Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Although soft tissue sarcomas are a heterogeneous group of neoplasms, their clinical evaluation and treatment follow common principles. This chapter focuses on the clinical evaluation, determinants of prognosis and outcome, and treatment of patients with soft tissue sarcoma.
Anatomically, the extremity is the most common anatomic site for soft tissue sarcoma, accounting for approximately half of all cases. Other important anatomic sites include the retroperitoneum, head and neck, and body wall. The site-specific distribution of histologic subtypes is outlined in Fig. 2.1 . Of note, the distribution of histologic subtypes depends greatly on the anatomic site; for example, in the extremities, undifferentiated pleomorphic sarcoma, liposarcoma, and synovial sarcoma are common. In contrast, in the retroperitoneum, synovial sarcoma and undifferentiated pleomorphic sarcoma are relatively uncommon; other histologic subtypes, particularly leiomyosarcoma and liposarcoma, predominate. The reasons for this regional variation in histologic subtype are not understood.
Most patients with suspected soft tissue neoplasms present with a painless mass, although pain is reported in one-third of cases. A delay in diagnosis is common; the most common misdiagnoses include posttraumatic or spontaneous hematoma and lipoma. A late diagnosis of patients with retroperitoneal sarcomas is common because of the large size of the retroperitoneal space, generally slow growth rate, and the tendency of sarcomas to gradually displace rather than to invade and compromise adjacent viscera. Therefore, retroperitoneal sarcomas can reach a considerable size before the diagnosis ( Fig. 2.2 ).

The physical examination should include an assessment of tumor size, relative mobility, and fixation. Patients with extremity soft tissue tumors should be evaluated for tumor-related neuropathy. An examination of regional lymph node basins should also be performed, with the understanding that nodal metastases are relatively uncommon, occurring in less than 15% of patients with extremity soft tissue sarcoma. Functional assessment of the involved region is of paramount importance, as well as complete neurologic and vascular examinations.
