Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
© 2018 Elsevier Inc. All rights reserved. Please note that the copyright for the original figures submitted by the contributors is owned by Contributors.
Chordomas and chondrosarcomas are malignant tumors whose gross total resection significantly increases the overall survival. They are locally invasive; as they breach normal anatomic planes, chordomas and chondrosarcomas may encroach upon or encase major cerebral blood vessels. Cerebral revascularization becomes necessary when critical blood vessels are irreparably injured during tumor removal, when resection of an encased internal carotid artery (ICA) or vertebral artery (VA) is indicated oncologically in an attempt to resect all tumor, or to reduce the risk of ICA pseudoaneurysm and rupture by rerouting the artery away from exposure to nasopharyngeal infection resulting from surgical exposure or tumor invasion.
Thorough preoperative medical and cardiac evaluation is important because the pharmacological agents used to induce temporary metabolic suppression and hypertension for brain protection during interruption of some cerebral blood flow during revascularization can stress the heart. Patients for whom cerebral revascularization is planned or is a possibility are maintained on aspirin 325 mg prior to surgery.
Patients undergo computed tomographic (CT) scan, magnetic resonance imaging, and noninvasive (CT or magnetic resonance–based) angiography to reveal the basic characteristics and extent of the tumor. Tumor encasement of a major cerebral artery warrants catheter digital subtraction angiography with balloon occlusion testing. This allows careful assessment of the vascular anatomy of the involved vessel, of its communicating arteries and the relevant collateral circulation, of the size and morphology of potential intracranial recipient vessels for a bypass, and of the extracranial vessels—including the cervical ICA, external carotid artery (ECA), superficial temporal artery, and occipital artery (OA)—that may be used as donor vessels. Doppler ultrasonography, also, is used to evaluate the diameter, length, and course of peripheral vessels that may be used for bypass grafting. For high-flow bypasses, the order of preference is radial artery (RA) > saphenous vein > anterior tibial artery. The larger caliber saphenous vein provides the highest flow, but radial arteries are easier to suture to intracranial vessels. The problem of vasospasm of the radial artery grafts (RAGs) has been greatly reduced by the pressure distension technique, first described by Sekhar et al. A Doppler ultrasound Allen test should be performed to assess the patency of the palmar arch in determining the safety of RA harvest. Optimal diameters for grafting are >0.22 mm for RA and >0.3 mm for the saphenous vein. The vein or artery harvested for an intracranial (external carotid–internal carotid (EC–IC)) bypass should be at least 20 mm long.
Reconstructive procedures can be classified as local bypasses and EC–IC bypasses. Local bypasses consist of (1) reimplantation (end to side), (2) end-to-end restructure, (3) side-to-side anastomosis, and (4) short interposition graft. All use intracranial arteries and can effectively replace small and medium arteries.
There are three types of extra- to intracranial bypasses. (1) Low-flow bypasses, e.g., superficial temporal to middle cerebral artery (MCA) bypass, OA to posterior inferior cerebellar artery (PICA) bypass, etc., usually provide flows less than 50 cc/min. acutely; (2) High-flow bypasses (more than 100 cc/min of flow) include RAG and grand saphenous vein graft (SVG); these are usually used for large vessel replacement, such as the ICA and basilar artery; and (3) Moderate-flow bypasses (60–80 cc/min.) are predominantly RAGs used in posterior circulation ( Table 21.1 ).
| Type of Bypass | Flow (cc/min) | Examples | Indications |
|---|---|---|---|
| Low-flow bypasses | ≤50 | STA to MCA, OA to PICA, etc. | Medium/small vessel replacement |
| High-flow bypasses | ≥100 | RAG and SVG | Large vessel replacement |
| Moderate-flow bypasses | 60–80 | RAG | Posterior circulation |
The choice of graft depends upon four factors: (1) size of the recipient vessel, the major determinant; (2) availability of an adequate donor vessel; (3) availability of graft material; and (4) the augmentation of blood flow required. The bypass blood flow immediately after superficial temporal artery-middle cerebral artery (STA-MCA) anastomosis is 20–60 mL/min. The average flow through RAGs is 133 ± 70 mL/min and through SVGs it is 160 ± 50 mL/min. The flow rate depends on the donor vessel, the recipient vessel, the flow demand, and the diameter of the graft. For RAGs, for each 1 mm increase of diameter, the flow rate increases by 33 mL/min.
