Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Congenital chest wall deformities fall into two groups: those with overgrowth of the cartilages causing either a depression or protuberance and those with varying degrees of either aplasia or dysplasia. Pectus excavatum (PE), also known as an “excavated, sunken, or funnel chest,” is the most common chest wall anomaly in most countries around the world. Pectus carinatum (PC), a chest wall protuberance, makes up approximately 10–15% of chest wall deformities in North America, whereas combined PE/PC deformities are found in about 5%. Jeune syndrome, or asphyxiating chondrodystrophy, is an extreme form of mixed PE/PC and is very rare.
Poland syndrome and bifid sternum represent different forms of aplasia of the anterior chest wall. Poland syndrome consists of varying degrees of dysplasia of the breast, the pectoralis muscles, and ribs. In bifid sternum, partial or complete failure of the midline fusion of the sternum is seen. This may result in ectopia cordis or varying degrees of sternal dysplasia and deficiencies of associated structures such as the heart, pericardium, diaphragm, and anterior abdominal wall (pentalogy of Cantrell).
Many of these deformities are present at birth. Some cases, such as ectopia cordis, are incompatible with life and have rarely been successfully repaired. Chest wall deformities are frequently associated with a systemic weakness of the connective tissues and with poor muscular development of the abdominal region, thorax, and spine. An association with PE and Marfan syndrome, Ehlers–Danlos syndrome, and scoliosis is well known. Other associations such as between omphalocele and bifid sternum have been identified as well ( Table 20.1 ).
| Total Evaluated | 4642 |
|---|---|
| Pectus excavatum (PE) only | 3478 |
| Mixed excavatum/carinatum | 231 |
| Carinatum only | 788 |
| No chest wall deformity | 145 |
| Male-to-female ratio | 4.13:1 |
| Family history of PE | 35.1% |
| Scoliosis | 24.5% |
| Marfan syndrome: Formal diagnosis | 1.8% |
| Marfanoid/presumed Marfan syndrome | 8.8% |
| Poland syndrome | 0.3% |
PE is a depression of the anterior chest wall of variable severity and can usually be characterized as mild, moderate, or severe. The deformity may be localized and deep (“cup-shaped”; Fig. 20.1A ) or diffuse and shallow (“saucer-shaped”; see Fig 20.1B ), and can be symmetric or asymmetric. The depth and extent of the depression determine the degree of cardiac and pulmonary compression, which, in turn, determines the degree of physiologic effect. Only one-third of patients referred from the Norfolk, Virginia, area have had a deformity severe enough to require operative correction. Even with referral of patients with a severe deformity from other centers, the ratio of operative correction at Children’s Hospital of the King’s Daughters (CHKD) has been only about 60% ( Box 20.1 ).

|
|
|
|
|
|
|
|
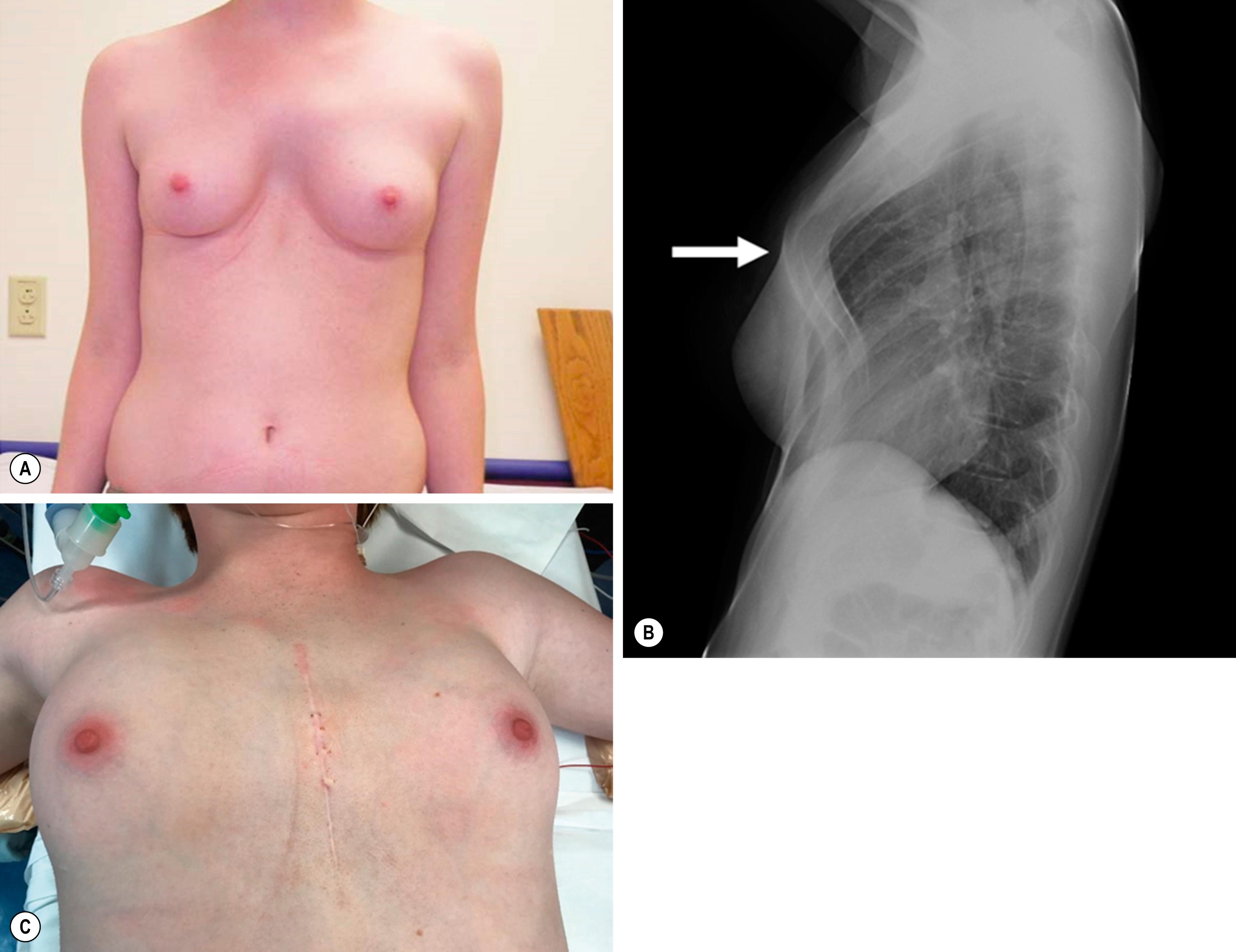
This chest wall deformity may be noted in infancy ( Fig. 20.2 ) and usually progresses with age and growth. With rapid growth at puberty, the progression may become especially pronounced, a fact apparently unknown to many pediatricians, who mistakenly advise families of younger patients that the condition will resolve spontaneously. We have seen many families who were given this advice and missed the opportunity to have the deformity repaired before puberty while the chest was still soft and malleable and before it interfered with physical performance.

