Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Despite a large burden of disease, understanding of the clinical and genetic risk factors for the development and calcific valve disease remains incomplete, and no medical treatment exists to prevent disease progression.
In addition to the traditional atherosclerotic risk factors that have been associated with the development of calcific valve disease, emerging risk factors include lipoprotein(a), mineral metabolism (e.g. phosphate levels), and osteoporosis.
Genetic studies have identified NOTCH1 and LPA as robust disease-associated loci for calcific aortic valve disease. Additional loci have also been identified.
Mendelian randomization studies have provided evidence in support of circulating lipoprotein(a) and low-density lipoprotein as causal factors in calcific aortic valve disease and for triglycerides in mitral annular calcification, pointing to potential therapeutic targets in early disease.
Work to identify clinical and genetic risk factors and to provide evidence for causality for the development and progression of calcific valve disease is ongoing.
Calcific valve disease is the most common cause of valvular heart disease in the developed world. It affects predominantly the aortic valve leaflets, but also affects the mitral annulus and leads to progressive calcification and fibrosis, culminating in loss of leaflet elasticity, restriction of blood flow, and valvular stenosis. Despite the large burden of disease, understanding of the risks factors and the underlying causes of the initiation and progression of calcific valve disease remain incomplete. Nonetheless, with the aging of the population and the increasing numbers of individuals affected, research into the risk factors, including the role of genetics, has led to insights into this disease. It is hoped that these findings will pave the way for new approaches to prevent and treat aortic stenosis (AS) and other calcific valve disease.
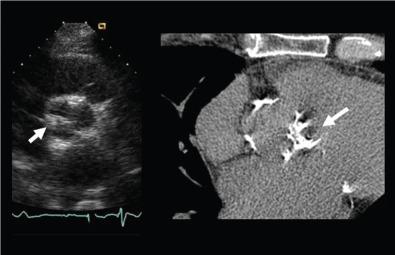
Calcific aortic valve disease (CAVD) represents a continuum of disease that begins with aortic sclerosis, which is asymptomatic but can be detected noninvasively by echocardiography or by cardiac computed tomography (CT) ( Fig. 4.1 ), and progresses to AS, which is characterized by obstruction to flow and the development of symptoms when stenosis becomes severe.
The natural history of CAVD consists of a long, clinically silent phase of valve calcification and hardening (i.e., sclerosis), which usually lasts at least a decade and heralds the clinical disease. Aortic valve sclerosis is exceedingly common, with a prevalence of 26% after 65 years of age, 40% after 75 years of age, and 75% after 85 years of age. Aortic valve sclerosis, which was long deemed a benign consequence of aging, is now known to confer a 40% increase in the risk of death and a 66% increase in the risk of cardiovascular death, independent of age and cardiovascular risk factors.
AS is the most common form of valve disease in the developed world, affecting more than 2.5 million individuals in the United States alone. Approximately 2% of the population older than 65 years of age have AS, a figure that increases to almost 7% of those older than 80 years of age. , It is estimated that the direct health care costs of advanced AS in the United States exceed 1 billion dollars per year. With the aging of the population, the prevalence of AS is projected to increase by more than twofold by 2040 and by threefold by 2060. , Although CAVD is poised to become a major contributor to health care expenditures, death, and disability, there are no medical treatments known to retard or arrest the progression of this disease.
Although CAVD has long been considered a degenerative condition of older age, research over the past 3 decades has demonstrated that the calcification and fibrosis, which characterizes this condition, are tightly regulated and likely occur in response to several risk factors that are shared with atherosclerosis. Although there is significant overlap between the early initiating lesion and certain shared risk factors, there are major differences in the underlying pathophysiology of these diseases, including a much more prominent mineralization phase in early disease and other histopathologic differences.
Among individuals undergoing aortic valve replacement for (noncongenital) AS, only 40% have significant coronary disease requiring bypass, suggesting unique pathologic processes in CAVD compared with coronary atherosclerosis. Lipid-lowering agents which have been remarkably effective for preventing atherosclerosis have also not demonstrated any benefit in randomized trials for CAVD further demonstrating that atherosclerosis and CAVD are related but separate diseases.
