Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
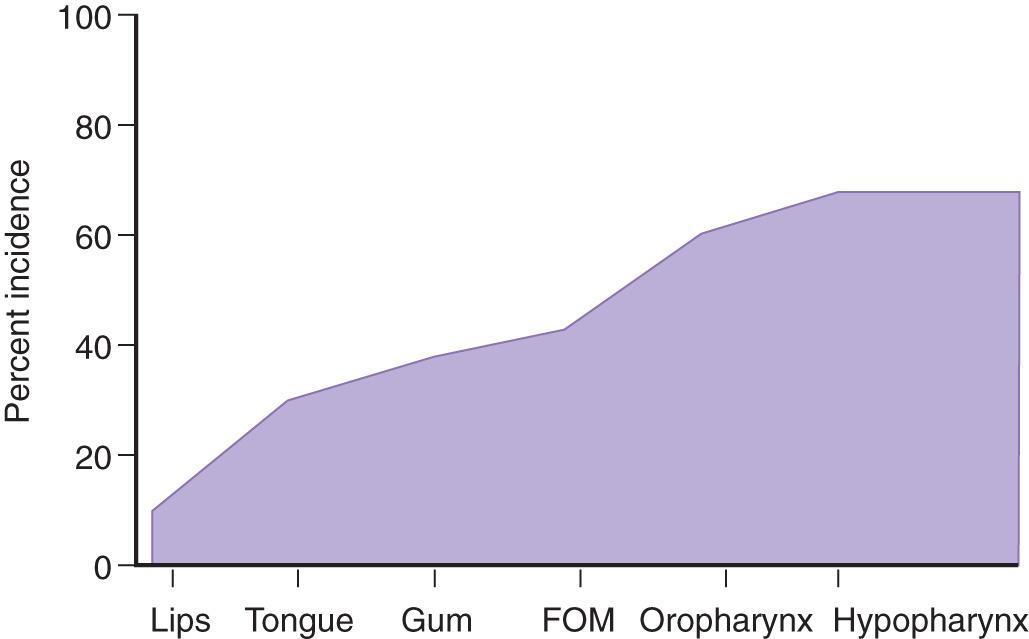
One of the most important factors affecting prognosis for patients with squamous cell carcinoma of the upper aerodigestive tract is the status of cervical lymph nodes at the time of presentation. The presence of nodal metastasis reduces survival by nearly 50% in nearly all squamous cell carcinomas of the upper aerodigestive tract ( Fig. 11.1 ). The exceptions to this are cancers of the nasopharynx and human papillomavirus (HPV)–associated oropharynx cancer, in which presence of ipsilateral lymph node metastasis does not have the same negative prognostic value. In spite of the progress in early detection and advances in imaging techniques during the past few decades, a significant number of patients still present with disease at an advanced stage. Reports from the American Cancer Society indicate that, in the United States, more than 40% of the patients with squamous cell carcinomas of the oral cavity and pharynx present with regional dissemination of disease at the time of initial diagnosis ( Fig. 11.2 ). In other parts of the world, such as South Asia and Latin America, a larger proportion of patients with cancer of the upper aerodigestive tract present with advanced stage disease. Therefore the management of cervical lymph nodes becomes a vitally important component in the overall treatment strategy for patients with cancers of the head and neck. Regional lymphatic drainage from the scalp and skin of the head and neck region, the mucosa of the upper aerodigestive tract, the paranasal sinuses, the salivary glands, and the thyroid gland is well defined, and metastasis from cancers in these locations occurs in a sequential and predictable manner to specific regional lymph nodes. As such, understanding the risk and patterns of metastasis for each primary site is essential in planning treatment.
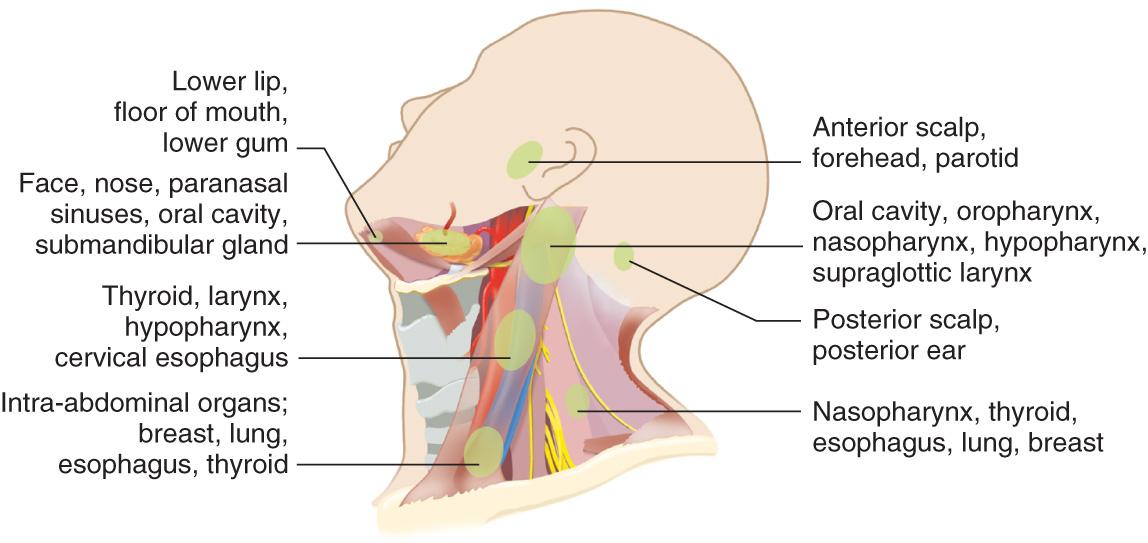
The lymphatic network of the head and neck area is located in two layers separated by the deep cervical fascia. The superficial lymphatics drain into suboccipital, preauricular and postauricular, prevascular facial, and external jugular lymph nodes. These lymph nodes eventually drain into the deep jugular lymph nodes. The major lymph node groups of the head and neck region are shown in Fig. 11.3 . The preauricular, periparotid, and intraparotid lymph nodes are the first-echelon lymph nodes for the anterior half of the scalp, the skin of the forehead, and the upper part of the face. The postauricular and suboccipital groups of lymph nodes provide drainage from the posterior half of the scalp and the posterior aspect of the external ear. Deep cervical lymph nodes in the lateral aspect of the neck primarily drain from the mucosa of the upper aerodigestive tract. These lymph nodes include the submental, prevascular facial, and submandibular group located in the submental and submandibular triangles of the neck. Deep jugular lymph nodes include the jugulodigastric, juguloomohyoid, and supraclavicular group of lymph nodes adjacent to the internal jugular vein. Lymph nodes in the posterior triangle of the neck include the accessory chain located along the spinal accessory nerve and the transverse cervical chain in the floor of the posterior triangle of the neck. Lymphatics of the pharynx also drain into the parapharyngeal and retropharyngeal lymph nodes.