PE was recognized by the ancient Egyptians. Leonardo da Vinci made a drawing of an elderly man with pectus excavatum as early as the 16th century. In 1594, Bauhinus described the clinical features of PE in a patient who had pulmonary compression with dyspnea and paroxysmal cough, both attributed to the severe PE. The familial predisposition was first noted by Coulson in 1820, who cited a family of three brothers with PE. In 1872, Williams described a 17-year-old patient who was born with a PE and whose father and brother also had the condition.
Numerous other case reports appeared in the 19th century, including a five-case report by Ebstein in 1882 that covered the clinical spectrum of this condition. Treatment at that time was limited to “fresh air, breathing exercises, aerobic activities, and lateral pressure.”
Thoracic surgery remained forbidden territory until the early years of the 20th century. The first attempt at PE correction was a tentative approach in 1911 by Meyer, who removed the second and third costal cartilages on the right side without improvement. Sauerbruch, one of the pioneers of thoracic surgery, used a more aggressive approach in 1931 by excising a section of the anterior chest wall, which included the left fifth to ninth costal cartilages as well as a segment of the adjacent sternum. Before his operation, the patient was incapacitated by severe dyspnea and palpitations, even at rest, and was unable to work in his father’s watch factory. After recovery, the heart could be seen to pulsate under the muscle flap, but the patient was able to work without dyspnea and was married 3 years later.
In the 1920s, Sauerbruch performed the first PE repair that used the bilateral costal cartilage resection and sternal osteotomy technique later popularized by Ravitch. He also advocated external traction to hold the sternum in its corrected position for 6 postoperative weeks. His technique was soon adapted by others in Europe and rapidly gained popularity in the United States. In 1939, Ochsner and DeBakey published their experience with this approach and reviewed the surgical literature on the subject. Also in 1939, Lincoln Brown published his experience in two patients and reviewed the literature with particular reference to the cause of PE. He was impressed with the theory that short diaphragmatic ligaments and the pull of the diaphragm on the posterior sternum were causative factors.
Ravitch initially subscribed to the short ligament theory as well. As a result, he advocated even more radical mobilization of the sternum, with transection of all sternal attachments, including the intercostal bundles, rectus muscles, diaphragmatic attachments, and excision of the xiphisternum. In 1949, he published his experience with eight patients in which he used this radically extended modification of Sauerbruch’s technique of bilateral cartilage resection and sternal osteotomy, but without external traction.
The lack of external traction may have led to an increased recurrence of the condition. As a result, Wallgren and Sulamaa introduced the concept of internal support in 1956 by using a slightly curved stainless steel bar that was pushed through the caudal end of the sternum from side to side and bridged the newly created gap between the sternum and ribs. In 1961, Adkins and Blades modified internal bracing further by passing a straight stainless steel bar behind, rather than through, the sternum. This technique was rapidly adopted for patients of all ages.
As early as 1958, Welch and Gross advocated a less radical approach than that of Ravitch. Welch showed excellent results in 75 patients without dividing all the intercostal bundles or the pectus muscle attachments. However, he still advocated performing the procedure in young patients. Conversely, Pena was very concerned about the idea of resecting the cartilages from very young patients and demonstrated that asphyxiating chondrodystrophy developed in baby rabbits after cartilage resection during their growth phase. Later, Haller et al. reported the risk of acquired asphyxiating chondrodystrophy following operative correction in young children. As a result, many surgeons stopped performing open PE repair in young children and waited until the child reached puberty. They also reduced the amount of cartilage resected and spoke about a modified Ravitch procedure, which was really the original Sauerbruch procedure.
In 1997, we at CHKD published our 10-year experience with a minimally invasive technique that did not utilize cartilage resection or sternal osteotomy, but instead relied on internal bracing made possible due to the flexibility and malleability of the costal cartilages. The rationale for this technique was based on the three following observations:
Malleability of the chest: Children have a soft and malleable chest. In young children, the chest is so soft that even minor respiratory obstruction can cause severe sternal retraction. Trauma rarely causes rib fractures and flail chest because the chest is so soft and malleable. Thus, the American Heart Association recommends “using only two fingers” when performing cardiac resuscitation in young children and “only one hand in older children” for fear of crushing the heart.
Chest reconfiguration: In middle-aged and older adults, a barrel-shaped chest configuration develops in response to chronic obstructive respiratory diseases such as emphysema. If older adults are able to reconfigure the chest wall, children and teenagers should be able to remodel as well, especially with the increased malleability of their anterior chest wall.
Bracing: The role of braces and serial casting in successfully correcting skeletal anomalies such as scoliosis, clubfoot, and maxillomandibular malocclusion by orthopedic and orthodontic surgeons is well established. The anterior chest wall, being even more malleable than the previously mentioned skeletal structures, is ideally suited for this type of correction.
PE occurs in approximately 1 in 1000 children and constitutes 80% of all chest wall deformities at CHKD (see Table 20.1 ). However, this is not the case in all countries. In Argentina, PC is more common than PE. PE also is rare in African-Americans and Africans. A familial predisposition, already noted in the 19th century, has been found in almost 40% of our patients. We have seen families with three siblings, as well as cousins and other family members, who had a PE deformity severe enough to require correction. We also have seen patients whose fathers and grandfathers had the deformity. The male-to-female ratio of 4:1 in our series of PE patients is similar to that of other large series. Female patients have an increased risk of associated scoliosis. Inheritance is variable, being autosomal dominant, autosomal recessive, X-linked, and multifactorial in different families.
The association with a connective tissue disorder is higher than in the normal population. The vast majority of our patients have an asthenic build, and a definitive diagnosis of Marfan syndrome has been found in 2% of our patients. An additional 9% have had clinical features suggestive of Marfan syndrome. Ehlers–Danlos syndrome has been present in approximately 4%. Mild scoliosis has been noted in 25% of our patients. In our experience, a severely asymmetric PE tends to aggravate the postural abnormality of scoliosis. Correction of the PE has improved the mild scoliosis in many patients.
