Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The musculoskeletal reaction to trauma can result in a variety of bone, muscle, and ligamentous disruptions; sometimes fracture and ligamentous injuries occur concurrently. The general types of musculoskeletal trauma are fractures, dislocations, subluxations, sprains, strains, and diastases.
This chapter defines fractures and dislocations by sections. The first part contains general terms that are easily understood by the nonspecialist, followed by classic, descriptive, and eponymic terms by anatomic location. The second section is a brief outline of the AO (Arbeitsgemeinschaft für Osteosynthesefragen) system and Orthopaedic Trauma Association Registry System of fracture classification. The third section defines the many eponymic classification systems by grades, types, and mechanisms. The last section covers the types of dislocations, subluxations, strains and sprains, and sports-related injuries. Many new terms have been added to this edition.
Most patients with musculoskeletal injuries present to an emergency room in an acute stage and are treated by the emergency room physician until it is determined that an orthopaedic specialist may be required. Good communication is essential when relating the assessment of acute injuries. A brief and accurate description is vital to the evaluation and immediate treatment of the injured, and familiarity with the classification systems that follow will help in understanding the importance of accurate communication. For example, an open, midshaft, comminuted, femur fracture gives a brief description but accurately relates a lot. To achieve this degree of accuracy, learning the classifications is an important tool to the end user.
A uniform descriptive system also allows accurate coding of specific diagnostic entities. The bony detail is described by the following:
Open versus closed
Portion of bone involved
General appearance
Alignment of fragments and position and alignment
Interestingly, fractures have specific terminology that varies from time of occurrence to healing. Fractures may be named for an anatomic location, a person, or a place. They are further defined in terms of how they occurred or reason for the break. As fractures begin to heal, the degree and nature of healing are described.
Contributing factors, such as tumors, infections, and repeated stress, are included in the descriptive terminology. This is important for diagnostic coding. The management of fractures is also clarified. Closed management (closed reduction) means that treatment is in the form of a manipulation to achieve the reduction followed by the application of some form of external immobilization such as a cast, splint, or traction. Open management (open reduction) requires a surgical incision to approximate the fracture fragments into normal position. Often, some form of internal fixation ( osteosynthesis ) is performed with open management of fractures. A fracture of necessity requires surgical fixation for reduction.
Many advances have been made in the management of fractures such as immobilization from casting to bracing, or a combination of both. The term cast brace has been applied to a form of treatment in which the brace design is incorporated into temporary standard cast materials. This method allows for limited motion in the brace during the early healing stage with controlled fracture movement. Its use has shown greater callus formation around the fracture site, improved ligamentous healing, and earlier recovery of joint mobility and muscle control.
Another method of fracture management employs magnetic and electrical bone stimulators, some with surface electrodes externally applied to a fracture site. Electromagnetic models use different modalities to effect an electric field that theoretically will induce piezoelectric microcurrents that help stimulate bone formation. Ultrasonic bone stimulation is also used and has been found to be more effective than previously thought.
An option of traumatic fracture management is the use of external fixation devices and frames, also called fixateurs or fixators. Treatment methods and external skeletal fixation devices are discussed in Chapter 8 .
diastasis: may be one of two types: (1) disjointing of two bones parallel to one another, for example, radius and ulna, tibia and fibula complex; or (2) rupture of any solid joint, as in a diastasis of the symphysis pubis. Such an injury tends to occur in association with other fractures and is then called fracture-diastasis.
dislocation: (L., luxatio ): complete displacement of bone from its normal position at the joint surface, disrupting the articulation of two or three bones at that junction and altering the alignment. This displacement affects the joint capsule and surrounding tissues (muscles, ligaments). Dislocation ( luxation ) may be traumatic (direct blow or injury), congenital (developmental defect), or pathologic (as in muscle imbalance, ligamentous tearing, rheumatoid arthritis, or infection).
fracture: (L., fractura ): structural break in the continuity of a bone, epiphyseal plate, or cartilaginous joint surface, usually traumatic with disruption of osseous tissue.
fracture-dislocation: fracture of a bone that involves a dislocation of an adjacent articulation of that bone. Example: Shoulder fracture dislocation in which there is a proximal periarticular humerus fracture with an associated dislocation (not subluxation) of the humeral head.
sprain-ligament rupture: (L., luxatio imperfecta ): stretching or tearing of ligaments (fibrous bands that bind bones together at a joint), varying in degrees from being partially torn (stretched) to being completely torn (ruptured), with the continuity of the ligament remaining intact. After a sprain, the fibrous capsule that encloses the joint may become inflamed, swollen, discolored, and extremely painful. Involuntary muscle spasm, and sometimes an associated fracture, may occur. Rest, elevation, and a restrictive bandage, splint, or cast are methods of treating these injuries until properly healed. When a ligament or tendon has been torn completely, dislocation may also occur. Surgical repair may be required in some cases.
strain: stretching or tearing of a muscle or its tendon (fibrous cord that attaches the muscle to the bone it moves) may result in bleeding into the damaged muscle area, which causes pain, swelling, stiffness, muscle spasm, and, subsequently, a bruise. A strain can be serious because muscle damage (scar tissue) may cause muscle shortening. With rest, strains will subside in 2–3 days, but symptoms may persist for months.
subluxation: incomplete or partial dislocation in that one bone forming a joint is displaced only partially from its normal position; also, a chronic tendency of a bone to become partially dislocated, in contrast to an outright dislocation, for example, shoulder, patella, and hip.
( Fig. 1-1 )
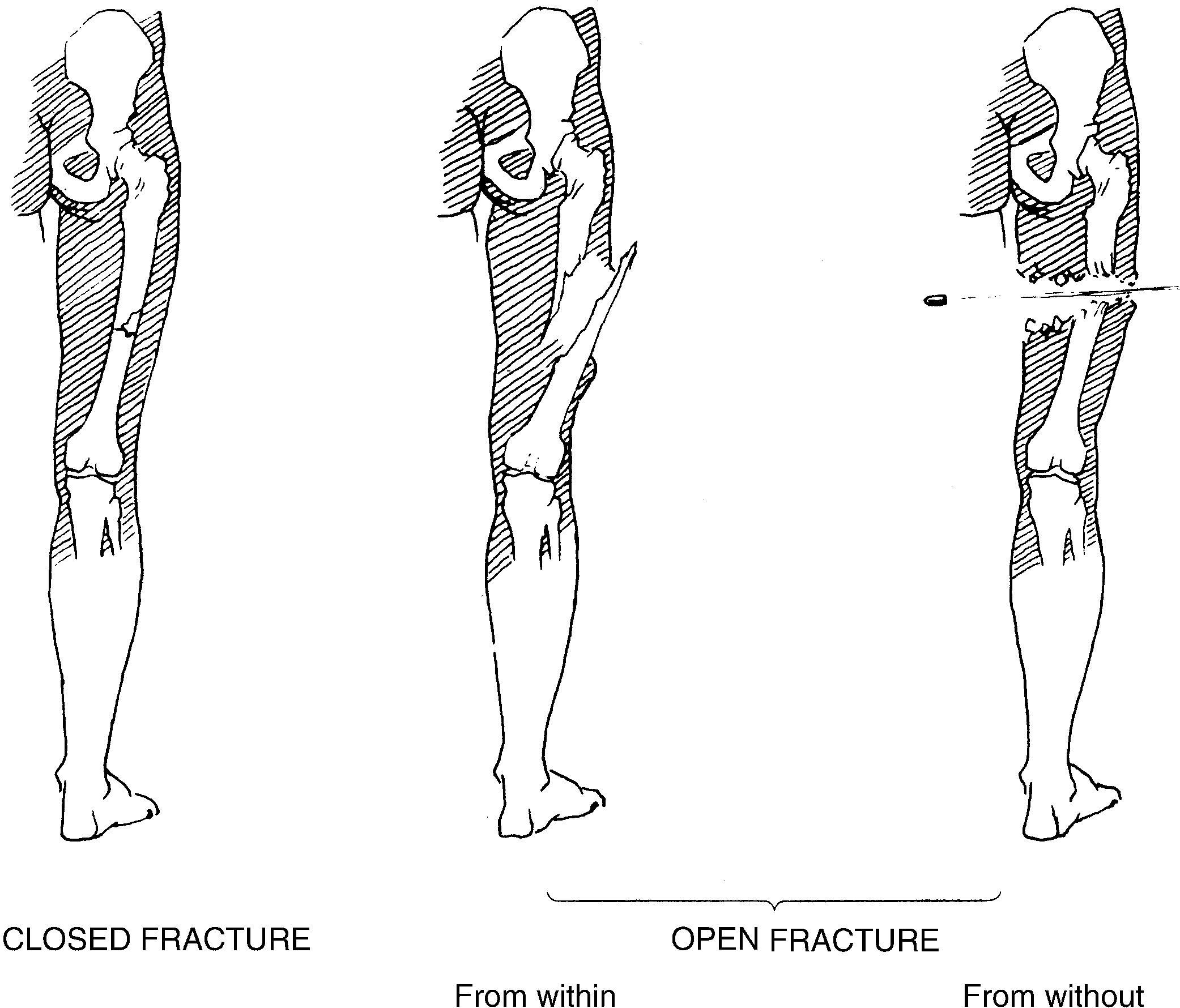
closed f.: does not produce an open wound of the skin but does result in loss of continuity of bone subcutaneously; formerly called simple f.