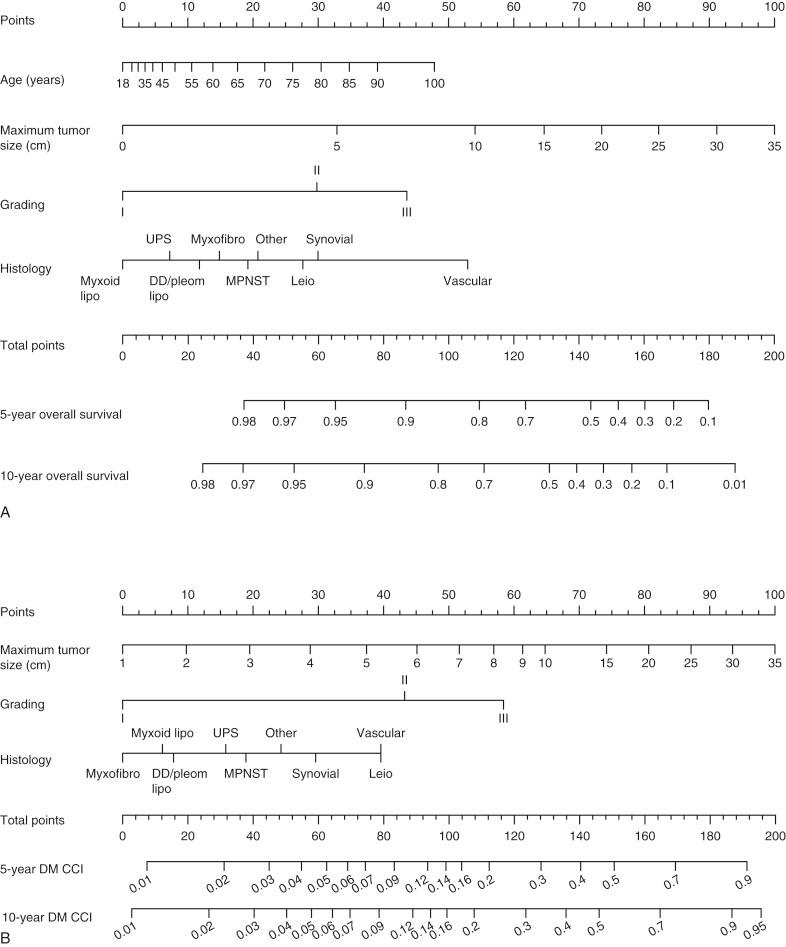
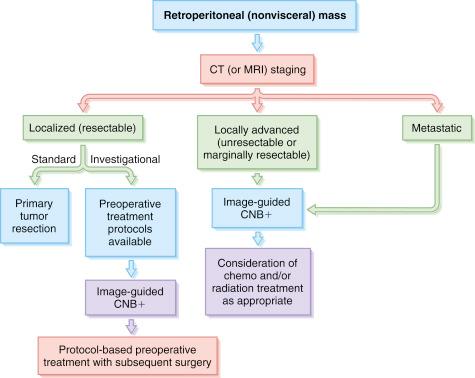
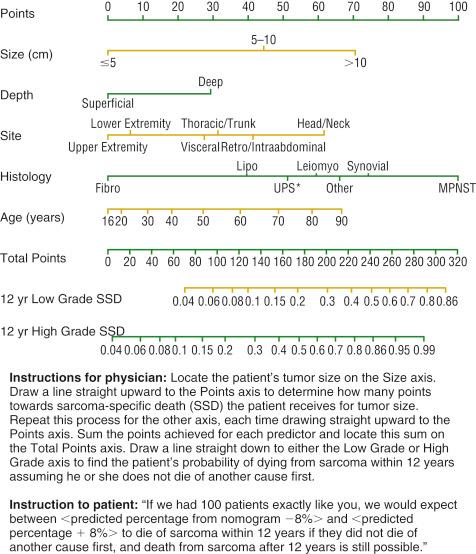
The pretreatment evaluation of the patient with a suspected soft tissue malignancy includes a biopsy diagnosis and radiologic staging to establish the extent of the disease. Practical nomograms and algorithms for the evaluation of patients with extremity and retroperitoneal soft tissue masses are outlined in Figs. 2.3 and 2.4 .
A pretreatment biopsy of the primary tumor is essential for most patients presenting with soft tissue masses. In general, any soft tissue mass that is enlarging or is greater than 5 cm should be considered for biopsy. For more anatomically constrained areas such as the forearm and hand, lesions less than 5 cm should be considered for biopsy. The preferred biopsy method is generally the least invasive technique that allows for a definitive histologic assessment, including an assessment of grade. Grade is particularly important to clinicians because it impacts treatment planning and treatment options. Grading of soft tissue sarcomas is discussed in Chapter 1 .
A percutaneous core-needle biopsy (CNB) provides satisfactory diagnostic tissue for the diagnosis of most soft tissue neoplasms. A CNB can be performed “blindly” in the clinic by clinicians without real-time radiologic control. However, many centers have moved to an image-guided CNB performed by interventional radiologists. Image-guided approaches allow for a biopsy from the areas of the tumor believed to be most likely to harbor viable tumor (i.e., avoiding centrally necrotic areas). The use of real-time imaging also minimizes the risks for biopsy-related vascular or adjacent organ injury. In many centers, image-guided biopsy also allows for real-time pathology quality control by having a pathologist immediately available in the biopsy suite to evaluate the quality of tissue retrieved and its probable suitability for a definitive diagnosis. Studies comparing a CNB to the traditional open surgical biopsy have demonstrated the safety, reliability, and cost-effectiveness of this approach. Additional issues related to the pathologic interpretation of core-needle biopsies are discussed in Chapter 5 .