SVGs provide the largest volume of flow, but the potential for turbulence leading to occlusion at the anastomotic sites (especially recipient) and for hyperemia and hemorrhage in chronically ischemic brain is a potential drawback. The risk of hyperemia is increased when the flow rate exceeds 200 mL/min. On the other hand, the low-flow STA-MCA anastomosis may not provide flow adequate to prevent a stroke in cases of acute ICA occlusion with poor or no collaterals. Although vasospasm in RAG grafts is usually prevented by pressure distension, occasionally endovascular angioplasty is needed.
EC–IC bypass is the most commonly employed revascularization technique used in resecting skull base chordomas and chondrosarcomas. RAG is used when some collateral circulation is present, the recipient vessel is not large enough (≥2 mm), or moderate increase or replacement of flow are required. The volume of flow increases with the actual diameter of the RAG. An SVG is used if a very high-flow replacement is needed. Alternatively, two bypasses may be created. After incidental arteriotomy during tumor resection, proximal and distal control of the arteriotomy site should be secured and direct suture repair attempted. If direct repair is unsuccessful, then local reconstruction is performed if feasible given the location and nature of the arterial injury. Examples include MCA branch reimplantation, MCA branch repair, anterior cerebral artery-to-anterior cerebral artery or PICA-to-PICA side-to-side anastomosis. When direct repair is precluded by the length of the gap, a short interposition graft using the STA, OA, or superior thyroid artery (SThyA) can be utilized. Less commonly, an STA-MCA or OA-MCA anastomosis is used if the blood flow requirement is small and the vessel being replaced is a small one, such as the PICA.
A prophylactic antibiotic, usually ceftriaxone, 1 g, is administered intravenously 1 h prior to the incision and repeated after 6 h in case the operation is prolonged. The patient is loaded with 1 g of fosphenytoin, and treatment is usually continued for a week. Administration of steroids is started on the morning of surgery or 24 h before surgery and continued postoperatively as needed. A balanced anesthetic technique is used. The patient is mildly hyperventilated (PaCO 2 around 30 torr) to reduce the intracranial pressure. Mannitol, at 0.5 to 1 g/kg body weight, is given intravenously at the time of skin incision. During temporary arterial occlusion, the blood pressure (BP) is raised 20% above the baseline, and the patient is placed in electroencephalographic (EEG) burst suppression using propofol. Neurophysiological monitoring consists of the somatosensory evoked potential (SEP), motor evoked potential (MEP), and EEG. Cranial nerve monitoring is also performed, depending on the specific extensions of the tumor and planned approach. Intraoperative indocyanine angiography (ICG angio) and micro-Doppler ultrasonography are used routinely. In many cases, these modalities provide sufficient detail to obviate intraoperative angiography. If intraoperative angiography is planned, femoral arterial access should be obtained prior to skin incision. Positioning should accommodate the likelihood of RAG or SVG harvest and the need for access to the cervical carotid arteries.
The reconstruction of cerebral arteries is usually performed after an inadvertent tear of a vessel wall. When the artery cannot be mobilized and sutured without tension, then a short interposition graft can be used. In some patients, section and reimplantation of a branch is possible. In all these situations, the operative technique is similar.