PE is noted in infancy in many patients (see Fig. 20.2 ) and usually progresses slowly as the child grows. Because young children have significant cardiac and pulmonary reserve and their chest wall is still very pliable, the majority of young children are asymptomatic. However, as they become older, the deformity becomes more severe and the chest wall becomes more rigid. Eventually, these children find that they have difficulty keeping up with their peers when playing aerobic sports. A vicious cycle may develop as patients stop participating in aerobic activities because of their inability to keep up. Subsequently, their exercise capacity diminishes further. The downward spiral is further promoted by the fact that these patients, already embarrassed by their deformity, will avoid situations in which they have to remove their shirts in front of other children, inhibiting participation in school and team activities.
By withdrawing from participation in activities with their peers, they also become depressed, which can affect their schoolwork. Most PE patients have a typical geriatric or “pectus” posture that includes thoracic kyphosis, forward-sloping shoulders, and a protuberant abdomen ( Fig. 20.3 ). A sedentary “couch potato” lifestyle may aggravate this posture, and the poor posture depresses the sternum even farther. For this reason, we always recommend an aggressive pectus posture exercise and breathing program, both preoperatively and postoperatively.

Many patients have a relatively mild PE deformity during childhood. Although the deformity may not always increase in severity, it is unlikely that it will spontaneously resolve. When the patients grow rapidly during puberty, the deformity often suddenly accelerates in severity. A mild condition may become severe in as little as 6–12 months. It is the rapid progression that alarms parents and stimulates them to seek consultation with a surgeon. Patients with a rapid progression of their deformity seem to exhibit the most pronounced symptom complex.
The earliest symptoms are shortness of breath and lack of endurance with exercise. As the PE progresses, chest pain and palpitations with exercise can develop, giving rise to exercise intolerance. Other symptoms include frequent and prolonged respiratory tract infections, which can lead to symptoms of asthma ( Table 20.2 ).
| Symptoms | Percent (%) |
|---|---|
| Shortness of breath, lack of endurance, exercise intolerance | 80 |
| Chest pain, with or without exercise | 70 |
| Frequent respiratory infections | 20 |
| Cardiology Indicators | |
| Cardiac compression | 85 |
| Cardiac displacement by computed tomography | 75 |
| Murmurs | 25 |
| Mitral valve prolapse | 13 |
| Pulmonary Indicators | |
| FVC <80% | 24 |
| FEV1% <80% | 29 |
| FEF25–75% <80% | 43 |
A study showed that PE patients have a poor body image, which has a major impact on their feeling of self-worth. Therefore, it is important to correct the deformity before it affects their ability to function normally. Just as one would not consider leaving a child with a cleft lip untreated, one should not leave a child with a severe PE untreated. Both have a physiologic and psychological impact on the child and adolescent.
In the last 15 years, there has been increasing acknowledgment in the medical community that a severe PE has a significant detrimental effect on cardiopulmonary function. In comparison to older studies, recent work has demonstrated the adverse effects more clearly and have shown that only in a minority of patients with PE are there no deleterious effects on cardiopulmonary function. Several factors play a role when evaluating cardiopulmonary function. These include the severity of the deformity, the inherent physical fitness of the individual patient, the patient’s age, any associated conditions, whether the tests are done supine or erect, and whether they are done at rest or during exercise. One study showed statistically significant and clinically meaningful improvements in stroke volume, cardiac output, and cardiac index after the minimally invasive repair of PE (MIRPE). An improvement in exercise cardiopulmonary function has been noted as well.
Cardiac effects from PE include decreased cardiac output, mitral valve prolapse, and arrhythmias. Compression of the heart results in incomplete filling and decreased stroke volume, which in turn results in decreased cardiac output. Cardiac compression may interfere with normal valve function. Mitral valve prolapse has been found in 13% of our patients and in up to 65% in other series. Prolapse occurs in only 1% in the normal pediatric population. In one study, the mitral prolapse resolved in about half of patients who underwent correction. Thus, both mechanical and connective tissue derangements can be involved. Dysrhythmias, including first-degree heart block, right bundle branch block, and Wolff–Parkinson–White syndrome, were found in 16% of patients in one study.
Pulmonary effects result from poor motion of the depressed part of the chest wall. Normal chest wall motion includes “pump handle” movement of the sternum. The lower sternum moves up and out, like the handle of a mechanical water pump. Physical examination, and now motion capture analysis, show that this motion is almost absent in the depressed area of the PE chest. Instead, patients compensate by increased abdominal diaphragmatic breathing. Following correction, this motion is indistinguishable from that of the normal chest wall.
Pulmonary function testing shows statistically and clinically meaningful diminution in static pulmonary function tests (e.g., forced vital capacity, forced expiratory volume in 1 second), even though most patients do not have a problem with their airway or pulmonary parenchyma (see Table 20.2 ). These values improve after correction. Exercise pulmonary function testing also shows improvement. Stress testing has shown an increase in oxygen consumption for a given exercise compared with normal patients. This indicates that the work of breathing is increased in patients with PE and explains why they often lack endurance.
A complete history is obtained and physical examination performed on all patients and includes documenting photographs. Younger patients with a mild to moderate deformity are treated with a posture and exercise program in an attempt to halt the progression and are followed at yearly or longer intervals ( Fig. 20.4 ).