open f.: one of the fragments has broken through the skin, and there is loss of continuity of bone internally; formerly called compound f.
The portion of bone involved or the point of reference of a fracture may be referred to as the distal third ( D/3 ), the middle third ( M/3 ), and the proximal third ( P/3 ). Middle third fractures are commonly called midshaft fractures. For specific anatomic locations, the following terms are commonly used.
apophyseal f.: avulsion of or fracture through an apophysis (bony prominence) where there is strong tendinous attachment.
articular f.: involves a joint surface; also called joint f. and intraarticular f.
cleavage f.: fracture through cartilage and bone that may be a large fragment such as a tibial plateau or avulsion of a small fragment of bone such as the capitellum.
condylar f.: involves any round end of a hinge joint (see sections on femoral and distal humeral fractures).
cortical f.: involves cortex of bone.
direct f.: results at specific point of injury and is due to the injury itself.
extracapsular f.: occurs near but outside the capsule of a joint, especially the hip; also called extraarticular.
intracapsular f.: occurs within the capsule of a joint; also called intraarticular.
nonphyseal f.: any childhood fracture that does not involve a growth plate.
periarticular f.: occurs near but not involving a joint.
transchondral f.: fracture through cartilage, which may not be apparent unless there is a bone fracture line into the joint; not to be confused with transcondylar f.
transcondylar f.: occurs transversely between the condyles of the elbow. This term is also used in fractures of the femur and bones with condyles; also called diacondylar f.
tuft f.: involves the distal phalanx (tuft) of any digit.
( Fig. 1-2 )
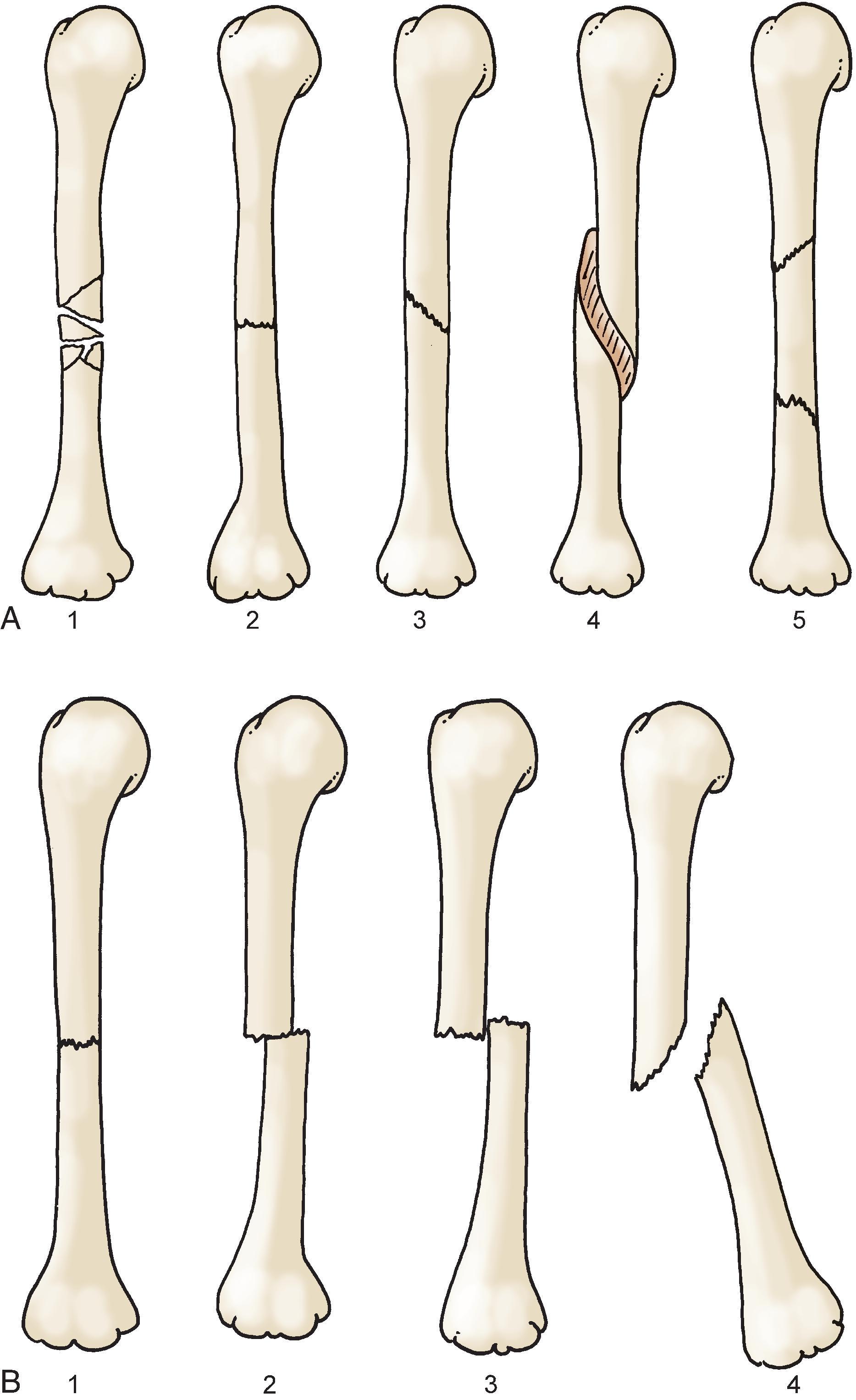
avulsion f.: tearing away of a part; a fragmentation of bone where the pull of a strong ligamentous or tendinous attachment tends to forcibly pull the fragment away from the rest of the bone. The fragment is usually at the articular surface.