For direct reconstruction, the two arterial ends to be rejoined are sharply sectioned obliquely and slightly fish-mouthed at the opposing ends ( Fig. 21.1 ). A rubber dam is placed beneath the vessels, and temporary clips are positioned on both the vessels. The diametrically opposed ends are anchored with 9-0 or 10-0 nylon suture. Continuous sutures are placed on one side and continuous or interrupted sutures on the other side. Before the last suture is tied, the lumen is flushed with heparinized saline. Often, the artery cannot be flipped after one side is sutured, so the deeper side should be sutured first from the inside as with the side-to-side anastomosis technique and then the nearer side is sutured.
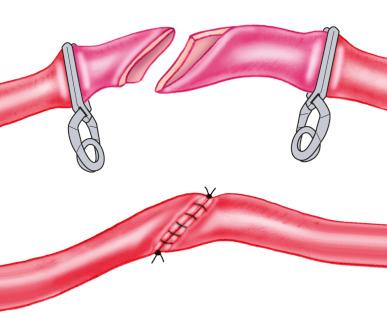
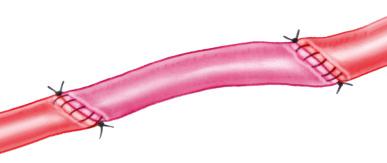
When the length of the gap between the two ends of the artery precludes approximation without tension, an arterial interposition graft is used. The grafts available for this purpose include the RA, STA, OA, and SThyA. The technique of suturing is similar to direct reconstruction ( Fig. 21.2 ).
Patient positioning takes into account the location of pathology, the donor and recipient vessel, and the site of graft extraction. Intraoperative angiography should be considered for large grafts. The patient’s head is fixed in a radiolucent head holder, the groin and thigh are prepared, and a femoral artery sheath is placed at the beginning if an intraoperative angiogram is considered. It can also be placed later in the case if needed. The graft extraction site should be prepared at the beginning, but in situations of unexpected emergency, preparation can also be done during the case.
A craniotomy alone may be adequate in some patients, but in most patients, a skull base approach is used to improve the exposure and to reduce brain retraction. Recipient vessel (vessels), donor vessel, and the graft are exposed, and a wide tunnel is created for the graft. The graft is extracted just before the anastomosis. The patient is placed in EEG burst suppression with pharmacological agents, and the systolic pressure is elevated 20% above baseline during vascular occlusion. For vein grafts and RAGs, 2500–3000 U of intravenous heparin is administered intravenously, just before the anastomosis is started. The recipient vessel is isolated, and the segment where the anastomosis is planned should be free of major perforators. The graft is adequately prepared and thoroughly flushed with heparinized saline. The graft end should be cut obliquely in an oval fashion. If needed, a fish-mouth opening is created by proximal spatulation. The distal anastomosis is performed first. Temporary clips of appropriate size are placed on the recipient vessel. Generally, the anastomosis time should be less than 45 min, and preferably less than 30 min, but for the posterior cerebral artery and superior cerebellar artery it can be as long as 50 min. The side of the recipient artery and the end of the graft vessel are marked with a pen. Following a small arteriotomy, an oval opening is created in the recipient vessel, usually about 1.5 to 2 times the diameter of the recipient artery. The graft is best oriented at a 45 degree angle (donor to recipient) for an end-to-side bypass. The suture thickness is chosen according to the thickness of the vessel wall. Usually 8-0 or 9-0 nylon is used for intracranial vessels, and the sutures are usually placed at the opposing ends of the arteriotomy first. This is usually followed by a running suture on the more difficult side, followed by running or interrupted, figure-of-8 sutures on the easier side. Care must be taken particularly near the ends to make sure that the suture includes both the intima and the media of the artery, and that only one wall is included in the suture. In placing the sutures near the ends, elevation of the wall of the recipient artery with a Rhoton 9 dissector facilitates correct placement of the suture. Specialized instruments are used to hold the arterial edges (long jeweler’s forceps, special titanium forceps), and special scissors are used to make cuts in the arteries and enlarge the opening, to hold and drive the needle (either straight, bayoneted, or pituitary style), and for tying the sutures. The steps follow the same sequence for the intracranial anastomosis and should be practiced by the surgeon and the assistant in the cadaver laboratory. The scrub nurse, the circulator, and the anesthesiologist should all be familiar and comfortable with their team roles during the operation. The neurophysiologist should alert the surgeon and anesthesiologist of any changes in the SEP or MEP during clamping. Such changes warrant BP elevation and blood volume expansion.