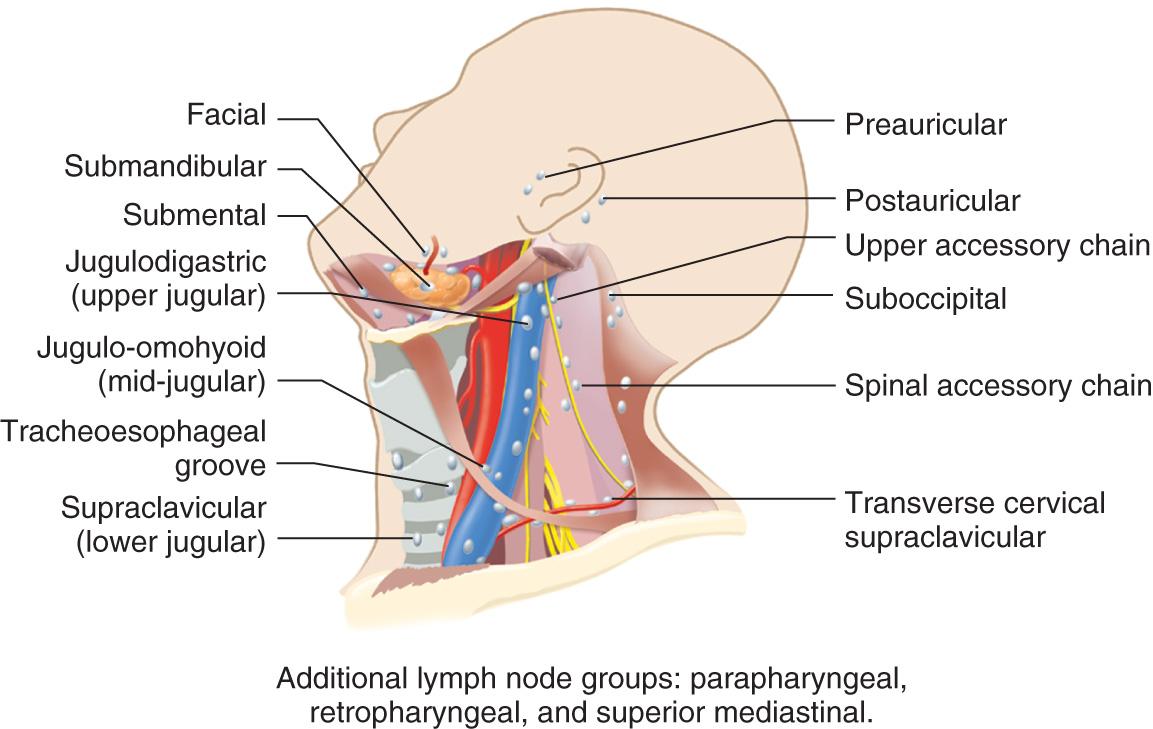
The central compartment of the neck includes the Delphian lymph node overlying the thyroid cartilage in the midline, which drains from the larynx and thyroid gland, and the perithyroid lymph nodes, as well as the pretracheal, paratracheal, and paraesophageal lymph nodes. Lymphatics of the thyroid gland, hypopharynx, subglottic larynx, and cervical esophagus drain into the paratracheal lymph nodes. Lymph nodes in the anterosuperior mediastinum provide drainage from the thyroid gland and the cervical esophagus and serve as a secondary lymphatic basin for central compartment viscera. Each previously described anatomic subgroup of lymph nodes serve as primary-echelon lymph nodes that drain from a specific site in the head and neck region. Thus the location of a palpable metastatic lymph node often may indicate the potential site of a primary tumor ( Fig. 11.4 ).
The conventional description of regional nodes is based on the leveling system first proposed from the Head and Neck Service at Memorial Sloan Kettering Cancer Center in New York nearly a century ago ( Fig. 11.5 ). This system divides the lymph nodes in the lateral aspect of the neck into five nodal groups or levels. In addition, lymph nodes in the central compartment of the neck are assigned level VI, and those in the anterosuperior mediastinum are assigned level VII.