Tumor recurrence in the needle track after a percutaneous CNB is extremely rare. Indeed, there are only case reports in the literature. However, these rare cases have led some physicians to advocate tattooing the biopsy site for subsequent excision. Most experienced sarcoma surgeons take a practical approach to this issue and perform an en bloc resection of the needle track and percutaneous entry point when feasible, but not if a resection of the biopsy track requires a second incision or substantial modification of the surgical plan. The low risk of needle track recurrence does not justify the added morbidity risk imposed by major alterations in the surgical plan.
An incisional biopsy is occasionally required to establish a definitive diagnosis for some soft tissue neoplasms. It has the advantage over CNB of providing more tissue for pathologic analysis and often additional tissue for tumor banking or research purposes. However, the morbidity associated with an incisional biopsy can be considerable, including the risks for anesthesia, bleeding, and wound-healing problems. Furthermore, if additional cores can be obtained, CNB may suffice to facilitate research. Given these considerations and its greater cost, incisional biopsy is generally a secondary technique best reserved for cases where a definitive diagnosis cannot be established by CNB.
An excisional biopsy may be appropriate for some patients who present with small, superficial neoplasms located on the extremities, well away from critical structures, or the superficial body wall, where the morbidity from this procedure is minimal. Although an excisional biopsy may allow for a single diagnostic and therapeutic procedure in some clinical settings, its main disadvantage is that the malignant potential of the neoplasm is unknown at biopsy, and informed decisions on surgical margins are not possible. This leaves the operating surgeon with the choice of narrow or nonexistent surgical margins, with generally lower risks for wound and functional morbidity, or deliberately wide margins, with generally greater risks for wound and functional morbidity. The oncologic appropriateness of the surgical margin cannot be assessed preoperatively and is difficult to assess with precision intraoperatively. This disadvantage makes an excisional biopsy appropriate for only a small subset of patients who have small, superficial neoplasms and for whom a reexcision is feasible, if the final diagnosis indicates a malignant lesion with compromised margins.
A percutaneous fine-needle aspiration (FNA) biopsy can also be used for cytologic assessment of some soft tissue neoplasms. Accurate FNA diagnosis requires the availability of an expert cytopathologist experienced in the diagnosis of soft tissue sarcomas by cytology. From a practical standpoint, most centers (even academic centers) will not have a cytopathologist with sufficient experience to allow for the use of FNA for routine diagnosis and classification of primary soft tissue neoplasms. Additionally, even with experience, a risk of diagnostic error remains because the histologic architecture is not captured with FNA. Given the frequent difficulty in histopathologic diagnosis and classification of soft tissue sarcoma, the major utility of FNA cytology in most centers is for the diagnosis of patients with suspected recurrent sarcoma. In this setting, there is already an established pathologic diagnosis, such that only confirmation of a recurrence with similar features is required.
The relative rarity of soft tissue sarcoma, the anatomic heterogeneity of these lesions, and the presence of more than 100 recognized histologic subtypes, of variable grades, have made it difficult to establish a functional system that can accurately stage all forms of this disease. The staging system (8th edition) of the American Joint Committee on Cancer (AJCC) and the Union for International Cancer Control (UICC; formerly International Union Against Cancer) is the most widely used staging system for soft tissue sarcoma (see Chapter 1 ). The system is designed for optimal staging of extremity tumors but is also applicable to the torso, head and neck, and retroperitoneal lesions; it should not be used for sarcomas of the gastrointestinal tract or other parenchymal organs.
Understanding the clinicopathologic factors that affect outcome is essential in formulating a treatment plan for the patient with soft tissue sarcoma. The three major clinicopathologic factors that establish the risk profile for a given patient are tumor size, histologic grade, and extent of disease (nodal or metastatic involvement), as reflected in the 8th edition of the AJCC staging system. The size of the tumor is now especially emphasized, with tumors grouped as 5 cm or less, greater than 5 cm, greater than 10 cm, and greater than 15 cm.
