlighted here for the evaluation of patients with skull base malignancies. This examination begins with a general assessment of the patient’s appearance, vital signs, and mental status.
The head and neck should be assessed for overall shape, symmetry, and signs of trauma. Distortion of facial anatomy and asymmetry should be noted, which can be indicative of an underlying malignancy. The facial skeleton should be carefully palpated for bony deformities with special attention given to the areas overlying the paranasal sinuses.
The eyes should be examined with assessment of the rounding of the canthi or an increase in intercanthal distance. Conjunctiva and sclera should be inspected as well as the eyelids for ptosis, injection, chemosis, and proptosis. Visual acuity, color vision, extraocular movements, and pupillary reaction to light should be evaluated to assess for any involvement of the cranial nerves of the eye.
The external nose should be examined for any deformity or asymmetry. Anterior rhinoscopy should be performed to assess the nasal septum and inferior turbinates. The quality of the septum should be noted as well as integrity of the mucosa. Any significant septal deviation or turbinate hypertrophy should be documented. Any extensive rhinorrhea should be noted as a concern for CSF leak.
Otologic examination should be performed, looking for evidence of eustachian tube dysfunction or obstruction, including serous otitis media or acute otitis media.
Oral cavity examination may detail tumor extension in the nasopharynx or oropharynx, erosion into the soft and hard palate, or loosened or poor dentition.
Palpation of the neck for any masses or lymphadenopathy should also be performed. The incidence of cervical metastases varies by pathology, but typically fewer than 10% of patients present with nodal disease. ,
Routine assessment requires evaluation of the function of the cranial nerves. Given that anterior skull base malignancies can present with palsies of the cranial nerves, it is critical to assess smell, vision, extraocular motion, and facial sensation. Cranial neuropathies of CNs II, III, IV, V1, V2, and VI are most common and can represent advanced disease. Patients with tumors of the ethmoids can present with anosmia or an altered sense of smell. Although both disease itself and surgical treatment can contribute to a loss of smell, techniques to preserve smell have been described.
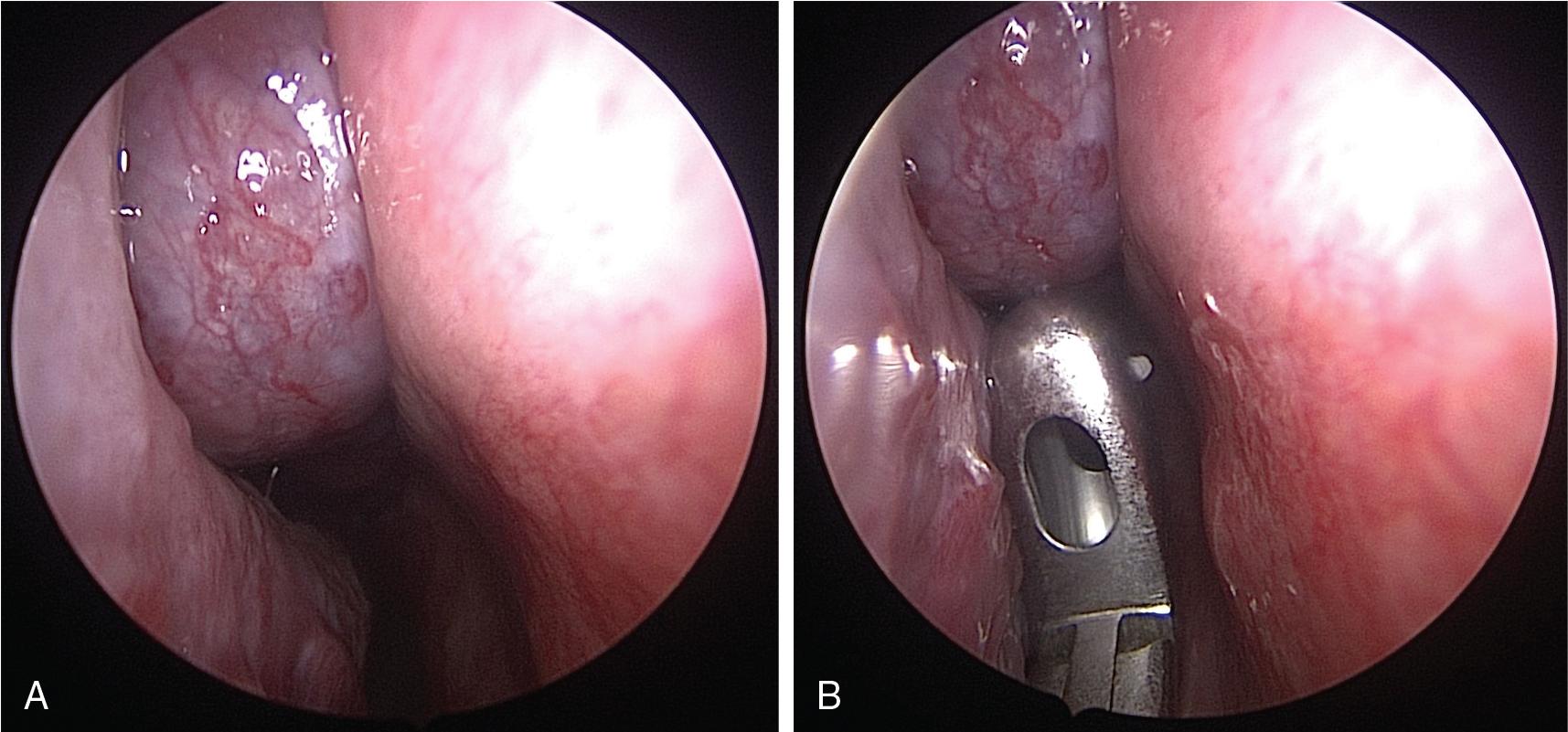
Rigid nasal endoscopic examination is preferred over flexible fiberoptic laryngoscopy. The rigid endoscopic examination allows for better optical visualization and ability to use a second hand to palpate the lesion to assess for surrounding structure involvement as well as biopsy if needed ( Fig. 26.1 A). Angled endoscopes may be used to increase visualization as needed. If further visualization is needed past the nasopharynx given lesion extension, a flexible endoscope may be used.
After applying a local anesthetic and topical decongestant spray, endoscopy is performed. The entire nasal cavity should be inspected in detail. The quality and character of the nasal mucosa should be assessed with attention given to any purulence or crusting. If purulence is present, this should be cultured and can be indicative of an associated chronic sinusitis. The examination should be conducted in inferior-to-superior and anterior-to-posterior directions. The inferior turbinate and meatus are inspected with visualization of any pathology at Hasner’s valve. The middle meatus and middle turbinate are then inspected if they are not obstructed by any sinonasal pathology. The septum should be evaluated bilaterally for any evidence of prior surgery as well as deviation, perforation, and mucosal abnormalities. It is important to assess the involvement of the septum with tumor because this may affect reconstructive options.
Evaluation of skull base malignancies should include radiologic assessment with both computed tomography (CT) and magnetic resonance imaging (MRI). Imaging has an essential role in the assessment of the extent of disease and planning of management. Details about the tumor such as bony erosion, meningeal or brain invasion, or orbital invasion is critical in management planning.
In general, whereas CT is better for bony assessment and anatomic features, MRI is better at delineating soft tissue details. The preoperative radiographic evaluation is also critical for surgical mapping to enable safe and optimal outcomes.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here