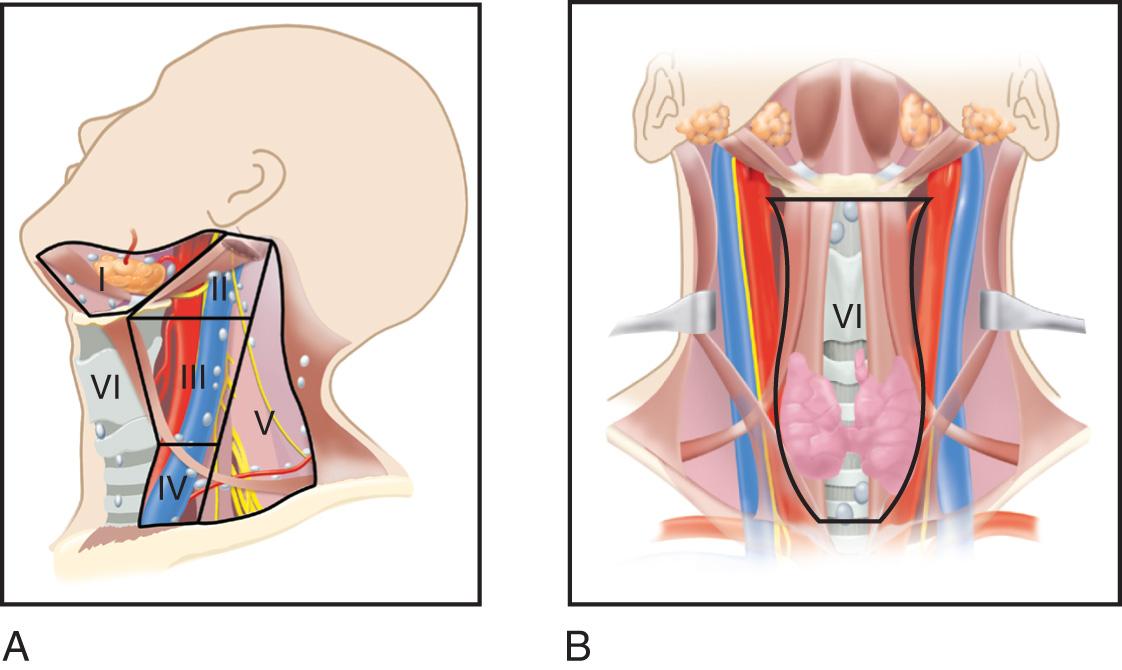
The American Academy of Otolaryngology-Head and Neck Surgery has modified the above system by subdividing levels I, II, and V into A and B categories for each of these levels ( Fig. 11.6 ).
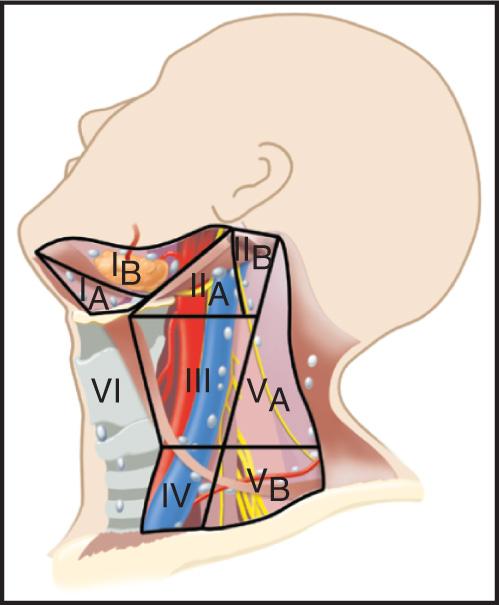
The submental group or level I (IA) includes the lymph nodes between the anterior bellies of the digastric muscles from the lower border of the symphysis of the mandible cephalad to the hyoid bone caudad. The submandibular group or level I (IB) includes lymph nodes in the triangular area bounded by the anterior and posterior bellies of the digastric muscle and the inferior border of the body of the mandible. The lymph nodes adjacent to the submandibular salivary gland and along the facial artery (prevascular facial) are included in this group.
Level II is the upper jugular group, which includes lymph nodes around the upper third of the internal jugular vein and the upper part of the spinal accessory nerve, extending from the base of the skull up to the bifurcation of the carotid artery or to the level of the hyoid bone. The posterior limit for this level is the posterior border of the sternocleidomastoid muscle, and the anterior limit is the lateral border of the sternohyoid muscle. Lymph nodes anterior to the spinal accessory nerve are designated level IIA, and those posterior to it are designated level IIB.
Level III is the midjugular group, which includes lymph nodes around the middle third of the internal jugular vein from the hyoid bone up to the inferior border of cricoid cartilage. The anterior and posterior borders are the same as those for level II.
Level IV is the lower jugular group, which includes lymph nodes around the lower third of the internal jugular vein from the inferior border of cricoid cartilage up to the clavicle. The anterior and posterior borders are the same as those for levels II and III.
Level V is the posterior triangle group, which includes lymph nodes around the lower portion of the spinal accessory nerve and along the transverse cervical vessels. It is bounded by the triangle formed by the clavicle, the posterior border of the sternocleidomastoid muscle, and the anterior border of the trapezius muscle. Level V is divided into two levels by a plane at the level of the inferior border of the cricoid cartilage. Level VA is superior to this plane, and level VB is inferior to it. Generally, level VA includes accessory chain lymph nodes and level VB includes transverse cervical chain and supraclavicular lymph nodes.
Level VI is the central compartment group, which includes lymph nodes in the prelaryngeal, (Delphian), pretracheal, paratracheal, and tracheoesophageal groove. The boundaries are the hyoid bone cephalad to the suprasternal notch caudad and between the medial borders of the carotid sheaths.
Level VII is the anterosuperior mediastinal group, which includes lymph nodes in the anterosuperior mediastinum and tracheoesophageal grooves, extending from the suprasternal notch to the innominate artery.
Dissemination of metastatic cancer to regional lymph nodes from primary sites in the upper aerodigestive tract occurs in a predictable and sequential fashion. Thus only a select group of lymph nodes are at risk of initial metastases from a given primary site. Understanding the sequential patterns of neck metastasis greatly facilitates surgical management of regional lymph nodes in the clinically negative neck (N0), but if the lymph nodes are at risk of harboring micrometastasis.