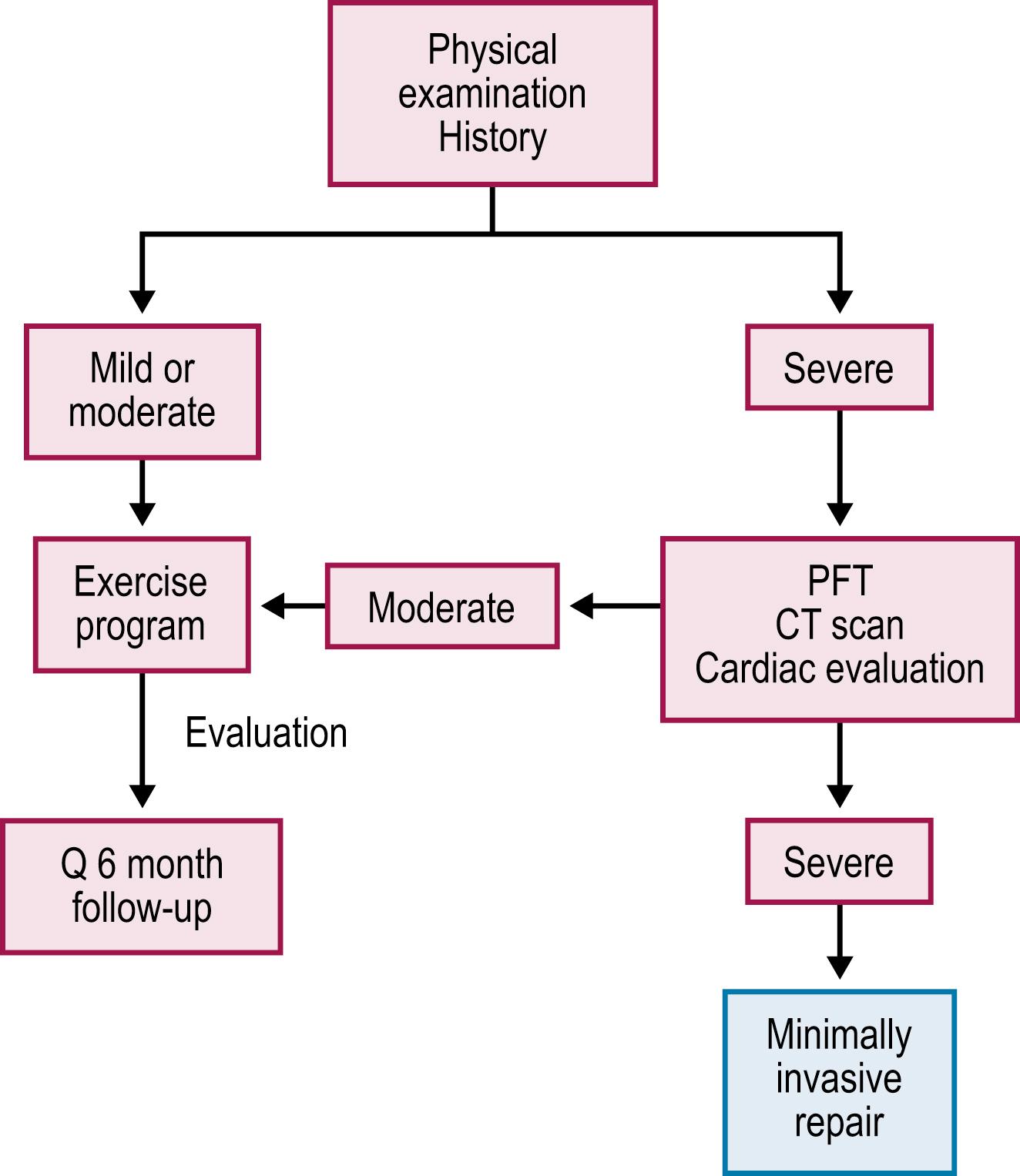
Patients with a severe PE deformity or those with documented progression also are treated with the exercise and posture program. Additionally, they undergo objective studies to evaluate whether their condition is severe enough to warrant repair. These studies include pulmonary function tests (PFTs), thoracic computed tomography (CT), or magnetic resonance imaging (MRI), as well as a cardiac evaluation that includes an electrocardiogram (ECG) and an echocardiogram.
CT scans are very helpful because they clearly show the degree of cardiac compression and displacement, the degree of pulmonary compression and atelectasis, whether there is asymmetry of the chest, sternal torsion, compensatory development of a barrel-chest deformity in long-standing deformities, and ossification of the cartilage in patients with previous repairs ( Fig. 20.5A,B) . They also are used to calculate the CT index, which gives an objective measurement for comparing the severity among patients. The CT index is calculated by dividing the transverse diameter by the anteroposterior diameter ( Fig. 20.5C ).
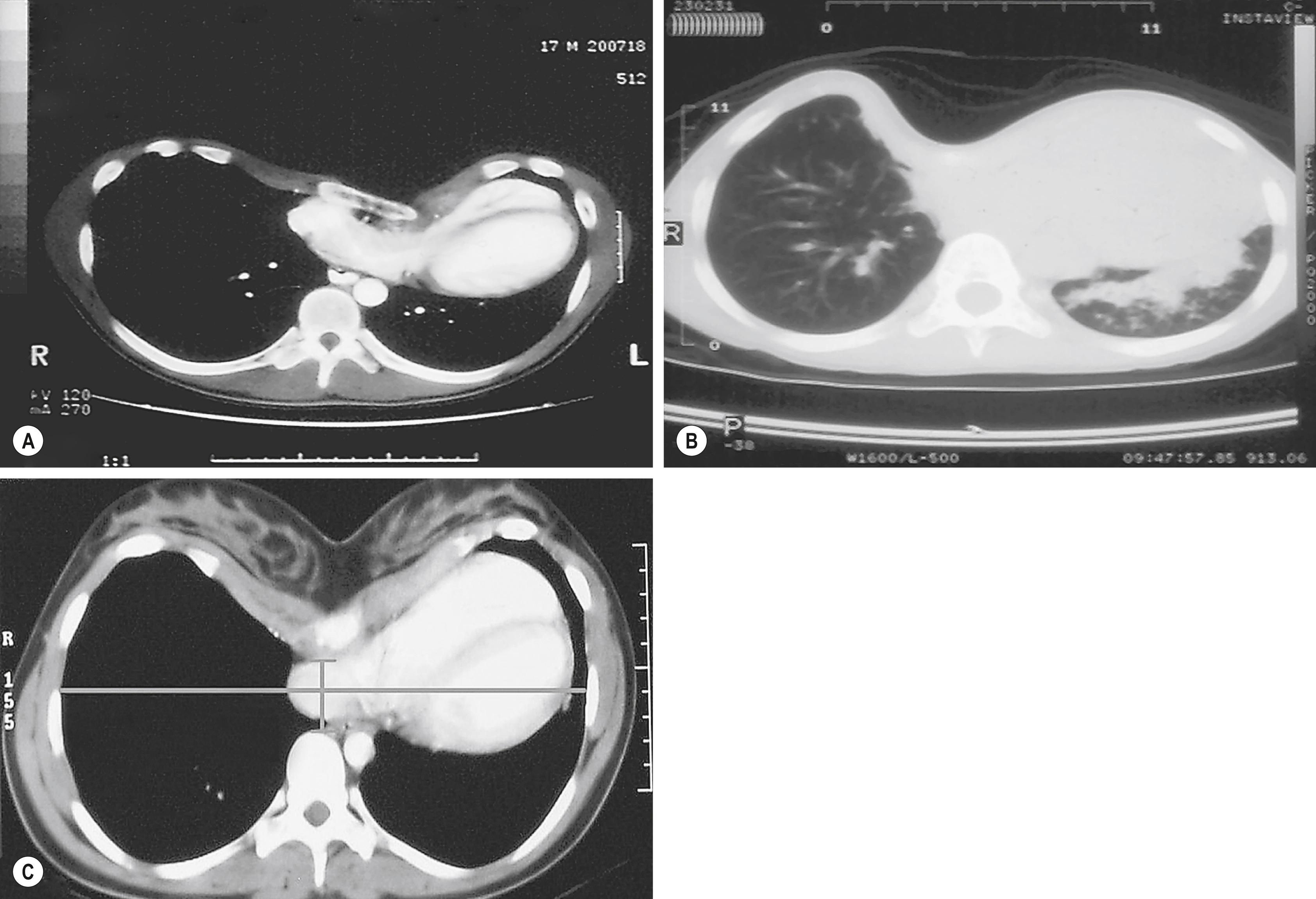
We have used MRI of the chest instead of CT scan to diminish radiation exposure. However, MRI does not give as clear a picture of the bony structures, which are the central issue. Cardiac MRI, which should be able to provide the same information as echocardiography and CT scan, remains in development.