burst f.: multiple fragments, usually at the end of a bone; f. of the first cervical vertebra or the body of the any vertebra where there is typically displacement of bone into the spinal canal.
butterfly f.: a bone fragment shaped like a butterfly in which the fragment is completely detached from the proximal and distal segments of the bone; usually involves high-energy force delivered to the bone.
chip f.: a small fragment, usually at the articular margin of a joint.
comminuted f.: more than two fragments; described by degree and quantity of pieces; any third fragment of bone will constitute some element of comminution. A butterfly segment is a type of comminution. Typically, comminution is used to describe multiple fracture fragments (highly comminuted) versus only an additional fragment or two (minimally comminuted); also called splintered fracture or multifragmentary fracture.
complete f.: the bone is completely broken through both cortices.
compression f.: crumbling or smashing of cancellous bone by forces acting parallel to the long axis of bone; applied particularly to vertebral body fractures.
depressed f.: typically an intraarticular depression of fragments, but may also be applied to depressed skull fractures.
double f.: segmental f. of a bone in two places.
epiphyseal f.: involves the portion of the bone that on the joint surface side of of the physis, which is the growth plate.
fissure f.: crack in one cortex (surface) only of a long bone.
fragility fracture: fracture that occurs with minimal trauma; caused by osteoporosis.
greenstick f.: in children, incomplete, angulated fracture with a partial break; also called incomplete f., interperiosteal f., hickory-stick f., and willow f.
hairline f.: nondisplaced fracture line (crack) in the cortex of bone.
impacted f.: fragments are compressed by force of original injury, driving one fragment of bone into adjacent bone.
incomplete f.: cortices of bone are buckled or cracked, but continuity is not destroyed; the cortex is broken on one side and only bent on the other. Microscopically, the fracture is present on bent side, and resorption and callus will occur on this side as well; types are greenstick f., torus f.
infraction f.: small radiolucent line seen in pathologic fractures, most commonly resulting from metabolic problems.
insufficiency f.: a fracture that occurs because bone is made insufficient as a result of osteoporosis or a metabolic process.
inverted Y f: typically used for a tibial medial and lateral condyle fracture with central fracture line entering joint. Term has also be applied to other Y shaped fracture.
linear f.: lengthwise fracture of bone straight line fracture; implies that there is no displacement.
multiple f.: two or more separate lines of fracture in the same bone.
oblique f.: slanted fracture of the shaft on long axis of bone.
occult f.: hidden fracture (undetectable on a radiograph), generally occurring in areas of the ribs, tibia, metatarsals, and navicular. Alternatively, difficult to detect fractures occurring in severe osteoporosis such as hip, pelvis, or vertebrae.
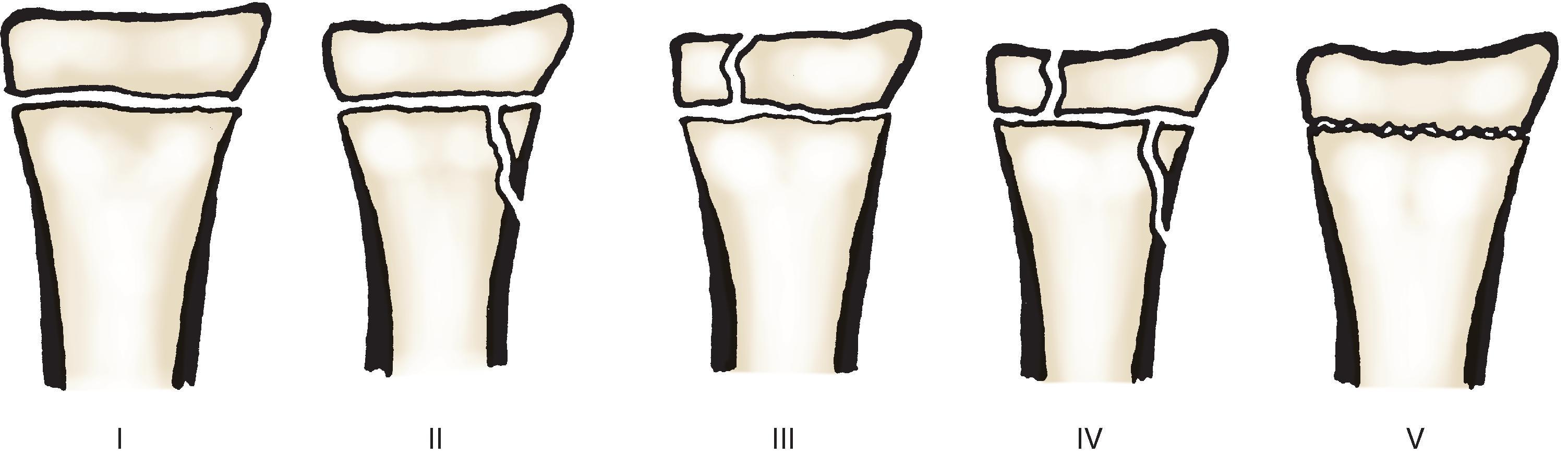
physeal f: one that involves the cartilaginous growth plate of a bone; also called epiphyseal slip f., Salter f., and Salter-Harris f. ( Fig. 1-3 ).
plastic bowing f.: curved deformity of a tubular bone without gross fracture; also called bowing f., greenstick f.
pathologic f.: fracture of bone weakened by disease such as tumors, metabolic disease, or severe osteoporosis; Also called secondary f.
segmental f.: several large fractures in the same bone shaft where the two principal fragments are not adjacent.
spiral f.: fracture line is spiral shaped and multiplanar, usually on shaft of long bones where the mechanism of injury is usually torsion.
stellate f.: numerous fissures radiate from central point of injury, usually a vertebral body.
subperiosteal f.: bone but not its periosteal tube is broken; uncommon; usually the result of a direct blow.
torus f.: usually noticed in children; a stable, often incomplete f. in which one distal cortical surface appears to be wrinkled by compression forces, and the opposite cortex may or may not be infracted by tension forces.
transverse f.: line of fracture across the shaft at right angles to the long axis of a bone.
unstable f.: fracture where it is difficult to maintain reduction and most often requires operative intervention because of the likelihood of recurrent deformity despite manipulation.