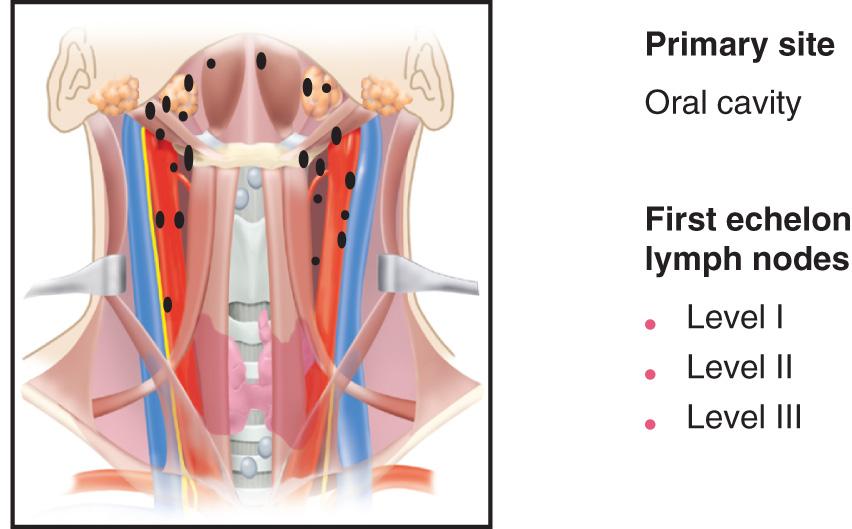
For primary tumors in the oral cavity, the regional lymph nodes at highest risk for early dissemination by metastatic cancer are limited to levels I, II, and III ( Fig. 11.7 ). Anatomically, this translates into regional lymph node groups contained within the supraomohyoid triangle of the neck bounded superiorly by the lower border of the mandible, posteriorly by the posterior border of the sternocleidomastoid muscle, and anteriorly by the superior belly of the omohyoid muscle, and which includes the submental triangle. The following lymph node groups are contained in the supraomohyoid triangle: submental, submandibular, prevascular facial, jugulodigastric, upper deep jugular, superior spinal accessory chain of lymph nodes, and midjugular lymph nodes. Skip metastasis to levels IV and V in the absence of metastatic disease at levels I, II, or III is exceedingly rare. Therefore if findings of the neck are clinically negative, level IV and V lymph nodes generally are not at risk of harboring micrometastasis from primary squamous cell carcinomas of the oral cavity. Primary carcinomas of the lateral border of the tongue has a somewhat higher risk of involvement of lymph nodes at level IV, particularly if there is already metastatic disease present at levels II or III.
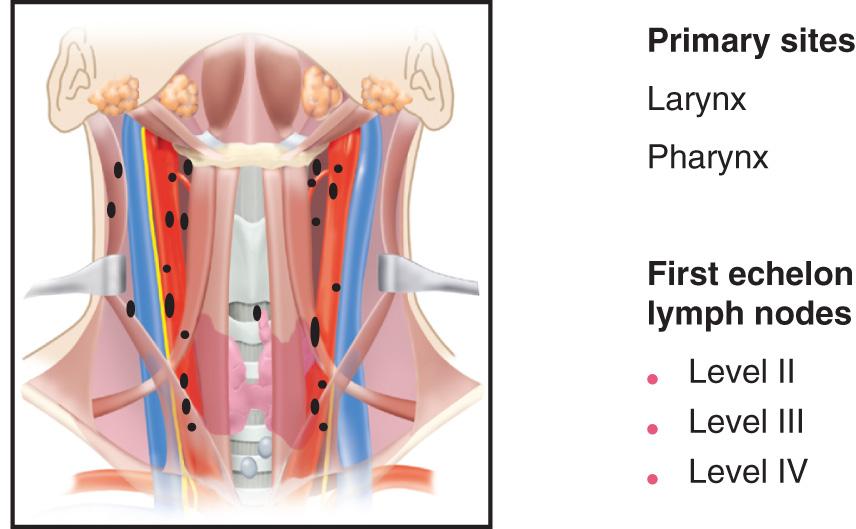
For tumors of the lateral aspect of oropharynx, hypopharynx, and larynx, the first-echelon lymph nodes at highest risk of harboring micrometastasis in the clinically negative neck are the deep jugular lymph nodes at levels II, III, and IV on the ipsilateral side ( Fig. 11.8 ). Contiguous lymph nodes lateral to the internal jugular vein overlying the cutaneous roots of the cervical plexus usually are considered a component of levels II, III, and IV. In patients with primary carcinomas of the oropharynx, hypopharynx, and larynx who have clinically negative neck, the risk of micrometastasis to levels I and V is exceedingly small. Skip metastasis to levels I and V in the absence of disease at levels II, III, or IV usually is not seen. Primary tumors that involve both sides of the midline in these primary sites have a potential risk of microscopic dissemination of metastatic disease to jugular lymph nodes on both sides of the neck. Similarly, tumors of the medial wall of the pyriform sinus are reported to have an increased risk of contralateral neck metastases.
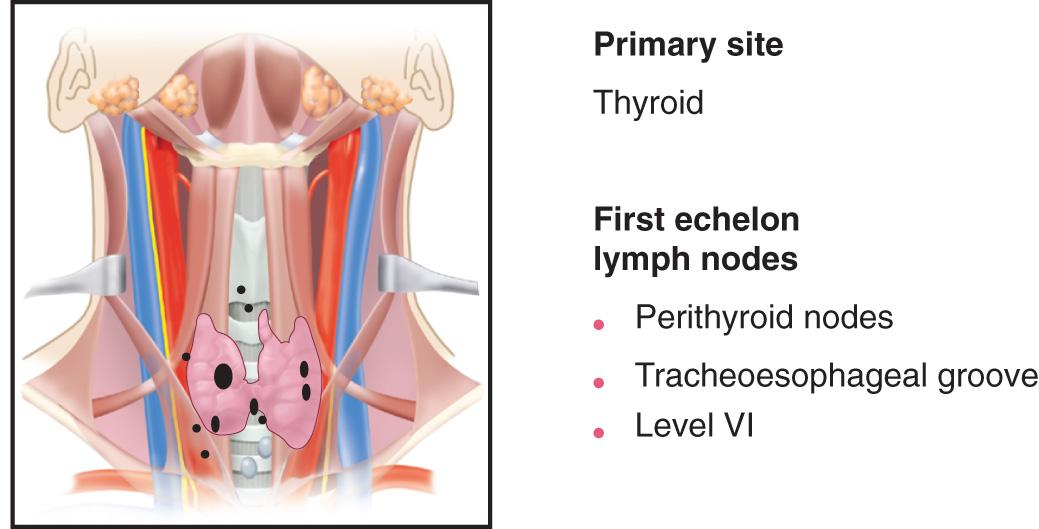
Regional lymph node metastases from primary differentiated carcinomas of the thyroid gland occur in an occult manner in a high proportion of patients (approximately 50%), although clinically gross metastases at initial presentation are infrequent. The first-echelon lymph nodes at highest risk for metastases from a primary differentiated carcinoma of the thyroid gland are those adjacent to the thyroid gland, the so-called perithyroid lymph nodes, and those in the tracheoesophageal groove and superior mediastinum ( Fig. 11.9 ). Metastatic disease sequentially progresses from the central compartment lymph nodes to lower, middle, and upper jugular lymph nodes. Lymph nodes in the posterior triangle of the neck are involved infrequently unless there is gross metastatic disease at level IV, where contiguous metastatic spread to level VB is not uncommon. Metastatic disease from a primary carcinoma of the thyroid to level I is exceedingly rare.