Determination of a severe PE and the need for repair include two or more of the following criteria: (1) a CT index greater than 3.2 or correction index greater than 24% ; (2) PFTs that indicate restrictive airway disease; (3) a cardiology evaluation in which compression is causing murmurs, mitral valve prolapse, cardiac displacement, or conduction abnormalities visible on the echocardiogram or ECG; (4) documentation of progression of the deformity with associated physical symptoms other than isolated concerns of body image; (5) a failed Ravitch procedure; or (6) a failed MIRPE. With these criteria, only approximately 60% of patients referred to us are found to have a deformity severe enough to warrant correction (see Box 20.1 ). ,
The age parameters for operative correction depend on the type of repair selected. Unlike the more invasive procedures (e.g., Ravitch procedure, sternal turnover), there is no interference with growth plates with the MIRPE. Therefore, it can be done at any age, as evidenced by the fact that we have successfully operated on patients from ages 13 months to 31 years ( Fig. 20.6 ). However, the concern with patients younger than 11 years is that if the procedure is performed at too young an age, many years of subsequent growth remain during which the PE can recur.
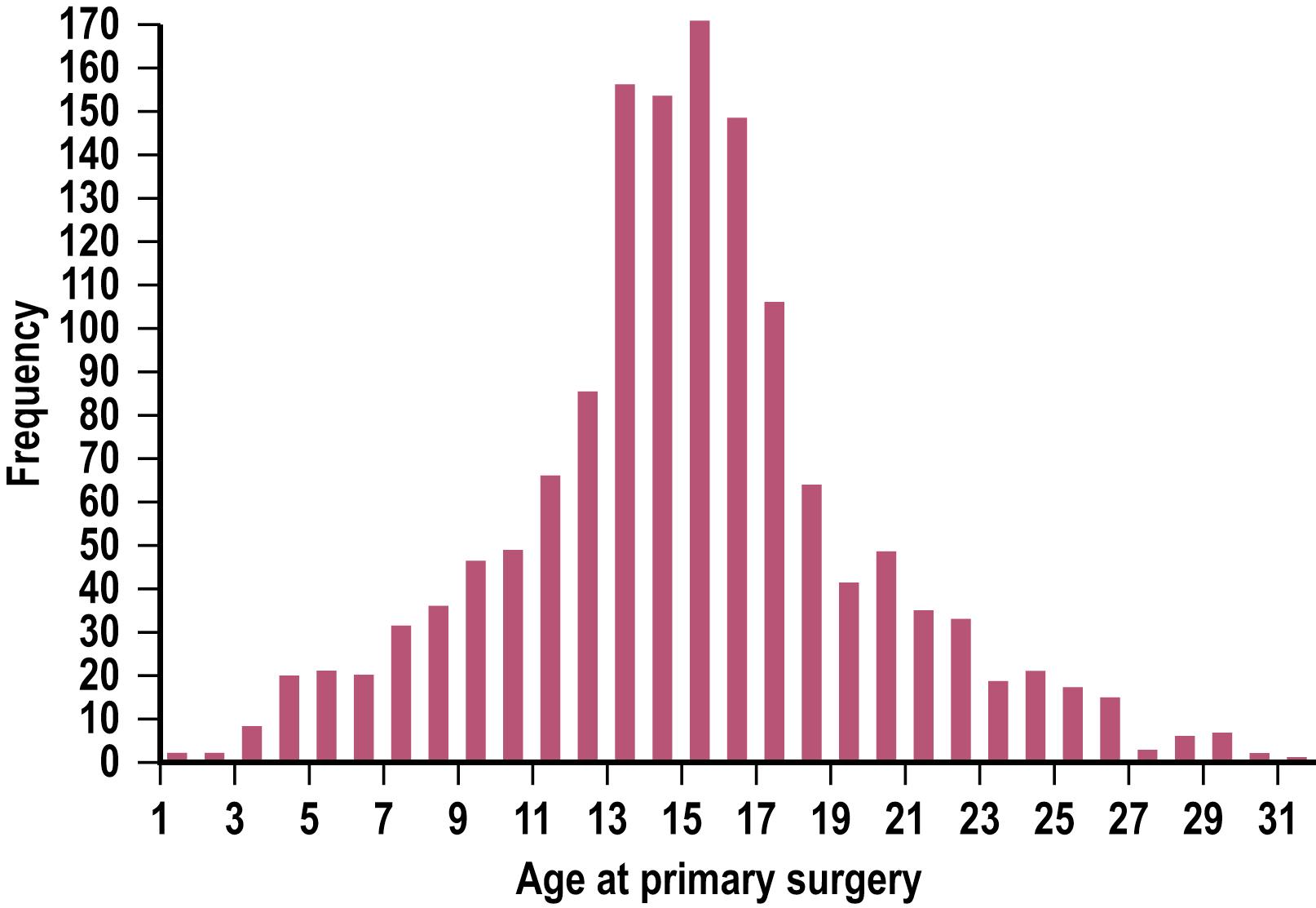
Our experience suggests that the optimal age for repair is 11–14 years. At this age, the patient is prepubertal, the chest is still soft and malleable, there is a quick recovery with a rapid return to normal activities, and results are excellent. After puberty, the flexibility of the chest wall is decreased, sometimes requiring the insertion of two bars, which makes the operation and recovery more difficult. However, patients older than 20 years have been uniformly pleased with their results. Several other centers have reported success with patients up to age 44 years.
