Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Catecholaminergic polymorphic ventricular tachycardia (CPVT) is an inherited arrhythmia syndrome that is characterized by exercise or emotional stress–induced bidirectional or polymorphic ventricular tachyarrhythmias in patients with a normal electrocardiogram (ECG) at rest and in the absence of structural heart disease. Its prevalence in the general population is unknown but is estimated to be approximately 1 in 10,000. CPVT is a significant cause of sudden cardiac arrest (SCA) and sudden cardiac death (SCD) in the young.
This chapter reviews the present knowledge, progress made, and future research directions on CPVT with a focus on the genetic background, clinical disease characteristics, and management. The pathophysiologic mechanisms underpinning this condition are discussed in Chapter 51 .
Although the familial nature of CPVT was already observed in the first reports, the genetic background of CPVT was first discovered in 2001. Mutations in the cardiac ryanodine receptor gene ( RYR2 ) were found to underlie the autosomal dominantly inherited form of CPVT, , whereas mutations in cardiac calsequestrin ( CASQ2 ) were identified in autosomal recessively inherited CPVT cases. Over the past few years it has become increasingly evident that the genetic background of CPVT is more complex than initially thought. First, so-called mutation calling of identified variants in RYR2 or CASQ2 can be challenging, and there is evidence that CASQ2 heterozygotes may also display a CPVT phenotype. Second, associations between variants in several other genes and patients with either a “true” CPVT phenotype, a CPVT phenocopy (i.e., patients with a phenotype resembling CPVT who carry a pathogenic variant in a gene that suggests an underlying pathophysiology different from intracellular calcium handling dysfunction), and/or phenotypes that overlap with other conditions, especially congenital long QT syndrome (LQTS), have been reported.
Mutations in RYR2 are identified in approximately 60% of patients with a clear CPVT phenotype. The yield of RYR2 genetic testing decreases to approximately 35% of patients with a possible clinical diagnosis of CPVT, 31% of patients with exertional syncope, and 15% of relatives of victims of exercise or emotion-related SCA or SCD with no signs of other inherited cardiac disease. , Besides the symptomatology and ECG phenotype, the age of the patient is an important predictor of disease; pathogenic RYR2 mutations are more likely to be identified in young individuals.
Hitherto, more than 200 unique, mostly missense pathogenic or likely pathogenic RYR2 mutations have been identified. Approximately 20% of the RYR2 mutations are de novo in origin, and in one study multiple RYR2 mutations were identified in 4 out of 73 patients (5.5%). In a large pediatric cohort, at least two RYR2 variants were identified in 6.7% of the patients, although fewer than half of the variants were classified as pathogenic or likely pathogenic. Mutations in RYR2 cluster in four hotspots: exons 3 to 15, 44 to 50, 83 to 90, and 93 to 105. Several RYR2 founder mutations have been identified, including the p.G357S mutation in approximately 180 family members from the Canary Islands and the p.R420W mutation in over 80 family members from the Netherlands. Recently a homozygous multiexon duplication in RYR2 among Amish youths was reported.
Although rare missense mutations in RYR2 were often considered pathogenic in the past, several studies have shown that the prevalence of these variants in the general population is significant. Approximately 3% of ostensibly healthy individuals carry a rare RYR2 protein-altering variant. This “genetic noise” introduces uncertainty in genetic test results that were previously considered “positive.” A study that analyzed the prevalence of 170 previously reported CPVT-associated RYR2 variants showed that these variants were identified in 41 of 6131 control subjects (6.7%), yielding a CPVT prevalence of up to 1:150, which is much higher than the estimated prevalence of clinically diagnosed CPVT. These findings were confirmed by another study, in which 38 (mostly RYR2 ) variants previously associated with CPVT were identified in the ExAC database comprising over 60,000 individuals and leading to a predicted CPVT prevalence of 1:132. A study assessing the prevalence of rare RYR2 and CASQ2 variants in a cohort referred for clinical whole-exome sequencing found a prevalence of 8.8%, again supporting the idea that variants of undetermined significances in these genes are unlikely to represent markers of CPVT pathogenicity in the absence of clinical suspicion for CPVT. On the other hand, using a pretest clinical probability of CPVT has been shown to be useful in reclassifying RYR2 variants of uncertain significance. In a study in 233 RYR2 -variant positive individuals, the variant of uncertain significance rate dropped from close to 50% to less than 10% by this phenotype-enhanced approach.