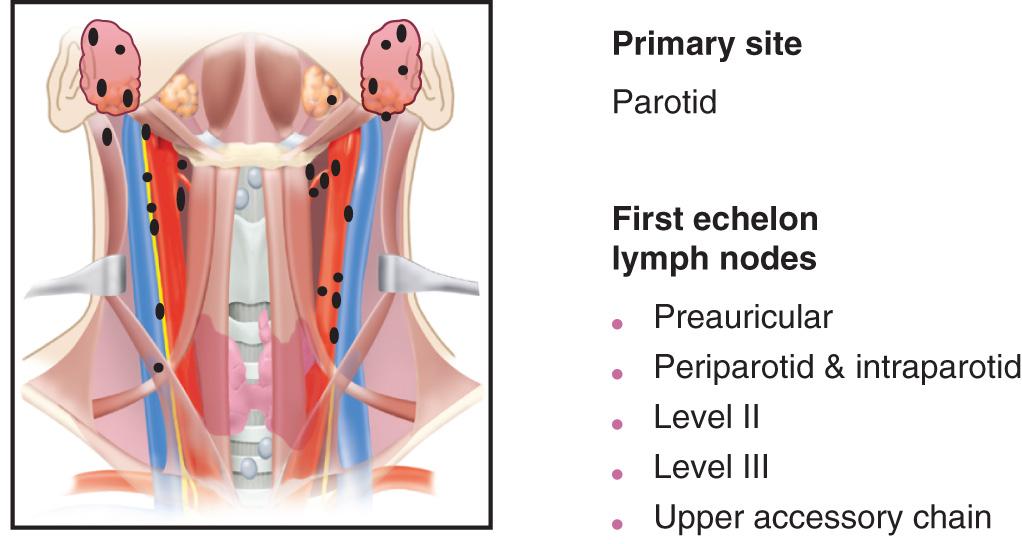
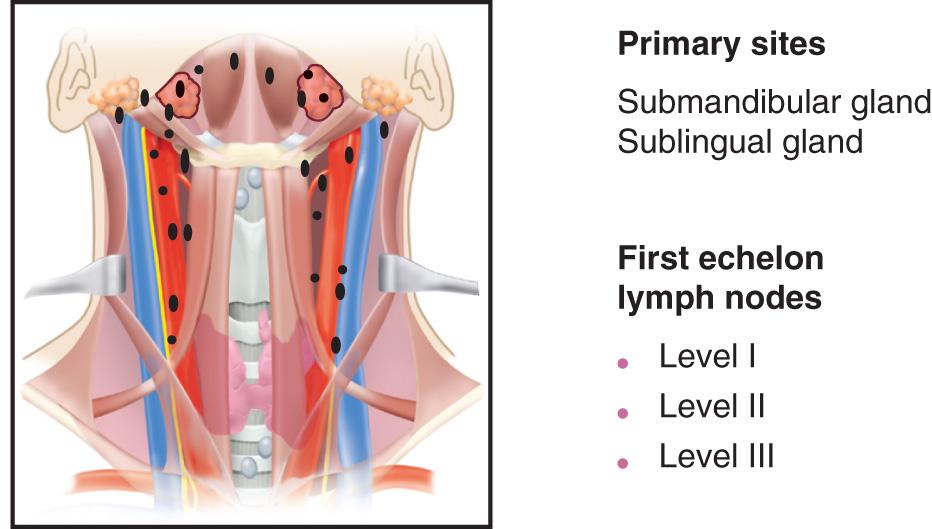
Regional lymph node metastasis develops in only 20% to 25% of patients with a carcinoma of the parotid gland. The lymph node groups at highest risk for metastases from a primary carcinoma of the parotid gland are those in the preauricular, periparotid, and intraparotid regions, as well as lymph nodes in the upper deep jugular chain and those in the upper spinal accessory chain in the posterior triangle of the neck ( Fig. 11.10 ). Initial dissemination of metastatic cancer from primary malignant tumors of the submandibular salivary gland occurs to lymph nodes in the supraomohyoid triangle ( Fig. 11.11 ).
Cutaneous malignant tumors of the scalp also spread to regional lymph nodes in a predictable fashion. A line joining the helix of one ear to the helix of the opposite ear in a coronal plane separates the watershed areas of the scalp. Tumors located anterior to this line in general metastasize to preauricular, periparotid, and anterior cervical lymph nodes (levels I to IV) and seldom metastasize to the posterior triangle of the neck. On the other hand, primary tumors of the scalp posterior to this line metastasize to the suboccipital and postauricular group of lymph nodes as well as those in the posterior triangle of the neck and the deep jugular chain (levels II to V).