( Fig. 1-4 )
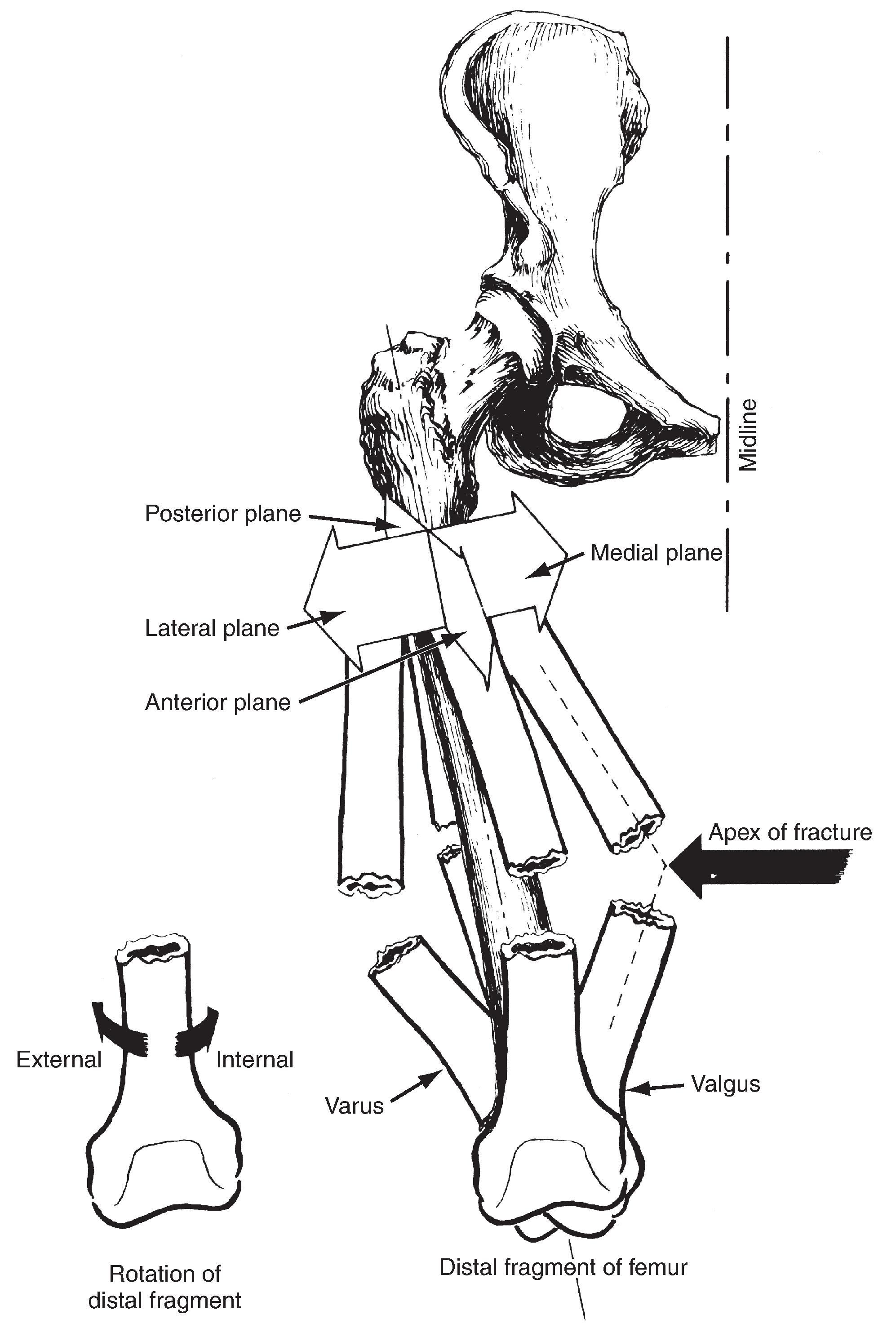
The position of a fragment refers to any displacement of one bone fragment in reference to the next. Displacement, should it exist, can be in any plane. Alignment refers to rotatory or angular deviation of the distal fragment in relation to the proximal fragment. For example:
angulation: typically described by the apex of the deformity. An apex anterior angulation means that the “point” or apex of the fracture is pointed anteriorly. This could also be described as antecurvatum or procurvatum. An apex posterior angulation is therefore recurvatum.
bayonet position: the fragments touch and overlap, but there is good alignment. Internal and external rotation can also be stated in degrees.
bow: the two fragments form an angle where the apex is sometimes described as an anterior or posterior bow.
The descriptive radiographic interpretations of fractures are defined as follows. The angulation of the fracture is designated by the direction of the apex of the fracture points. Fragments themselves are designated as proximal and distal displacement, which is the amount of offset of the proximal to distal fragment as seen in an anterior to posterior or medial to lateral direction.
When broken ends of the principal fragments are touching on end, they are said to be in apposition. Accuracy or degree of apposition is defined in percentages, such as 50%, indicating at least one radiographic view shows 50% contact and other views may appear to be more.
The site may be diaphyseal, metaphyseal, or epiphyseal portions of a specific bone or may be intraarticular. Extent may be described as complete, incomplete, cracked, hairline, buckled, or greenstick. The configuration may be transverse, oblique, or spiral, and is referred to as comminuted when more than two fragments are present. The fracture fragments may be undisplaced or displaced.
Thus a fracture is described radiographically by its site, bone name, extent, configuration, relationship of fragments to each other and to the external environment (open or closed), and the presence or absence of complications.
anatomic neck f.: occurs in the area of tendinous attachments, the true neck of humeral metaphysis.
Bankart f.: detachment of a small piece of bone from the anteroinferior rim of the glenoid; seen with anterior shoulder dislocation, usually called a Bankart fragment. The cartilage rim may detach without a fracture, and this is called a Bankart lesion.
coracoid f.: fracture of coracoid process of scapula.
greater tuberosity f.: fracture of bone prominence and attachment of supraspinatus.
lesser tuberosity f.: fracture of bone prominence for attachment of subscapularis.
Hill-Sachs f.: moderate compression f. or indentation f. of the humeral head usually seen after an anterior dislocation of the shoulder. In a classic Hill-Sachs lesion the anterior glenoid causes a dent or defect of the region near the greater tuberosity. A reverse Hill-Sachs is seen with posterior dislocations, and where the defect is in the region of the lesser tuberosity; also called Hermodsson f.
surgical neck f.: occurs in area below the anatomic neck of the humerus.
boxer’s elbow: chip f. at the tip of the olecranon caused by a fast extension of the elbow in a missed jab (punch).
condylar f.: occurs at the medial or lateral articular process of the humerus at the elbow.
epicondylar f.: occurs through one of the two epicondyles, medial or lateral.
Hahn-Steinthal f.: complete capitellar fracture with little or no extension into the lateral trochlea typically associated with anterior displacement.
Holstein-Lewis f.: involves the humerus at the junction of the middle and distal thirds; associated with radial nerve paralysis because of nerve proximity to posterior septum and bone.
Kocher f.: semilunar chip f. of capitellum with displacement into joint.
Kocher-Lorenz f.: minimal osteochondral capitellar fracture typically associated with posterior displacement.
Laugier f.: involves the trochlea of the humerus.
Malgaigne f.: extension mechanism supracondylar f. of humerus; name also applied to a vertically dissociated fracture dislocation of the pelvis and a proximal fibular fracture.
Posada f.: anteriorly angulated fracture of distal humerus associated with posterior dislocation of radius and ulna.
sideswipe f.: comminuted fracture of distal humerus and sometimes radius and ulna caused by direct blow against elbow.
supracondylar f.: occurs through the distal metaphysis of the humerus or femur.
T f.: intercondylar fracture shaped like a T.
Y f.: intercondylar fracture shaped like a Y.
Barton f.: an intraarticular fracture of the dorsal articular rim of the distal radius resulting in volar displacement radial carpal fragment.
chauffeur’s f.: oblique fracture of the radial styloid caused by a twisting- or snapping-type injury; also called backfire f., Hutchinson f., and lorry driver’s f.
chisel f.: incomplete, usually involving medial head of radius, with fracture line extending distally.
Colles f.: named prior to x-ray technology; implies a fracture of the distal radius, either articular or nonarticular, with dorsal angulation of the distal fragment producing a silver fork deformity; generally associated with a fracture of the ulnar styloid.
corner f.: a small bucket-handle-appearing fracture in the distal metaphyseal corner in a young child, often associated with child abuse.
de Quervain f.: combination of a wrist scaphoid fracture with volar dislocation of scaphoid fragment and lunate.
dye-punch f.: an intraarticular fracture of the ulnar (volar) portion of the distal radius, usually caused by direct impaction of the lunate onto the lunate fossa of the distal radius.
Essex-Lopresti f.: a comminuted radial head fracture with an injury to the distal radioulnar joint caused by disruption of the interosseous membrane, which can cause a proximal migration of the radius if the radial head is excised secondarily.