Older age is the most important risk factor for the development of CAVD and its major clinical manifestation, AS ( Table 4.1 ). The prevalence of CAVD (which includes sclerosis) based on echocardiography in the Cardiovascular Health Study (CHS) was determined to be 21% among individuals 65 to 74 years of age, 38% among those 75 to 84 years of age, and 52% among those older than 85 years.
| CAVD ANALYSES | |||
| Risk Factors | Cross-Sectional | Incident | Progression |
| Age | +++ | +++ | +++ |
| Male gender | ++/− | ++ | 0 |
| Height | ++ | ++ | 0 |
| BMI | ++ | ++ | 0 |
| Hypertension | ++ | ++ | 0 |
| Diabetes | +++ | +++ | 0 |
| Metabolic syndrome | ++ | ++ | + |
| Lipoprotein(a) | +++ | NA | ++ |
| Dyslipidemia | ++ | ++ | 0 |
| Smoking | ++ | ++ | + |
| Renal dysfunction | + | 0 | 0 |
| Inflammatory markers | + | 0 | 0 |
| Phosphorus | ++ | 0 | NA |
| Calcium levels | 0 | 0 | NA |
| Baseline calcium score | NA | NA | +++ |
In multivariable models, each 10-year increment in age was associated with an adjusted odds ratio of 2.18 (95% confidence interval [CI]: 2.15–2.20, P < 0.001) for CAVD. For AS, estimates from a meta-analysis suggest that approximately 12% of individuals older than 75 years of age have AS and that almost 4% have severe AS. Based on longitudinal data from the Multi-Ethnic Study of Atherosclerosis (MESA) using CT to measure valve calcium, age appears to influence progression of calcification and the development of new calcification in otherwise unaffected valves. Although age has been shown to be a key risk factor, it remains unclear whether age is a marker for the exposure time of other risk factors acting on the leaflets or whether aging itself predisposes to calcification and fibrosis.
Similar to the preponderance of coronary artery disease in men, a similar sex difference exists in CAVD. Male sex has been demonstrated to be a risk factor for CAVD in several studies. This may be related to the higher prevalence of bicuspid aortic valves in men, greater burden of cardiovascular risk factors, and lack of possible protective factors (e.g., estrogens). In multivariable analysis, male sex was shown to increase the odds of valve calcium by 1.56 (95% CI: 1.19–2.12, P = 0.005) in the Framingham Offspring Study cohorts, even after considering other possible risk factors. In the CHS, male sex was an important predictor of progression to AS (odds ratio [OR] = 3.05, 95% CI: 1.76–5.27, P < 0.001).
Limited data exist about whether race, ethnicity, or both, affect the prevalence of CAVD. In MESA, the baseline prevalence was 14% among white, 7% among Chinese, 11% among black, and 12% among Hispanic participants. However, none of these differences persisted after multivariable adjustment for other risk factors, suggesting no independent contribution from race or ethnic background.
A large study using electronic health records identified a much lower prevalence of AS among African-American patients due to CAVD or bicuspid aortic valve compared with white patients (adjusted OR = 0.41, 95% CI: 0.33–0.50, P < 0.001). Severe AS was also lower in African Americans (adjusted OR = 0.47, 95% CI: 0.36–0.61, P < 0.05). These results were independent of traditional risk factors. To demonstrate that the results were not due to bias (e.g., referral), the study authors showed no racial difference in the prevalence rates of mitral regurgitation. African Americans also demonstrated reduced progression to AS in the CHS (OR = 0.49, 95% CI: 0.25–0.95, P = 0.035). Whether these observations demonstrate true race-related differences due to genetic or other causes will require validation in future studies.
Cigarette smoking has been associated with CAVD in several studies. In the CHS, Stewart et al reported an adjusted odds ratio of 1.35 (95% CI: 1.1–1.7, P = 0.006) for current cigarette smoking. Similarly, in Framingham Offspring, cigarette smoking was associated with an adjusted odds ratio 1.22 for aortic valve calcium (AVC). (95% CI: 1.06–1.39, P = 0.005). In MESA, cigarette smoking was also a strong risk factor for incident aortic valve calcification (OR = 2.49, 95% CI: 1.49–4.15, P = 0.001).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here