After the anastomosis is complete, the graft is flushed with heparinized saline before the last suture is tied. A temporary clip is placed on the graft, followed by the release of temporary clips on the recipient vessel. The graft is brought through the tunnel previously created and anastomosed to the donor artery. RA grafts may be brought to the neck through either the preauricular or postauricular tunnel. A preauricular tunnel can be created with a large chest tube (usually 14F size). For a postauricular tunnel, we make a skin incision just posterior to the site of the tunnel and connect the cervical and cranial incisions. For an SVG, a postauricular tunnel is preferred, as it allows orienting the graft parallel to the recipient MCA before it enters the cranium, which reduces turbulence in the graft. If the anastomosis of the SVG is to the supraclinoid ICA, then a preauricular tunnel is preferable. We also create a groove in the bone along the tunnel with the ultrasonic bone curette to allow more space for the graft to expand and to prevent compression by the skin superficial to it. If the patient wears glasses, one of the stems of the glasses must be taken out temporarily until the swelling subsides, to prevent compression by the plastic or metal stem.
Potential donor vessels include the ECA, the cervical ICA, the V2-V3 segment of the VA, the OA near the digastric groove, and the STA just inferior to the zygomatic process. The size of the donor vessel does limit the volume of flow into the graft. The anastomosis is either end to end or end (graft) to side (donor artery). When there is a disparity between the size of the graft and the donor vessel, an end-to-side anastomosis is preferred. For an end-to-side anastomosis, an oval hole, 3.5–4.5 mm in diameter, is created in the donor artery, usually with a vascular punch. This opening can be furthered if necessary. The anastomosis is usually sewn with 8-0 nylon or 7-0 Prolene running suture on one side, and interrupted, or figure-of-8 sutures, on the other side. Both vein grafts and RAGs expand on resumption of flow. As vein grafts expand more, they should be on slight stretch during the anastomosis. As the proximal and then distal clips are sequentially opened and the operator inspects for leaks and kinking. RA grafts are backbled to clear any air. Since this is not possible with vein grafts, any trapped air should be aspirated through a small branch or a small needle puncture site. Flow in the graft and the recipient vessel is confirmed with a micro-Doppler probe and an ICG angio. The dura mater is cut in circular fashion to allow unimpeded entry of the graft. An intraoperative angiogram, if needed to exclude obstruction by dura, is performed after dural closure. An opening in the bone flap is fashioned to accommodate graft without vessel kinking or tension. The graft is checked again with the Doppler probe after affixation of the bone flap.
For SVGs in particular, grooves are cut into the bone it overlies or penetrates to allow adequate space for the graft to expand in a pulsatile fashion. We always close the dura mater first, followed by neck wound closure (in the case of bypasses originating from the ECA or the ICA), replacement of the craniotomy flap, and skin closure. The graft is insonated each step of the way. If there is any concern, intraoperative angiography is needed to confirm graft patency.
Postoperative monitoring of graft patency usually consists of Doppler ultrasound evaluation every hour for 24 h. It should show a good diastolic flow, since systolic flow alone may be seen even when the graft is occluded. Any doubt regarding the functioning of the graft, should prompt cerebral angiography or magnetic resonance angiography (MRA). Patients are maintained on subcutaneous heparin, 5000 U every 8 h, for 1 week (in case of SVG). Aspirin, 325 mg once daily, is used for its antiplatelet effect, for life in the case of SVG and at least 6 weeks in the case of other grafts.
Long-term follow-up is performed annually with MRA or three-dimensional (3D) CT angiography.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here