Galeazzi f.: typically a displaced fracture of the distal third or quarter of the radius with disruption of the distal radioulnar joint; called fracture of necessity because surgical fixation is required for reduction; also called a reverse Monteggia f., Dupuytren f., or Piedmont f.
Kocher f.: fracture of capitellum of distal humerus with possible displacement of fragment into joint.
Laugier f.: isolated fracture of the trochlea of the humerus at the elbow.
lead pipe f: typically in the forearm, a combination of greenstick fracture and torus fracture in the immature skeleton. Such fractures do not penetrate the entire shaft of the bone and have the appearance of a slightly bent lead pipe.
Lenteneur’s f.: a distal radial fracture of the palmar rim, similar to Smith’s type II fracture.
Monteggia f.: isolated fracture of proximal third of ulna, with posterior or anterior dislocation of radial head allowing angulation and overriding of ulnar fragments.
Moore f.: like a Colles f.; specifically, fracture of distal radius with dorsal displacement of ulnar styloid and impingement under annular ligament.
Mouchet f.: involves humeral capitellum.
nightstick f.: undisplaced fracture of the ulnar shaft caused by a direct blow.
Piedmont f.: oblique f. usually at the proximal portion of distal third of the radius; obliquity runs from proximal ulnar to distal radial aspect, allowing distal fragments to be pulled into the ulna by the pronator quadratus muscle; fracture of necessity requiring operative management.
radial head f.: involves the most proximal part of the radius, a dish-shaped portion of bone.
radial styloid f.: involves distal radial tip of radius.
reverse Barton f.: dorsal displacement of carpus on radius, with associated fracture of dorsal articular surface of radius. The mechanism and appearance of this fracture are similar to those of a Colles f.
Skillern f.: open f. of the volar or dorsal rim of the distal radius, usually resulting in subluxation or dislocation of the radial carpal joint line associated with greenstick f. of distal ulna.
Smith f.: fracture of the distal radius in which the distal fragment is displaced volarly; also called reverse Colles f. This fracture was defined before the advent of radiography, and, classically, there are three types:
Nonarticular
Intraarticular; also called volar Barton f.
Oblique nonarticular fracture near the joint line
Bennett f.: fracture of the base of the thumb metacarpal, usually leaving a volar ulnar fragment attached to a retaining ligament with radial subluxation of the metacarpal.
crush f.: term used for comminuted impaction of any bone, but for the finger is a distal phalanx fracture resulting from a crush injury.
mallet f.: avulsion f. of the extensor tendon from the dorsal base of the distal phalanx of any digit that includes insertion of extensor apparatus, thus allowing distal segment to drop into flexion; also called baseball finger, drop finger, and mallet finger deformity.
Rolando f.: an intraarticular comminuted fracture of the base of the thumb metacarpal resulting in a Y- or T-shaped fracture at the base of the metacarpal.
unciform f.: fracture of the hook of the hamate, usually caused by direct trauma that may or may not be associated with ulnar neuropathy.
Wilson f.: involves the proximal volar portion of the middle phalanx because of strong attachment of volar plate.
burst fracture: Involved a compressive fracture of the vertebra that can disrupt stability and cause retropulsion of bone into the spinal canal resulting in paralysis. Depending on severity and location, they can be treated by bracing or require extensive surgical intervention.
Chance f.: involves vertebra, with horizontal splitting of spinous process and neural arch with disruption through vertebral body; an unstable fracture.
clay shoveler’s f.: involves spinous process(es) C-6, C-7, T-1, T-2, or T-3.
compression fracture: most frequently a “wedge-shaped” compression fracture seen in older adults. They contribute to deformity of a “hunched” back commonly seen in older adults and are mostly painful and do not risk neurologic compromise. They may be just as disabling and commonly caused by low-energy mechanisms (jolt or fall) with bone insufficiency resulting from osteoporosis.
hangman’s f.: posterior element (pedicles) fracture with anterior subluxation of the cervical neck of C-2 on C-3.
Jefferson f.: bursting f. of the ring of the first cervical vertebra (atlas).
posterior element f.: broad term used to describe any fracture of the spinous process, lamina, facets, pars interarticularis, or pedicle.
seatbelt f.: thoracic or lumbar spine fracture resulting from tensile stress that occurs on spine with forward motion of thorax with abdominal or thoracic restraint resulting in bony or ligament disruption. If only the bone is involved, the injury is called a Chance f.
sentinel f.: a cervical spine fracture characterized by fractures through the lamina on either side of the spinous process. A sentinel of potential instability.
slice f.: an unstable lumbar spine fracture caused by a flexion rotation injury that results in a fracture in the upper body of the lower vertebra and a dislocation of the articular process of the upper vertebra.
spondyloptosis: dislocation of one vertebra from another without any bone fracture.
teardrop f.: exists in two forms: (1) an isolated anteroinferior fracture of the cervical spine (unstable); or (2) a three-part, two-plane fracture of an anteroinferior corner of the vertebral body (the teardrop), a sagittal vertebral body, and the posterior neural arch.
vertebra plana f.: wafer-thin compression f. of a vertebral body resulting from an intrinsic pathologic condition of the bone.
wedge f.: anterior compression f. of any vertebra; most common in the dorsal thoracic spine.
acetabular fracture: Any fracture that involves the acetabulum (socket).
basal neck f.: involves base of femoral neck at junction of trochanteric region basicervical.
bucket-handle f.: vertical shear fracture of anterior pubis and opposite ilium.
central f.: acetabular fracture, centrally displaced through inner wall of pelvis.
dashboard f.: posterior lip of acetabulum chips when femoral head is driven against it; often caused by a sudden jolt when knee hits dashboard.
dome f.: acetabular fracture involving weight-bearing surface of the acetabulum. This term can also be applied to a fracture of the superior surface of the talus.
Duverney f.: involves ilium just below the anterosuperior spine.
extracapsular f.: occurs outside of joint capsule of humerus or femur.
femoral neck f.: transcervical fracture through midportion of femoral neck.
hip f.: implies a fracture of the femoral neck or intertrochanteric area.
intertrochanteric f.: the principal plane of the fracture disrupts the intertrochanteric line.
intracapsular f.: commonly used for high femoral neck fractures, but is also used for any fracture within a joint capsule.
Malgaigne f.: occurs through wing of the ilium or sacrum with associated fractures through the ipsilateral pubic rami, allowing upward displacement of hemipelvis; often associated with internal injuries.
open book f: pelvis fracture with symphysis separation and disruption of the sacral pelvic ligaments to give appearance of opening a book.
pertrochanteric f.: involves proximal femur where the fracture line passes through both the lesser and greater trochanters.
ring f.: involves at least two parts of pelvic circumference.
shaft f.: occurs between subtrochanteric and supracondylar area.
sprinter’s f.: involves anterosuperior or anteroinferior spine of ilium, with a fragment of bone being pulled forcibly by sudden muscular pull.
straddle f.: double f. or dislocation of the pubis usually caused by a straddling mechanism, for example, falling onto a rail with the point of contact between the legs.
subcapital f.: femoral fracture at head-neck junction.
subtrochanteric f.: transverse f. of femur just below lesser trochanter.
Waddell triad: femoral fracture associated with head and thorax injuries.
Walther f.: transverse ischioacetabular f. where the fracture line passes from ischial spine to acetabular cavity to ischiopubic junction.
bumper f.: involves the tibia or femur and is caused by a direct blow in area of the tibial tuberosity; commonly caused by a car bumper accident; may be bilateral.
cartwheel f.: fracture of the distal femoral epiphysis in a child, so named by mechanism of a leg caught in the spokes of a cartwheel; also called wagon wheel f .
clipping injury f.: fracture through growth plate of distal femur or proximal tibia caused by a strike from the lateral side of the knee when the foot is planted.