The risk for metastasis to regional lymphatics from primary squamous cell carcinomas of the upper aerodigestive tract depends on the primary site, T stage, and histomorphologic features of the primary tumor. In general, the risk of nodal metastasis increases from the anterior to posterior aspect of the upper aerodigestive tract, that is, the lips, oral cavity, oropharynx, and hypopharynx ( Fig. 11.12 ). For tumors of the larynx and pharynx, the risk of nodal metastasis increases with progression from the center of the upper aerodigestive tract (the vocal cords) to the periphery (the lateral pharyngeal wall). For example, the risk of regional lymph node metastasis from a carcinoma of the true vocal cords is exceedingly small. However, the risk increases with progression from the vocal cords to the false vocal cords, aryepiglottic fold, pyriform sinus, and pharyngeal wall. Nearly two-thirds of patients with primary carcinomas of the hypopharynx present with clinically palpable regional lymph node metastasis.
The T stage usually reflects tumor burden or invasiveness and is correlated with risk for nodal metastasis for any given primary site. Overall, the risk for metastasis is less than 15% for T1, 15% to 30% for T2, 30% to 50% for T3, and up to 75% for T4 head and neck primary squamous cell carcinomas. Certain histomorphologic features of the primary tumor also increase the risk of nodal metastasis. The risk of nodal metastases from HPV-positive oropharynx cancer is disproportionately high, even with a low T stage of the primary tumor. Endophytic tumors have a higher risk for metastasis compared with exophytic tumors. This is particularly true for primary carcinomas of the oral cavity (tongue and floor of mouth), where there is increasing risk of nodal metastases, with increasing depth of invasion (DOI). The AJCC and UICC have therefore revised the T staging of primary squamous cell carcinomas of the oral cavity, where each 5 mm increase in DOI will upstage the tumor by one T stage. Poorly differentiated carcinomas have a higher risk of nodal metastases compared with well-differentiated lesions. The pattern of invasion also has been shown to affect risk for metastasis. However, the influence of these parameters is not independent of T stage based on multivariate analysis. Only DOI has been shown to be an independent predictor of the risk for nodal metastases for cancers of the tongue and floor of the mouth. Metastatic spread from primary carcinomas of salivary origin is generally low (approximately 20%). The risk depends on the histology, grade, and stage of the primary tumor. Similarly, most head and neck sarcomas have a very low risk for regional metastasis with the exception of rhabdomyosarcoma, epithelioid sarcoma, synovial sarcoma, and angiosarcoma. Unlike other head and neck malignancies, even though the risk for dissemination to regional lymph nodes from differentiated carcinomas of the thyroid (papillary) is quite high (approximately 50% of occult metastases), elective dissection of regional lymph nodes is not recommended because it does not have an adverse impact on prognosis in a majority of patients who fall into the low-risk group stratification.
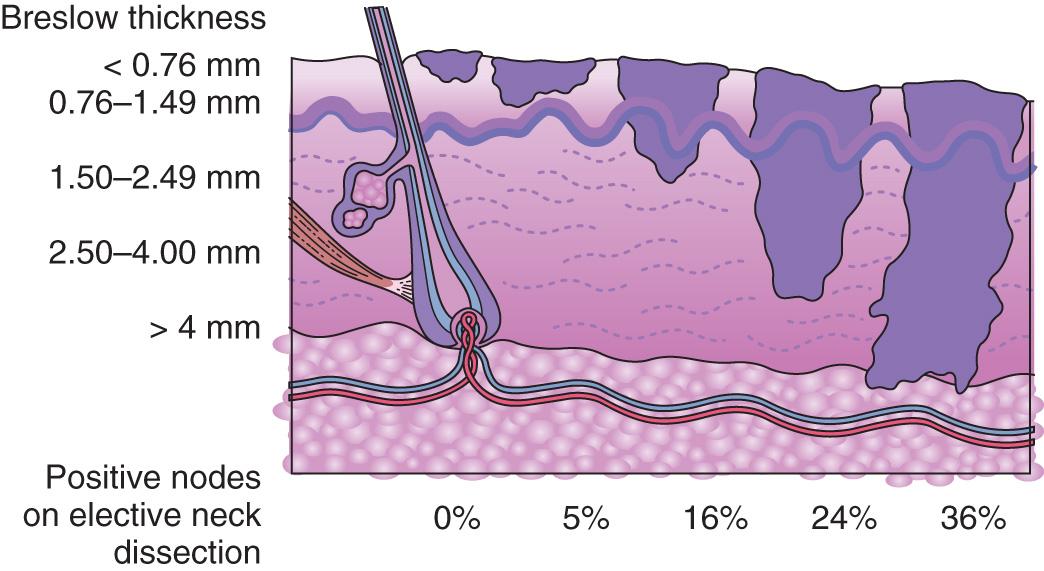
Risk of nodal metastases from cutaneous malignancies is relatively low. Basal cell carcinomas have a very low risk for metastasis (<1%), whereas the risk can be as high as 10% for cutaneous squamous cell carcinomas. Larger cutaneous squamous cell carcinomas (>2 cm) and those with adverse pathologic features (i.e., poor differentiation, DOI of >6 mm, and perineural invasion) have a higher risk for metastases. Once metastases develop from a cutaneous malignancy, the probability of survival decreases by up to 90%. On the other hand, cutaneous tumors of neuroendocrine origin (e.g., Merkel cell carcinoma and malignant melanoma) have a much higher risk for regional metastasis. For Merkel cell carcinomas larger than 1 cm, the risk of nodal metastases is 20% or more. The risk for nodal metastasis for cutaneous melanomas is related to tumor thickness and is higher for tumors thicker than 1 mm ( Fig. 11.13 ). Adnexal tumors of the skin rarely metastasize with the exception of sebaceous and eccrine gland carcinomas.