In 2001, mutations in the gene encoding CASQ2 were found to underlie a malignant autosomal recessive inherited form of CPVT in seven related Bedouin families. CASQ2 is located within the sarcoplasmic reticulum and also plays a pivotal role in calcium homeostasis. Mutations in CASQ2 are identified in less than 5% of CPVT index cases. Although CASQ2 mutations are typically identified in consanguineous families, compound heterozygosity in nonconsanguineous families has also been observed. Homozygous and compound heterozygous forms are highly penetrant and are associated with a high incidence of arrhythmic events at young age. More recent data suggest that heterozygous CASQ2 mutations can sometimes manifest with a malignant CPVT phenotype, indicating that CASQ2 heterozygotes should also undergo cardiac evaluation.
In 2007 a third CPVT form, inherited as an autosomal recessive trait, was mapped to a 25-Mb interval on chromosome 7p14-p22 in a report including four children from an inbred Arabic family. All children presented before the age of 12 years and showed mild QTc interval prolongation, and three children eventually succumbed to the condition. The disease-causing gene, the gene encoding trans-2,3-enoyl-CoA reductase-like protein ( TECRL ), was identified in 2016. The patients showed an overlap phenotype between CPVT and LQTS. This was confirmed in functional studies in cardiomyocytes differentiated from patient-specific human induced pluripotent stem cells, which manifested action potential duration prolongation (LQTS) as well as a disturbed calcium handling and increased propensity for delayed afterdepolarizations during catecholaminergic stimulation (CPVT). Later, a young CPVT patient with compound heterozygosity in the TECRL gene was reported. In a study on 631 patients with suspected CPVT or LQTS, four patients with homozygous or compound heterozygous TECRL mutations were identified. All patients showed features of CPVT, sometimes combined with a prolonged QT interval.
In 2012, cardiac triadin ( TRDN ) was reported as a new gene responsible for an autosomal recessive form of CPVT. Triadin is a transmembrane sarcoplasmic reticulum protein and is another component of sarcoplasmic reticulum calcium release during cardiac contraction. In the initial report, three TRDN mutations were identified in 2 of 97 CPVT probands without mutations in RYR2 or CASQ2 (2%). An international series of 21 patients carrying recessive null mutations in TRDN showed that patients do not have typical CPVT or LQTS, but instead suffer from a distinct overlap disorder that displays clinical features of multiple arrhythmia syndromes.
Mutations in the genes encoding the identical calcium-signaling protein calmodulin ( CALM1-3 ) have been identified in patients with CPVT, with LQTS with exertion-induced ventricular arrhythmias, and idiopathic ventricular fibrillation. In a report from the International Calmodulinopathy Registry, 28% of the patients showed a CPVT phenotype and 49% an LQTS phenotype. In the patients with CPVT, 78% carried a de novo mutation, the median age of onset was 6 years, and major arrhythmic events occurred in almost half of the patients.
Multiple series have described a phenotype with polymorphic ventricular ectopy in carriers of gain-of-function mutations in the gene encoding the pore-forming subunit of the cardiac sodium channel, Na V 1.5 ( SCN5A ) , including families in which these arrhythmias were exercise induced. , Nevertheless, a feature that distinguishes them from “true” CPVT is abundant ventricular ectopy occurring at rest.
Mutations in the gene encoding the potassium inwardly rectifying channel K ir 2.1 ( KCNJ2 ) are generally associated with Andersen-Tawil syndrome but may also cause a CPVT phenocopy, including the typical bidirectional VT (see Differential Diagnosis).