In addition to the previous factors, histologic subtype and margin status are also significant, but this information is not captured by the current staging system. Moreover, unlike other solid tumors, factors that predict local recurrence differ from those that predict distant metastasis and tumor-related death ( Table 2.1 ). In other words, patients with a constellation of adverse prognostic factors for local recurrence are not necessarily at increased risk for distant metastasis or tumor-related death, and vice versa. Therefore, clinicians and pathologists should be careful about using the terminology “high-risk disease” without qualification of the end point (i.e., local recurrence or overall survival) for which the patient is believed to be at increased risk.
| End Point | Adverse Prognostic Factor | Relative Risk (%) |
|---|---|---|
| Local recurrence | Fibrosarcoma | 2.5 |
| Local recurrence at presentation | 2.0 | |
| Microscopically positive margin | 1.8 | |
| Malignant peripheral nerve sheath tumor | 1.8 | |
| Age >50 yr | 1.6 | |
| Distant recurrence | High grade | 4.3 |
| Deep location | 2.5 | |
| Size 5.0–9.9 cm | 1.9 | |
| Leiomyosarcoma | 1.7 | |
| Nonliposarcoma histology | 1.6 | |
| Local recurrence at presentation | 1.5 | |
| Size ≥10.0 cm | 1.5 | |
| Disease-specific survival | High grade | 4.0 |
| Deep location | 2.8 | |
| Size ≥10.0 cm | 2.1 | |
| Malignant peripheral nerve sheath tumor | 1.9 | |
| Leiomyosarcoma | 1.9 | |
| Microscopically positive margin | 1.7 | |
| Lower-extremity site | 1.6 | |
| Local recurrence at presentation | 1.5 |
Surgeons should use the UICC resection (designated by the letter R ) classification system for integration of the operative findings and the final microscopic surgical margins. Under this system, an R0 resection is defined as a macroscopically complete sarcoma resection with microscopically negative surgical margins; an R1 resection is a macroscopically complete sarcoma resection with microscopically positive surgical margins, and an R2 resection is a macroscopically incomplete (i.e., with gross residual disease) sarcoma resection with microscopically positive surgical margins.
All therapeutic surgical procedures should be described in medical records using the R classification. To do so, surgeons must await the final pathology report, including margin assessment, and then integrate the observed operative findings, including the presence or absence of a residual gross tumor, with the final assessment of microscopic surgical margins. The operative report, discharge summary, and related medical records should describe the procedure using the R classification. As an example, a surgical procedure that involved a wide local resection of a left anterior thigh soft tissue leiomyosarcoma with satisfactory gross tumor margins, no operatively defined residual gross tumor, and negative microscopic surgical margins would be described as “R0 resection of left anterior thigh leiomyosarcoma.”
The type of microscopically positive surgical margins also appears important. For example, an R1 resection for a low-grade liposarcoma or an R1 after preoperative radiation treatment in which a microscopically positive margin is anticipated (and accepted) in order to preserve critical structures has a relatively low risk (<10%) for local recurrence. Furthermore, an anticipated positive margin on a critical structure does not increase local recurrence rates, as described in the Toronto Margin Context Classification (TMCC). Using the TMCC, positive margins are separated into planned close but positive at critical structures, positive after an unplanned surgical resection or reexcision, and inadvertent positive margins.
Patients undergoing “unplanned” excision followed by a reexcision with positive margins (i.e., R1 re-resection) or patients with unanticipated positive margins after primary resection are at increased risk for local recurrence, with rates approaching 30%. Therefore the specific clinical setting needs to be considered when interpreting the relative risk for local recurrence after an R1 resection.
Several prognostic nomograms have been developed for patients with soft tissue sarcomas in the extremity and retroperitoneum. The results have been used to construct and internally validate a nomogram to predict sarcoma-specific death ( Fig. 2.5 ). These nomograms match a patient’s prognostic score against those of previously treated patients with comparable tumor and clinical factors to estimate individual patient risk for sarcoma-related death.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here