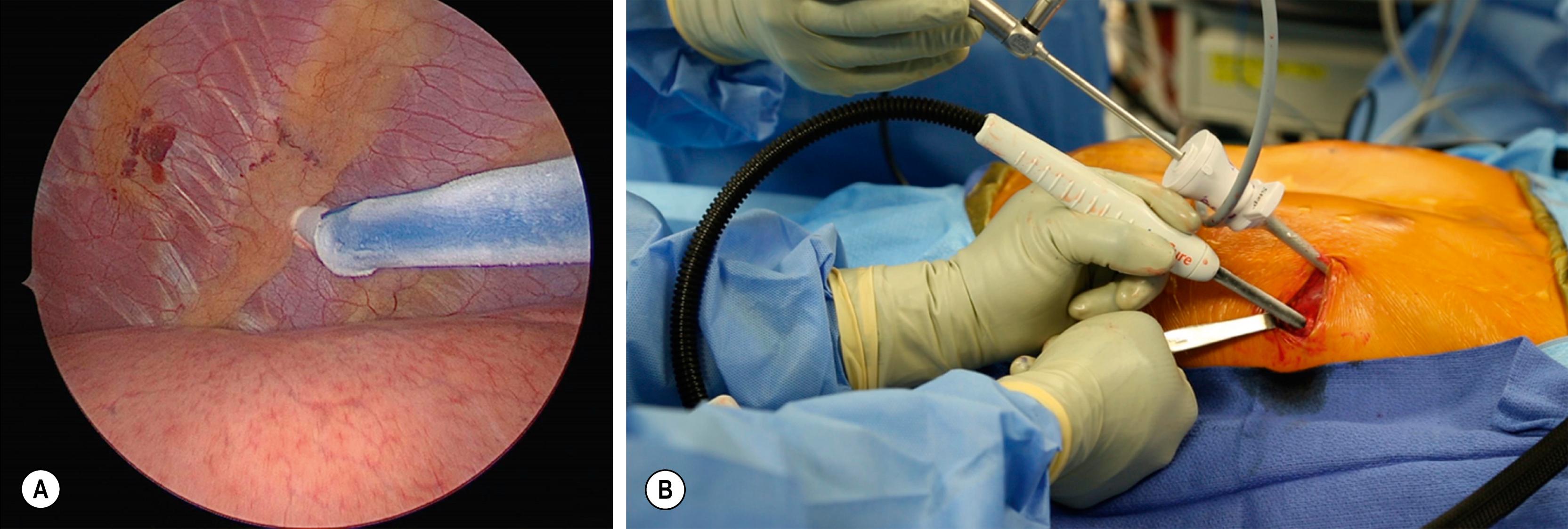
In the last few years, newer options for treatment of PE have been developed. An option that is being used internationally is the vacuum bell device as a sternal lifter ( Figs. 20.7 and 20.8 ). Whether this technique is effective for all patients with PE is not yet known but is unlikely. In a small study of 29 patients, the average improvement in the Haller index was 0.76. Vacuum bell suction was most effective in patients with low body weight and smaller chest depth. Another innovation has been the development the Magnetic Mini-Mover (Mini-Mover), which is currently envisioned for treatment of prepubertal patients with PE. In a pilot trial with 15 patients and a mean treatment duration of 25 months (range 18–33 months), the Haller index decreased in 5, remained stable in 2, but increased in 6. Of the 15 patients, 7 had breakage of the implant’s titanium cables because of fatigue.


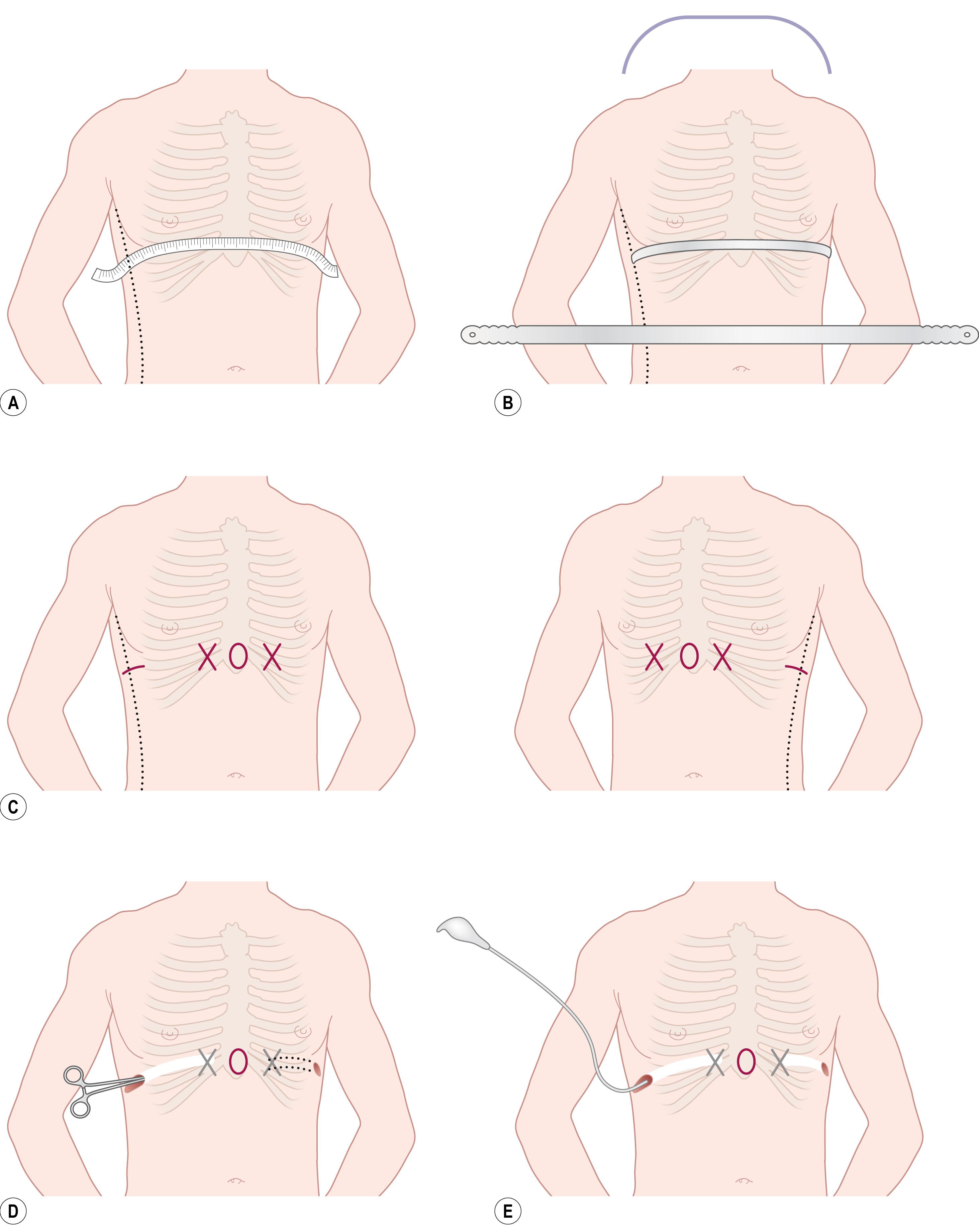
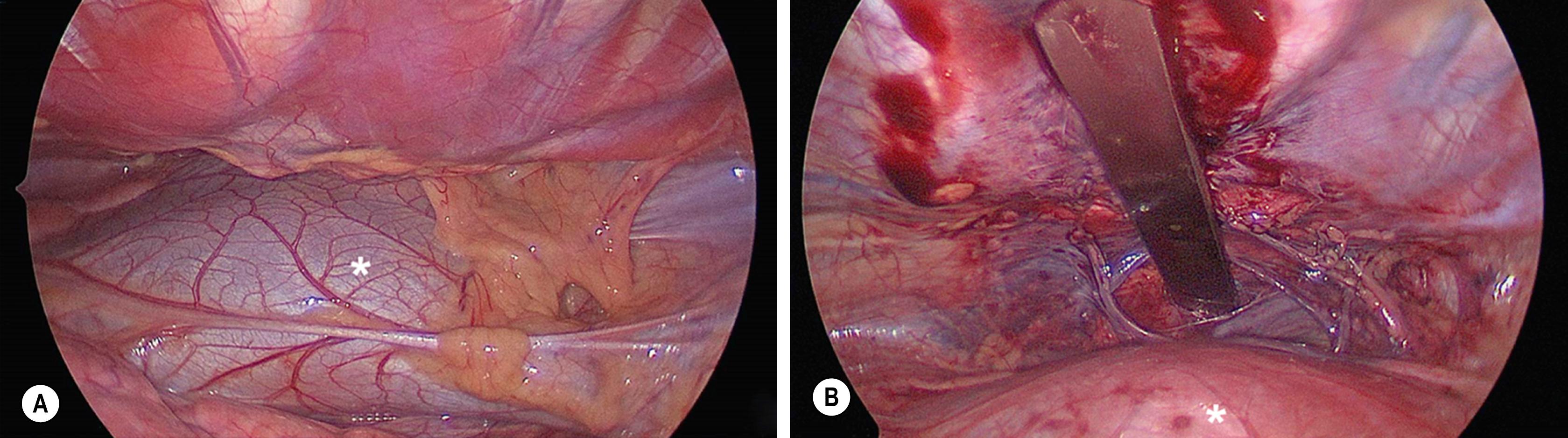
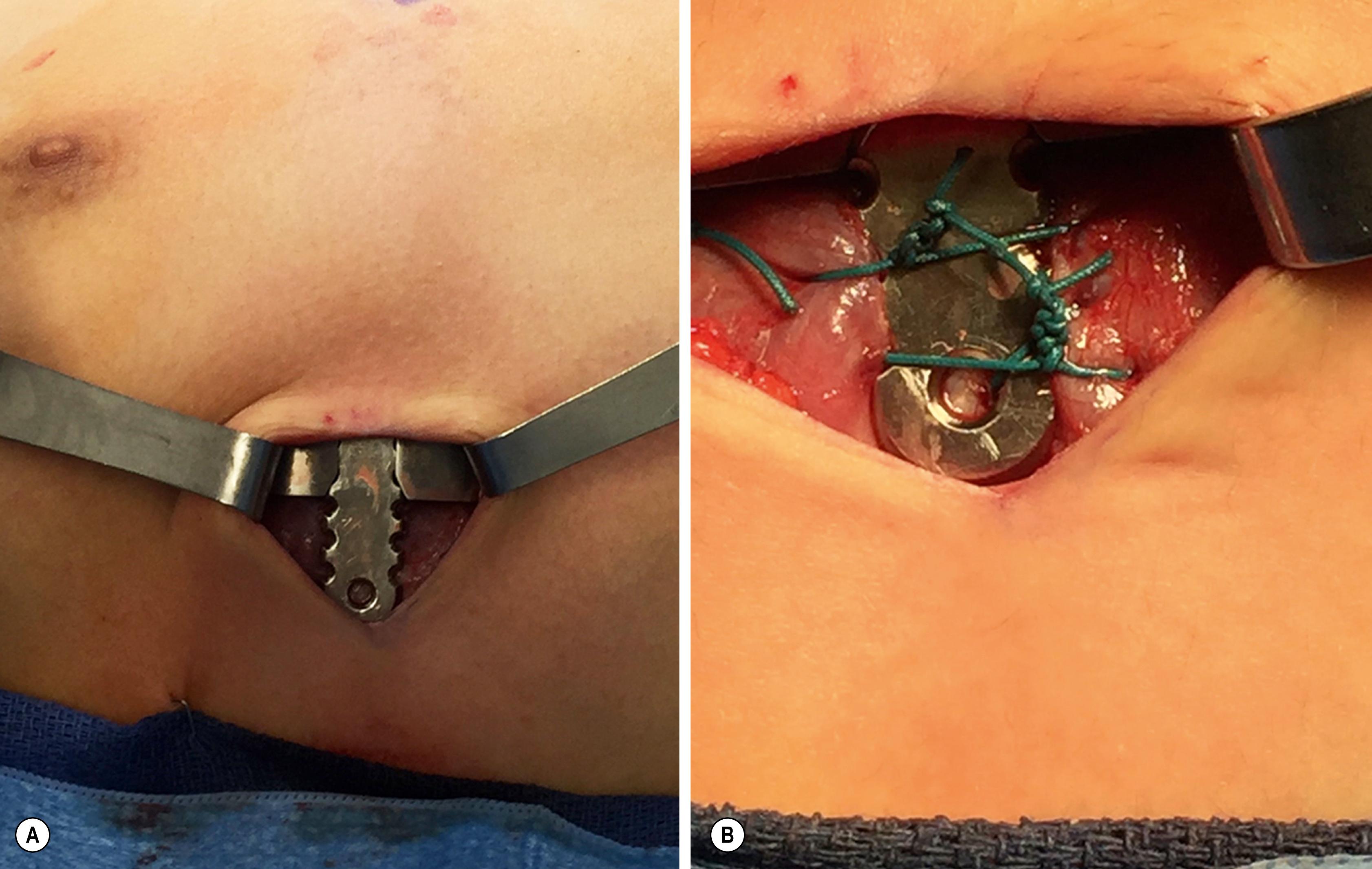
The MIRPE ( Fig. 20.9 ) involves making incisions on each side of the chest and creating a subcutaneous tunnel from the lateral thoracic incision to the top of the pectus ridge on each side. Sternal elevation, by use of a crane (Rultract, Inc., Cleveland, OH, or other device), vacuum bell, or sturdy assistant, can be used to help lift the sternum away from the heart. At the top of the ridge, bilateral thoracostomy incisions are created and a large introducer is inserted into the chest cavity under thoracoscopic visualization. Very carefully, the pleura and pericardium are dissected off the undersurface of the sternum and the introducer is slowly advanced across the mediastinum and exteriorized through the thoracostomy site on the contralateral side. When the introducer is in place under the sternum, the sternum can be further elevated from its depressed position. Once the sternal depression is corrected, two umbilical tapes are attached to the introducer and the introducer is slowly withdrawn. The length of the bar is determined by measuring the distance from midaxillary line to midaxillary line and subtracting 2.5 cm (1 inch). The stainless steel bar is bent to the desired configuration using a bar bender. (Patients with metal allergy require a titanium bar, which is bent at the factory according to the patient’s CT scan.) All of these maneuvers are performed using thoracoscopy for visualization ( Fig. 20.10 ). The thoracoscope can be placed in the right, left, or both hemithoraces. The pectus support bar is then attached to the umbilical tape and slowly guided through the substernal tunnel with its convexity facing posteriorly until it emerges on the contralateral