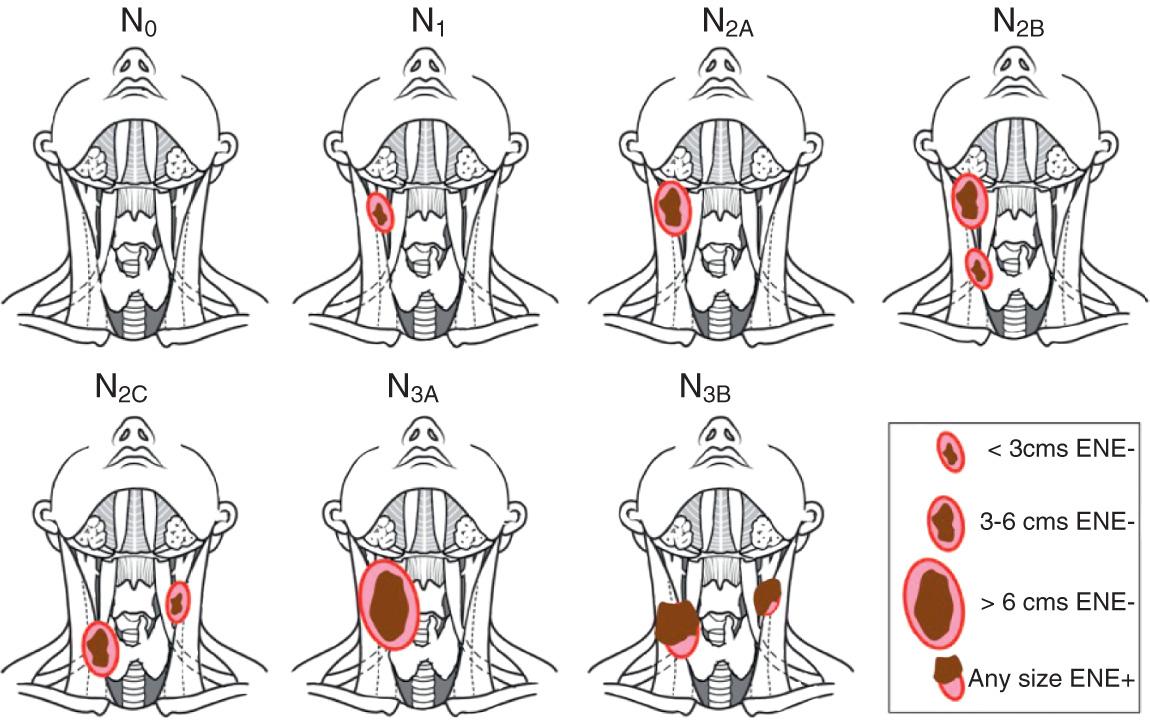
The American Joint Committee on Cancer and the International Union Against Cancer have agreed upon a uniform staging system for cervical lymph nodes. The site, number, size, and extranodal extension (ENE) are the most important factors considered in nodal staging of most squamous cell carcinomas of the head and neck. The presence of clinical evidence of ENE has such an important negative prognostic impact that any lymph node with clinical or radiologic evidence of ENE gets upstaged to N3B category. ENE can be diagnosed clinically by the presence of a matted mass of nodes fixed to the overlying skin or adjacent soft tissue or clinical signs of cranial nerve invasion. Radiologic signs of ENE include amorphous, spiculated margins of a metastatic node and stranding of the perinodal soft tissue in previously untreated patients. The exact description of each clinical N stage of lymph node metastases from squamous cell carcinomas of the head and neck (oral cavity, HPV-negative oropharynx, hypopharynx, larynx, paranasal sinuses, salivary glands, and nonmelanoma skin cancers of the head and neck) is shown in Fig. 11.14 and Table 11.1 . Squamous cell carcinomas of the nasopharynx, HPV-positive cancers of the oropharynx (OPC), and well-differentiated thyroid carcinomas have a different biology, and cervical metastases from these tumors are assigned different staging systems. The natural history and response to treatment of cervical nodal metastases from nasopharynx and HPV-positive oropharynx primary sites are different in terms of their impact on prognosis, so they justify a different N classification scheme. For the nasopharynx, the size and location of the metastatic node(s) are important parameters ( Table 11.2 ). For HPV-positive OPC only the size of the metastatic nodes are considered in staging ( Table 11.3 ). Regional node metastases from well-differentiated thyroid cancer do not significantly affect the ultimate prognosis in a majority of patients (approximately 80%) who fall in the low-risk group category and therefore also justify a unique staging system. Staging for nodal metastases from differentiated thyroid carcinoma is largely based on the location of the metastases ( Table 11.4 ).