Finally, plakophilin-2 truncation variants can precipitate exercise-associated arrhythmic events before the presence of overt cardiomyopathy and thereby clinically mimic CPVT.
The typical clinical presentation of CPVT is the occurrence of syncope, SCA, or SCD in circumstances of physical or emotional stress in normally developed children or young adolescents. Swimming seems a particular important trigger, and electronic gaming is another reported trigger. In a pediatric cohort, however, approximately 25% of the arrhythmic events were atypically triggered (e.g., occurred at rest). Arrhythmic events during sexual intercourse have been described but are rare.
In large series the age of onset of symptoms was 10.8 years (interquartile range, 6.8–13.2 years) and 12 ± 8 years. Some patients are initially diagnosed with epilepsy because CPVT-related syncope may include convulsive movements and urinary or fecal incontinence. If these symptomatic patients receive antiepileptic or no treatment, further arrhythmic events can occur and eventually can prove fatal in some cases. Classically, the family history of these young patients includes relatives with syncope, SCA, SCD, or “epilepsy” under similar conditions.
CPVT has been associated with neurodevelopmental disorders. An increased prevalence of neurodevelopmental disorders, especially intellectual disability, was identified among families with CPVT (8% vs. 1%–3% in a general population). This subgroup displayed a more malignant CPVT phenotype involving supraventricular tachyarrhythmias in approximately 50% and a high rate of arrhythmic events despite receiving adequate medical therapy. CPVT and intellectual disability may share common underlying pathophysiologic mechanisms involving caffeine hyperresponsive, RYR2 -mediated, intracellular calcium handling in the heart and the brain.
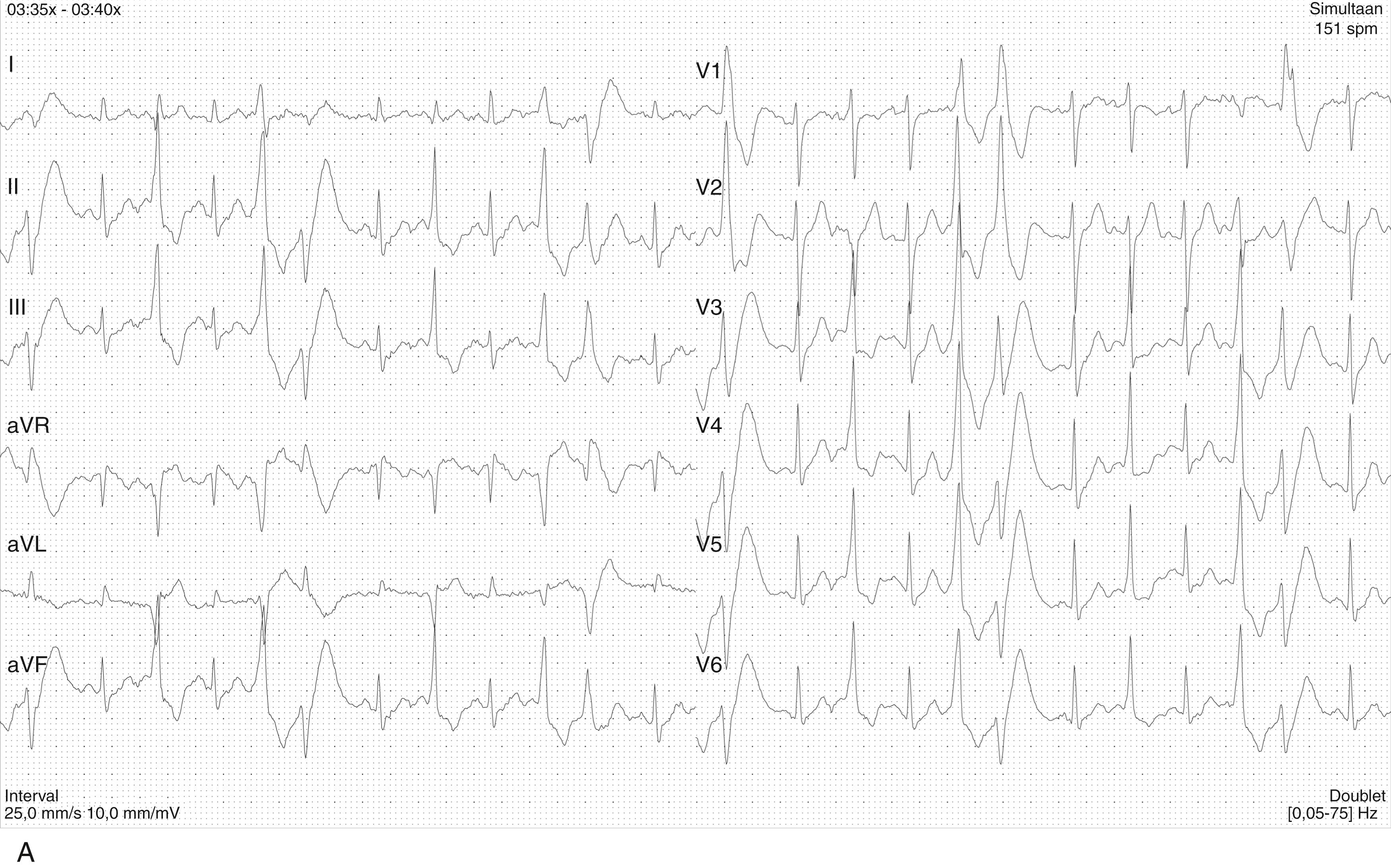
Typically, a gradual increase in ventricular arrhythmia burden and complexity during exercise stress testing is observed, starting with isolated ventricular premature beats (VPB) at a heart rate of approximately 110 to 130 beats/min. In the absence of important therapeutic modifications, the ventricular arrhythmia threshold heart rate is accurately reproducible in an individual patient. VPBs are relatively late-coupled with