side. Once the bar is positioned inside the chest with the convexity facing posteriorly, it is turned over by using specially designed bar flippers, resulting in correction of the excavatum. The bar is secured with a stabilizer on one side and absorbable sutures around the bar and underlying ribs on the other side. These sutures can be placed with an EndoClose needle (Covidien, Mansfield, NJ) using thoracoscopy or with an orthopedic tendon passer. Stabilizers also can be used on both sides to secure the bar. It is essential that the bar is well stabilized ( Fig. 20.11 ) or it can become displaced. Once the bar is secure, the thoracoscope is removed, the pneumothorax evacuated, and the incisions are then closed.
The patient is discharged from the hospital, usually on the third or fourth day after operation. Patients are instructed to refrain from sports or other similar activities for 6 weeks after the operation. All patients are restarted on an exercise and posture program to facilitate chest expansion and maintain a good posture.
A variety of measures have been used for pain management in the postoperative period. Many surgeons use a combination of intravenous narcotics, benzodiazepines, and nonsteroidal anti-inflammatory agents. Transition to oral medications is usually attempted on either the second or third postoperative day in preparation for discharge on day 4 or 5. A prospective randomized trial was performed in 110 patients who were randomized to either epidural analgesia or patient-controlled analgesia (PCA) following their PE repair. In the epidural group, the patients had a longer time in the operating room, more phone calls to anesthesia, and a statistically significant increase in hospital charges. Interestingly, the epidural catheter was removed within 24 hours or could not be placed in almost a quarter of the patients in the epidural group. The pain scores, as recorded by the patients, favored the epidural group in the first 2 days and the PCA approach in the last 2 days of their hospitalization. Recently, a new approach employing cryoablation of the intercostal nerves has been described ( Fig. 20.12 ). As more experience is gained, this approach may find favor if late neuralgia is not encountered. Patients younger than 13 years of age are generally able to stop all pain medications after 7–10 days, and patients 13 years and older often require pain medications for 10–14 days postoperatively.