| N CATEGORY | N CRITERIA |
|---|---|
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Metastasis in a single ipsilateral lymph node, 3 cm or smaller in greatest dimension ENE(−) |
| N2 | Metastasis in a single ipsilateral node larger than 3 cm but not larger than 6 cm in greatest dimension and ENE(−); or metastases in multiple ipsilateral lymph nodes, none larger than 6 cm in greatest dimension and ENE(−); or in bilateral or contralateral lymph nodes, none larger than 6 cm in greatest dimension, and ENE(−) |
| N2a | Metastases in a single ipsilateral node larger than 3 cm but not larger than 6 cm in greatest dimension, and ENE(−) |
| N2b | Metastasis in multiple ipsilateral nodes, none larger than 6 cm in greatest dimension, and ENE(−) |
| N2c | Metastasis in bilateral or contralateral lymph nodes, none larger than 6 cm in greatest dimension, and ENE(−) |
| N3 | Metastasis in a lymph node larger than 6 cm in greatest dimension and ENE(−); or metastasis in any node(s) and clinically overt ENE(+) |
| N3a | Metastasis in a lymph node larger than 6 cm in greatest dimension and ENE(−) |
| N3b | Metastasis in any node(s) and clinically overt ENE(+) |
| N CATEGORY | N CRITERIA |
|---|---|
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Unilateral metastasis in cervical lymph node(s) and/or unilateral or bilateral metastasis in retropharyngeal lymph node(s), 6 cm or smaller in greatest dimension, above the caudal border of cricoid cartilage |
| N2 | Bilateral metastasis in cervical lymph node(s), 6 cm or smaller in greatest dimension, above the caudal border of cricoid cartilage |
| N3 | Unilateral or bilateral metastasis in cervical lymph node(s), larger than 6 cm in greatest dimension, and/or extension below the caudal border of cricoid cartilage |
| N CATEGORY | N CRITERIA |
|---|---|
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | One or more ipsilateral lymph nodes, none larger than 6 cm |
| N2 | Contralateral or bilateral lymph nodes, none larger than 6 cm |
| N3 | Lymph node(s) larger than 6 cm |
| N CATEGORY | N CRITERIA |
|---|---|
| NX | Regional lymph nodes cannot be assessed |
| N0 | No evidence of locoregional lymph node metastasis |
| N0a | One or more cytologically or histologically confirmed benign lymph nodes |
| N0b | No radiologic or clinical evidence of locoregional lymph node metastasis |
| N1 | Metastasis to regional nodes |
| N1a | Metastasis to level VI or VII (pretracheal, paratracheal, or prelaryngeal/Delphian, or upper mediastinal) lymph nodes; this can be unilateral or bilateral disease |
| N1b | Metastasis to unilateral, bilateral, or contralateral lateral neck lymph nodes (levels I, II, III, IV, or V) or retropharyngeal lymph nodes |
The American Joint Committee on Cancer and the International Union Against Cancer have developed a separate pathologic staging (pN) for those tumors primarily treated surgically, and where a pathologic specimen is available for accurate assessment of the extent of nodal metastases. For example even microscopic ENE (<2 mm) is considered as ENE(+), and thus entered into upstaging N category. This nodal staging is different than cN staging and offers more accurate information for overall pN staging of these cancers. Thus pN staging is often used for adjuvant treatment planning as well as for more accurate assessment of prognosis. The pN staging for oral cavity, HPV-negative oropharynx, hypopharynx, larynx, paranasal sinuses, salivary glands, and nonmelanoma skin cancers of the head and neck is shown in Table 11.5 . The pN staging for HPV-positive oropharynx cancers is shown in Table 11.6 . There is no pN staging developed for cancers of the nasopharynx and differentiated cancers of the thyroid gland.
| N CATEGORY | N CRITERIA |
|---|---|
| NX | Regional lymph nodes cannot be assessed. |
| N0 | No regional lymph node metastasis |
| N1 | Metastasis in a single ipsilateral lymph node, 3 cm or smaller in greatest dimension and ENE(−) |
| N2 | Metastasis in a single ipsilateral lymph node, 3 cm or smaller in greatest dimension and ENE(+); or larger than 3 cm but not larger than 6 cm in greatest dimension and ENE(−); or metastasis in multiple ipsilateral lymph nodes, none larger than 6 cm in greatest dimension, ENE(−) |
| N2a | Metastasis in a single ipsilateral or contralateral node 3 cm or smaller in greatest dimension and ENE(+); or a single ipsilateral node larger than 3 cm but not larger than 6 cm in greatest dimension and ENE(−) |
| N2b | Metastasis in multiple ipsilateral nodes, none larger than 6 cm in greatest dimension and ENE(−) |
| N2c | Metastasis in bilateral or contralateral lymph nodes, none larger than 6 cm in greatest dimension and ENE(−) |
| N3 | Metastasis in a lymph node larger than 6 cm in greatest dimension and ENE(−); or in a single ipsilateral node larger than 3 cm in greatest dimension and ENE(+); or multiple ipsilateral, contralateral, or bilateral nodes any with ENE(+) |
| N3a | Metastasis in a lymph node larger than 6 cm in greatest dimension and ENE(−) |
| N3b | Metastasis in a single ipsilateral node larger than 3 cm in greatest dimension and ENE(+); or multiple ipsilateral, contralateral, or bilateral nodes any with ENE(+) |
| N CATEGORY | N CRITERIA |
|---|---|
| NX | Regional lymph nodes cannot be assessed |
| pN0 | No regional lymph nodes metastasis |
| pN1 | Metastasis in 4 or fewer lymph nodes |
| pN2 | Metastasis in more than 4 lymph nodes |
The pattern of the lymphatic drainage varies for different anatomic sites. However, the location of the lymph node metastases has prognostic significance in patients with squamous cell carcinoma of the head and neck. Survival is significantly worse when metastases involve lymph nodes beyond the first echelon of lymphatic drainage and, particularly, lymph nodes in the lower parts of the neck, i.e., level IV and level VB (supraclavicular region). Therefore the AJCC recommends that each N staging category be recorded on the staging forms to show whether the nodes involved are located in the upper (U) or lower (L) regions of the neck, depending on their location above or below the lower border of the cricoid cartilage.
When enlarged lymph nodes are detected, the actual size of the nodal mass(es) should be measured. It is recognized that most masses over 3 cm in diameter are not single nodes but are confluent nodes or tumor in soft tissues of the neck. Careful clinical examination; radiologic assessment; and, in surgically treated patients, detailed pathologic examination is necessary for documentation of tumor extent in terms of the location or level of the lymph node(s) involved, the number of nodes that contain metastases, and the presence or absence of ENE.
Involvement of lower cervical lymph nodes (levels IV and VB) by metastatic cancer usually is ominous. Lymph node density, which reflects tumor factors (number of positive lymph nodes), treatment factors (number of lymph nodes removed during neck dissection), and staging factors (completeness of the sampling procedure, including those related to the surgeon and pathologist) has been found to stratify risk of local regional recurrence and survival. Lymphovascular invasion (LVI) and perineural invasion (PNI) by a tumor, as well as the presence of tumor emboli in regional lymphatics, also has an adverse impact on prognosis. Therefore these factors must be considered when developing a treatment strategy for patients in whom regional lymph nodes are involved by metastatic disease, particularly for planning adjuvant therapy and in the assessment of prognosis.
Assessment and management of patients with head and neck primary tumors presenting with regional lymphatic metastasis can be divided into those with clinically detectable metastasis and those at risk of harboring occult metastasis. The approach to management of these two clinical scenarios is defined by patterns and risk of regional spread.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here