a coupling interval of approximately 400 ms. , Left bundle branch inferior axis and right bundle branch block superior axis morphologies have consistently been shown to be predominant in CPVT, , and VPB morphologies are usually reproducible in an individual patient. Further exercise causes the number of isolated VPBs to increase to bigeminal VPBs, and eventually polymorphic couplets or nonsustained ventricular tachycardia, including bidirectional ventricular tachycardia, may be induced ( Figs. 91.1 and 91.2A ). In very rare cases, this may further escalate to polymorphic sustained ventricular tachycardia or ventricular fibrillation. When exercise testing is terminated, the ventricular arrhythmias rapidly recede in most patients, whereas VPBs recorded more than 1 minute during the recovery are uncommon. In a substantial subset of patients with ventricular arrhythmias who reach a high maximum heart rate, the ventricular arrhythmias are paradoxically suppressed as heart rates increases further with continued exercise ( Fig. 91.2B ). This phenomenon was also observed in CPVT mice models when intrinsic sinus rates were increased with atropine and after atrial overdrive pacing.

A study of 80 pediatric CPVT patients found evidence for a circadian variation of ventricular arrhythmias. Ventricular arrhythmias occurred significantly more often in the afternoon and evening.
The most common supraventricular manifestation of CPVT is sinus bradycardia and/or sinus node dysfunction. In one study, RYR2 mutation-carriers had a lower average resting heart rate compared with their nonmutation carrying relatives. Heart rates tended to be lowest in males and RYR2 mutation carriers with a CPVT phenotype. In a series including 116 relatives from 15 families who were identified by cascade screening of the RYR2 mutation causing CPVT in the proband, sinus bradycardia was observed in 19%. In addition, other supraventricular dysrhythmias were present in 16% and mainly included intermittent ectopic atrial rhythm identified by Holter monitoring. In another study, paroxysmal supraventricular arrhythmias were observed in 7 of 27 patients with CPVT (26%).
Exercise-induced supraventricular tachyarrhythmias have been reported in CPVT patients but are uncommon.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here