The preoperative preparation and evaluation are the same for the open approach for pectus repair as for MIRPE. However, because of the risk of interference with growth plates in young children and the development of asphyxiating chondrodystrophy, the procedure should be reserved for patients who have initiated their pubertal growth. The open procedure is best suited for the older patients, especially those who have asymmetric or eccentric deformities, and patients with mixed PE/PC deformities. It is the only approach we have found effective for chondromanubrial deformities (also called Currarino–Silverman syndrome or pectus arcuatum) ( Fig. 20.13 ).
The open technique involves making an anterior thoracic incision and elevating skin and muscle flaps until the 3rd to 8th costal cartilages are exposed. The perichondrium is then incised longitudinally, and the deformed cartilages are either partially or completely removed. Most surgeons now advocate removing only a small section (1–2 cm) of the deformed cartilages as was originally advocated by Sauerbruch and Gross. An anterior table, wedge-shaped sternal osteotomy is performed at the angle of Louis. The sternum is elevated, and the osteotomy is closed with nonabsorbable sutures. Some surgeons insert a metal strut under the sternum to bridge the gap between the ribs and the sternum to prevent the sternum from sinking back into the chest. The perichondrial sleeves are approximated with absorbable sutures, drains are left, the muscle flaps are sutured back into position, and the incisions are closed. Postoperative management is similar to that for the MIRPE except that patients are required to refrain from contact sports for at least 3 months.
The MIRPE received rapid acceptance by the surgical community because the technique requires neither rib resection nor sternal osteotomy. Blood loss is minimal, the operating time is short, and the patient rapidly returns to regular activity.
Although the initial report from CHKD in 1998 presented a 10-year experience, the numbers were limited (42 patients) and the long-term results were affected by an early learning curve of using a support bar that was too soft. Moreover, in some of these patients, the bar was removed too early. From 1988 through December 2016, 1986 patients have had their initial operation at CHKD (see Box 20.1 ). Since the original paper, numerous important modifications have been made, both to the operative technique (e.g., routine use of thoracoscopy) and instruments, to minimize the risks of the operation and facilitate insertion and stabilization of the support bar. These modifications have markedly reduced the risks and complications and have been previously reported. In 60% of these patients, a single bar was used. Two bars were needed in 40% of the patients. The median length of stay has been 5 days ( Table 20.3 ).
| Length of Stay | Median Range | 4 Days2–14 Days |
|---|---|---|
| Blood loss | Median | 11 mL |
| Number of bars |  |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here