Hoffa f.: coronal fracture of medial femoral condyle.
patellar f.: involves kneecap.
pillion f.: T-shaped fracture of distal femur with displacement of the condyles posteriorly to femoral shaft, caused by severe blow to knee; so named for pillion back seat position of a motorcycle rider who sustains this injury. Not to be confused with pilon fracture, which is due to a vertical impaction of the distal tibia into the talus.
Segond f.: small avulsion f. of superolateral tibia caused by tension on the lateral capsule or ligament; usually associated with other severe ligamentous injuries leading to anterolateral knee instability; also called lateral capsule sign.
sleeve f.: involves a small chip of bone from the superior or inferior portion of the patella associated with loss of integrity of quadriceps extensor mechanism.
Stieda f.: avulsion f. of origin of medial collateral ligament on medial femoral condyle.
supracondylar f.: involves the distal shaft of bone above condyles of femur or humerus.
tibial plateau f.: involves proximal tibial articular surface.
toddler f.: nondisplaced fracture of the tibia seen in toddlers beginning to walk.
Trélat fracture: type III fracture crossing the physis of the medial femoral condyle.
Y and T f.: combined supracondylar and intercondylar f. of the distal femur.
ankle mortise diastasis: separation of tibia and fibula at ankle; often associated with a fracture or dislocation.
aviator’s astragalus: denotes a talar neck fracture caused by sudden impaction of foot into ankle; may be associated with other fractures about the foot and ankle.
bimalleolar ankle f.: in which both the medial malleolus and distal fibula are fractured; also called Pott f.
bimalleolar equivalent: a fracture of the medial or lateral malleolus with ligamentous damage on the opposite side of an ankle.
boot-top f.: involves transverse, distal third of tibia, occurring at boot top of old-style ski boot; also called skier’s injury.
Bosworth f.: fracture-dislocation of the ankle, with oblique fracture of the distal fibula and displacement of the proximal fibular fragment out of fibular groove to a place posterior and medial to the posterolateral ridge of the tibia.
bunkbed f.: intraarticular f. of the base of the first metatarsal in children.
Cedell f.: fracture of the posterior medial process of the talus; may be associated with tarsal tunnel syndrome.
Chaput f.: involves the anterior tubercle of distal tibia because of strong attachment of anterior tibiofibular ligament.
Conrad-Bugg trapping: incarceration of soft tissue, usually the posterior tibial tendon, between fragments of an ankle fracture. This produces an injury that usually is reduced by open methods.
Cotton f.: partial forward dislocation of the tibia to produce a fracture of the posterior inferior margin of the tibia, sometimes called the posterior malleolus. This is most commonly associated with a fibular fracture.
Descot f.: involves the posterior lip of tibia.
dome f.: involves the superior articular surface of talus or the weight-bearing portion of the acetabulum.
Dupuytren f.: spiral f. of the distal end of fibula; associated with ankle diastasis.
Gosselin f.: V-shaped fracture of the distal tibia into the tibiotalar joint.
Henderson f.: trimalleolar fracture of the ankle.
Jones f.: fracture of the base of the fifth metatarsal such that the fracture line extends from lateral to medial cortex in the shaft portion of the apophyseal tip. This term has been misapplied to fractures in the proximal apophyseal portion.
Kohler f.: involves the navicular and is associated with avascular necrosis; seen in children.
Lisfranc f.: usually a fracture-dislocation, with displacement of the proximal metatarsals most commonly the first and second.
Maisonneuve f.: spiral f. of proximal end of fibula, near the neck, associated with a tear of the anterior tibiofibular ligament and the potential for ankle diastasis associated with a tear of the anterior tibiofibular ligament and a medial malleolus fracture or deltoid ligament disruption.
march f.: stress f. of metatarsal caused by excessive marching; also called fatigue f.
midnight f.: open, oblique fracture of proximal phalanx of little toe caused by stubbing the toe on a solid object.
Montercaux f.: fracture of fibular neck with associated diastasis of ankle mortise.
paratrooper f.: involves posterior articular margin of tibia or lateral malleolus.
Pott f.: spiral oblique f. of distal fibula with associated rupture of the deltoid ligament; avulsion of the medial malleolus and lateral displacement of foot on tibia.
plafond f.: any fracture that involves the surface of the tibia that comes in contact with the dome of the talus.
Shepherd f.: involves posterior talus with sheared off piece of bone and, in some instances, a separate piece of bone (os trigonum).
Tillaux Kleiger f.: involves distal lateral tibia, vertically extending into the joint; sometimes associated with diastasis and other fractures about the ankle.
tongue f.: involves the posterosuperior portion of calcaneus.
trimalleolar f.: fracture of medial, lateral, and posterior malleolus.
triplane f.: involves the ankle in three planes: coronally through the posterior tibial metaphysis, transversely through the growth plate, and sagittally through the distal tibial epiphysis.
Volkmann f.: involves a triangular portion of the posterior lateral tibia into the joint, leaving a triangular bone fragment sometimes called Volkmann’s triangle.
Wagstaffe f.: separation of a distal anterior fragment of the fibula, that is, the portion of attachment of the anterior tibiofibular ligament; also called Le Fort f.
Aside from a single obvious traumatic event, other factors contribute to fractures.
dyscrasic f.: results from weakening of bone by a disease process.
endocrine f.: occurs in bone weakened by an endocrine disorder.
fatigue f.: spontaneous fracture in healthy bone resulting from fatigue or stress produced by excessive physical activity in a short period; seen in fibulas and tibias of young long-distance runners, the hips and heels of young military recruits, and in the metatarsals; also called stress f., march f.
hoop stress f.: involves the medial or anteromedial femoral neck and occurs during broaching of the femoral canal for a prosthesis or during the actual impaction of the prosthesis.
inflammatory f.: occurs in association with inflammation secondary to an infection, such as syphilis.
insufficiency f.: stress f. that occurs in bone because of its diminished volume (i.e., osteopenia).
neoplastic f.: a form of pathologic f. Presence of a tumor in bone, whether originating in the bone or metastatic from elsewhere, causes sufficient weakening to allow it to fracture spontaneously or with less trauma than it would normally take to break a healthy bone.
neuropathic f.: fracture caused by overuse trauma to bone that occurs because of lack of pain perception.
pathologic f.: occurs with or without trauma where bone has been weakened by a local or systemic process. The most common causes are a tumor (benign or malignant), local infection, or bone cyst. This term is less widely applied to congenital disorders such as osteogenesis imperfecta, osteopetrosis, and neurofibromatosis. The term is applied more to congenital or acquired disorders such as osteomalacia, rickets, Paget disease, scurvy, and osteoporosis.
pseudofracture: radiographic finding of a line through bone that is due to abnormal mineralization that occurs in osteomalacia.
spontaneous f.: fracture that occurs without abnormal force. Usually caused by a pathologic condition of the bone or the cumulative overuse of a bone where the response to repeated stress is sufficient for a fracture to occur.
stress f.: crack in bone from overexertion placed on bone structure of limb or metatarsals and from pull of muscle on bone. Not noticeable on initial radiograph but is on later radiographs when callus formation has taken place at the site. A bone scan or magnetic resonance imaging will show the fracture; also called march f., fatigue f. More recently, the term stress reaction to bone has been used because fracture lines often do not appear and because the term more accurately describes the condition.
tension f.: bone fails at right angle to the direction of a tension force resulting in a transverse fracture.
The quality of bone healing is stated in terms of the solidarity of adhesiveness of the bone fragments. As most fractures heal, a surrounding sleeve of bone, or callus, is formed. This new bone formation is composed of cartilage, bone, blood vessels, and fibrous tissue and is often referred to in discussing bone healing. If the bone is completely healed, the term healed or united is used. When based on radiographic criteria, fracture union is defined as radiographic evidence of callus formation bridging three out of four cortices. Anything less is considered a state of healing, unless there is a failure of progression of healing with expectation of no further healing. This is then considered a nonunion.
The absence of complete union is called ununited, but this term by some users implies an expectation of failure to unite. In delayed union the speed of callus formation (fracture healing) is slower than anticipated, but this does not imply expectancy of either total healing or nonunion. A pseudoarthrosis is the formation of a jointlike structure at the old fracture site and is a type of nonunion. It consists of fibrocartilaginous tissue and a synovial fluid sac. If a bone unites in an abnormal position or alignment, the term malunion is used. If two bones parallel to one another unite by osseous tissue, such as the tibia/fibula or ulna/radius complex, the result is a crossunion, or synostosis.
For example, in a simple fracture of the midshaft of the radius and ulna, assume that the radius adheres to the ulna at the distal fracture site and that the radius does not heal because of angulated healing of the ulna. Such a situation can be described as a malunited fracture of the midshaft of the ulna with a nonunion of the radius and crossunion of the distal radius and ulna. When the diagnoses are listed, they might be given as (1) malunion, fracture, closed, midshaft, ulna, right; or (2) nonunion, fracture, closed, midshaft, radius, right, associated with crossunion.
Secondary union has multiple meanings. It implies delayed healing either by the eventual adhesion of granulating surfaces of bone fragments or surgical intervention late in the course of fracture healing to promote union.
Nutritional support is important in bone healing to augment medical and surgical care. Bones need mineral and protein to heal, another consideration in treatment.
This is a scheme of fracture classification for research purposes and a more uniform description in the literature. The scheme has not been validated or used by all investigators. It tends to be cumbersome in some instances, but in certain locations, the first letter and number modifier is very useful in describing the extent and pattern of fracture. For example, a C3 distal femur fracture is notated as 33.C3. This system is most commonly used in the distal femur, distal tibia, and distal humerus.
The system defines bones by number ( 1, humerus; 2, radius and ulna; 3, femur; 4, tibia and fibula; 5, spine, jaw, clavicle, and scapula; 6, pelvis and sacrum; 7, hand; 8, foot).
Nature of fracture is identified by letter ( A, simple involving at least 90% of the cortex or extraarticular; B, wedge with some contact between fragments or partial articular; C, complete with no contact between fragments or complete articular).
Degree of comminution is identified by number (A: 1, spiral; 2, oblique; 3, transverse less than 30 degrees. B: 1, spiral wedge; 2, bending wedge; 3, fragmented wedge. C: 1, spiral; 2, segmental; 3, irregular).
The subgroups .1, .2, and .3 further define the complexity of each of the above groupings.
Limitation: agreement among raters.
For uniform description in the literature.
IC1: no skin lesion
IC2: contusions but no skin laceration
IC3: circumscribed degloving
IC4: extensive closed degloving
IC5: necrosis from contusion
IO1: skin breakage from inside out
IO2: skin breakage from outside in < 5 cm, contusion at edges
IO3: skin breakage > 5 cm, increased contusion, devitalized edge
IO4: considerable full thickness contusion, abrasion, extensive open degloving, skin loss
MT1: no muscle injury
MT2: circumscribed muscle injury, one compartment only
MT3: circumscribed muscle injury, two compartments
MT4: muscle defect, tendon laceration, extensive muscle contusion
MT5: compartment syndrome, crush syndrome with wide injury zone
NV1: no neurovascular injury
NV2: isolated nerve injury
NV3: isolated vascular injury
NV4: extensive segmental vascular injury
NV5: combined neurovascular injury, subtotal and total amputation
The trend toward standard classification of fractures and dislocations is certainly a step forward, but such a system is designed for computer storage and is sometimes difficult to apply when viewing a fracture for the first time. It should not be forgotten that most of these specific classification systems were developed to address a specific set of circumstances. Attempting to apply them to other areas frequently leads to misinterpretation and erroneous conclusions. The authors, therefore, feel that these systems should be interpreted as meant by the original authors. The reference is indicated in a footnote (see Bibliography for full reference citations).
Based on mechanism and injury patterns.
Extension loading force: fracture spinal process and possible lamina, with compression severe displacement with retrolisthesis superior on inferior vertebra.
Flexion loading force: unilateral or bilateral facet dislocation that, if with posterior ligament disruption, produces facet locking. May also have vertebral compression fracture or teardrop fracture.
Neutral load: burst fracture, very unstable if complete ligamentous disruption.
To define location of most common sites of occurrence and of nonunion.
Group I: fractures of middle third
Group II: fractures distal to coracoclavicular ligament, nonunion frequent
Group III: fractures of proximal end; nonunion and displacement rare
Limitations: does not incorporate other factors such as degree of trauma.
Based on location of fracture; to define fracture pattern likely to require surgery for healing.
Type I: avulsion fracture of tip of odontoid
Type II: fracture at junction of odontoid to body of vertebra
Type III: fracture line extends downward into cancellous bone of body of vertebra
Based on location of failure of integrity.
Type A injuries: failure under axial compression of the anterior elements with intact posterior constraining elements
Type B injuries: failure of the posterior constraining elements (tension band or PLC injuries in case of TL spine)
Type C injuries: failure of anterior and posterior elements leading to displacement
Based on direction or mechanism of force.
first degree: transsyndesmotic fracture of the fibula
alternate first degree: rupture of the anterior tibiofibular ligament with or without spiral fracture of the proximal fibula
second degree: rupture of the deltoid ligament
alternate second degree: avulsion of the medial malleolus
third degree: fracture of the entire lower end of the tibia and fibula with external rotation
first degree: transverse fracture of the medial malleolus at or below its base
second degree: rupture of the deltoid ligament or fracture of the medial malleolus followed by a fracture of the distal fibula
third degree: fracture of both lower tibia and medial malleolus lateral displacement
first degree: avulsion of the fibular malleolus at or below its base
second degree: avulsion of the fibular malleolus at or below its base with medial malleolus below plafond, a shear vertically into tibial shaft
third degree: supramalleolar fracture in both the tibia and fibula with medial displacement
first degree: isolated marginal fracture of the distal weight-bearing plate of the tibia
second degree: comminution of the tibial plafond
third degree: T or Y fractures (V fracture of Gosselin)
Limitations: fracture patterns overlap.
Roentgenographic basis for stability versus displacement, which requires surgical reduction.
Type I: nondisplaced fracture that can be seen only on one view
Type II: visible fracture line with minimal displacement
Type III: displacement of more than 2 mm on all views
Type IV: severe displacement with complete separation of fracture edges
Based on mechanism of injury; to help define management.
Type 1: fracture of any portion of the ulna diaphysis with anterior angulation and anterior dislocation of the radial head
Type 2: fracture of the ulnar diaphysis with posterior angulation and posterior or posterolateral dislocation of the radial head
Type 3: fracture of the ulnar metaphysis with lateral or anterolateral dislocation of the radial head
Type 4: proximal fracture of both bones at the same level with anterior dislocation of the radial head
Limitations: some controversy as to relationship to treatment; types I and II have equivalents that involve dislocation radial head only (type 1) and fractured radial head.
Too complicated for inclusion, a complex system based on angulation, dislocation, and associated injury. See Arslan H et al.
To define stages of osteochondritis of bone.
Stage I: normal x-ray but positive bone scan or change seen on magnetic resonance imaging (repeated minitrauma)
Stage II: incomplete separation of subchondral fragment (single injury event)
Stage IIA: cyst formation (repeated minitrauma)
Stage III: complete separation of fragment, which is in anatomic position (single injury event)
Stage IV: separation of fragment (single injury event)
To define surgical approach and prognosis for fractures near and around the femoral neck.
Type 1: intertrochanteric f., simple to reduce and maintain
Type 2: intertrochanteric f. with comminution and additional coronal seen from lateral
Type 3: subtrochanteric f. with at least one fracture line passing just distal to or through lesser trochanter
Type 4: fractures of the trochanteric region and proximal shaft and fracture in two planes requiring two-plane fixation
Limitations: crosses over from subtrochanteric fracture type to intertrochanteric and neck fractures.
To define shape and direction of elbow capitellar fractures.
Type 1: shear fracture in plane of capitellum involving none or little of the trochlea
Type 2: a variable amount of the cartilage of the capitellum with minimal attached subchondral bone
Type 3: comminuted or compression fracture of the capitellum
Based on location of fracture and association with displacement and effect on blood supply; to define prognosis for long-term outcome with particular reference to avascular necrosis.
Type I: minimal displacement, only one source of blood supply might be disrupted
Type II: subtalar subluxation or dislocation, two or three sources of blood supply might be affected
Type III: body of talus dislocated from the ankle and the subtalar joint
Type IV: fracture of talar neck associated with dislocation of the body from the ankle, or subtalar joint and additional subluxation or dislocation of the head of the talus from the talonavicular joint
Four columns: anterior, right pillar, left pillar, and posterior.
For each column, an analogue scale using fracture displacement and ligament disruption is given:
Fracture nondisplaced with mild ligamentous 1–3 mm (analogue scale 0–1)
Fracture displaced 1–3 mm, mild ligamentous 1–3 mm (analogue scale 1–2)
Fracture displaced 1–3 mm, moderate ligamentous 3–5 mm (analogue scale 2–3)
Fracture displaced 3–5 mm (analogue scale 3–4)
Fracture displaced > 5 mm, severe ligamentous > 5 mm (analogue scale 4–5)
Based on x-ray analysis; reflects the mechanism of type IV Salter fractures of the distal tibia and fibula and helps predict retardation of growth.
Group I: epiphysis not fractured
Group 1a: abduction injury with fracture of the distal fibular shaft and lateral displacement
Group 1b: supination/hyperplantar flexion injury with posterior metaphyseal fragment of the tibia and posterior displacement
Group 1c: supination/external rotation injury with large anteromedial metaphyseal component, tibia, and posterior displacement
Group 1d: adduction injury (rare), posteromedial metaphyseal fragment of the tibia with fracture of the distal fibular shaft and medial displacement
Group II: vertical fracture through epiphysis with shift of lateral fragment
Group III: adduction injury, Salter type I or II fibular slip with type IV medial malleolar fracture
Attributes classification to Delbet; no purpose given.
Type I: transepiphyseal separations with or without dislocation of femoral head
Type II: transcervical fractures, displaced and nondisplaced
Type III: cervicotrochanteric fractures, displaced and nondisplaced
Type IV: intertrochanteric fractures
To define treatment.
Avulsion group: transverse fracture line separating a small fragment of olecranon with or without displacement
Oblique group: primary failure being an oblique line from the trochlear notch to the distal outer ulnar shaft, degree of comminution staged a to d
Stage a: single fracture line, displaced and nondisplaced
Stage b: nondisplaced single central large V-shaped fragment
Stage c: displaced single central large V-shaped fragment
Stage d: highly comminuted central pieces of bone with displacement
Fracture dislocation (Monteggia group): fracture line at or slightly proximal to coronoid, which may result in anterior fracture or dislocation of the elbow
Unclassified group: high-energy, highly comminuted fractures not matching previous descriptions
Denis Classification for Sacral Fractures
Denis 1: Lateral to foramen
Denis 2: Through or involving foramen
Denis 3: Medial to foramen
Uses Lauge-Hansen guidelines, foot position, and direction of force in correlation with the Salter-Harris classification to plan surgical and other treatment approaches.
Supination-inversion: inversion force applied to supinated foot
Grade I: Salter-Harris type I or II of distal fibular epiphysis
Grade II: grade I with Salter-Harris type III or IV of tibial epiphysis
Supination-plantar flexion: plantar flexion force on supinated foot
Grade I: Salter-Harris type I or II of distal tibia, usually with posterior displacement
Supination-external rotation: external rotation ankle force on fully supinated foot
Grade I: Salter-Harris type II of distal tibia with long spiral fracture of distal tibia
Grade II: grade I with spiral fracture of fibula
Pronation-eversion-external rotation: a combination of eversion and external rotation force on pronated foot
Grade I: posterolateral displacement of Salter-Harris type II tibial fracture with short oblique fibular fracture above physis
Limitations: fractures not covered under this system include Salter-Harris type III distal tibia and triplane fracture (as described by author).
Grouped by stable or unstable and open or closed.
Type I: closed fracture may or may not exist
Type II: superficial open injury
Type III: open injury tendon exposed
Type IVa: physical injury (pediatric)
Type IVb: involving 20–50%
Type IVc: involves greater 50% joint surface
Based on direction of injury force (A–C superior to inferior, and D–F anterosuperior to posteroinferior); helps define method of closed and open management.
Type A: nondisplaced fracture inferior to lateral process of talus and through lateral cortex
Type B: type A with shearing of sustentaculum tali along with one-third to one-half of the posterior facet
Type C: type B with depression of joint and superior posterior displacement of distal portion
Type D: affects lateral half or two-thirds of subtalar joint and fracture of the lateral cortex without displacement
Type E: type D with superior displacement of anterior portion of calcaneus
Type F: type E with displacement of posterior facet of calcaneus and further superior migration of anterior portion
Grouped by stable or unstable and expected response to treatment.
Type I: fracture line extends upward and outward from lesser trochanter:
Undisplaced stable
Displaced reduced with stable medial apposition
Displaced unreduced with no medial apposition
Comminuted unstable with no medial apposition
Type II: reversed obliquity with line from lesser trochanter to inferior lateral cortex
Limitations: directed at open versus closed management, which is no longer used.
System Based on Frequency, Etiology, and Direction.
Frequency
Solitary 1 episode
Occasional 2–5 episodes
Frequent >5 episodes
Etiology
Traumatic
Atraumatic
Direction
Anterior
Inferior
Posterior
The direction is confirmed at the time of the physical examination using provocative tests to determine directions most closely reproduces symptoms.
Severity
Subluxation
Dislocation
To define stages of appearance and attachment of lesion to subchondral bone.
Stage A: smooth, intact, but soft or ballottable
Stage B: rough surface
Stage C: fibrillations or fissures
Stage D: flap present or bone exposed
Stage E: loose, nondisplaced fragment
Stage F: displaced fragment
To define stages of attachment of subchondral bone.
Stage I: cystic lesion within dome of talus
Stage IIA: cystic lesion with communication to talar dome surface
Stage IIB: open articular surface lesion with overlying nondisplaced fragment
Stage III: nondisplaced lesion with lucency
Stage IV: displaced fragment
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here