Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Carotid intervention for the treatment of atherosclerotic disease has evolved considerably. The potential for serious neurologic complications during such procedures places a premium on careful studies documenting the overall clinical efficacy of intervention compared with medical therapy.
Carotid bifurcation disease and intracranial atherosclerosis account for 15% to 20% of all ischemic strokes and represent an important target for stroke prevention.
Contemporary carotid bifurcation intervention involves the use of self-expanding stents with embolic protection systems to reduce the risk of distal embolization. The technique has proven to be equivalent to carotid endarterectomy in high-risk patients. There remains debate on the interpretation of randomized trial data for carotid stenting and on Medicare reimbursement in normal-risk patients.
Proximal vertebral artery disease may account for up to 10% of posterior circulation ischemic events. Intervention at this site is straightforward and safe but has not proven to be superior to medical therapy alone.
Intracranial intervention is evolving to be an important therapy for acute stroke at qualified institutions.
Further refinements in technique, technology, and patient selection, together with dedicated randomized controlled trials, will allow cerebrovascular intervention to realize its true potential in patients with stroke.
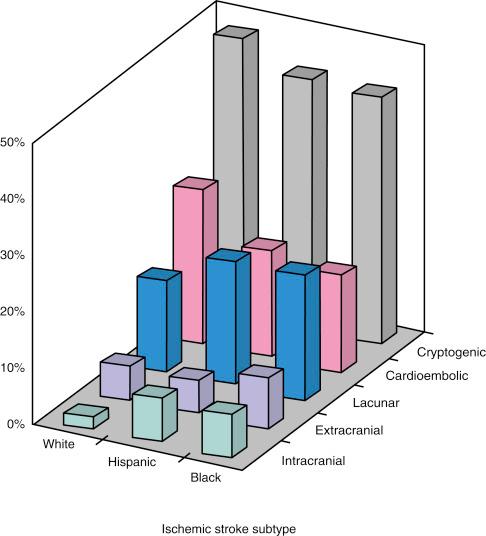
Stroke is the leading cause of adult disability and the third leading cause of death in North America, Europe, South America, and Asia. Most strokes (80% to 85%) are ischemic in etiology. In the United States, atherosclerotic disease affecting the extracranial and intracranial arterial circulation accounts for approximately 20% of ischemic strokes ( Fig. 46.1 ) and thus is an important target for stroke prevention. Carotid intervention has evolved largely for the treatment of atherosclerotic disease with the goal of stroke prevention. Based on dramatic technological advances and increased operator expertise, these procedures can currently be performed with a high rate of technical success. However, because of the potential for serious neurologic complications from endovascular intervention in the cerebrovascular circulation, clear documentation of the safety of these procedures and their overall clinical efficacy is of paramount importance. These considerations have raised the bar for cerebrovascular intervention compared with other peripheral vascular procedures.
In the field of cerebrovascular intervention, carotid bifurcation intervention is unique in that the natural history of carotid artery bifurcation disease has been well defined and large randomized trials have previously documented the clinical effectiveness of surgical revascularization for this disease. There is already a large evidence base supporting carotid intervention in specific patient subgroups, and several randomized trials are ongoing in the remaining patient populations. With more than 140,000 carotid endarterectomy (CEA) procedures performed each year in the United States, and more than 280,000 worldwide, the potential impact of percutaneous revascularization has captured the interest of endovascular specialists who are keen to offer an alternative to surgery.
In contrast, endovascular intervention in the cerebrovascular circulation outside of the carotid bifurcation has been hampered by two important considerations: the natural history of noncarotid bifurcation cerebrovascular disease is less well defined, and there is a notable absence of randomized data documenting the benefit of revascularization compared with medical therapy alone. However, despite these obstacles, dramatic advances in the technical aspects of these interventions have been made, and there is an increased recognition of the need for well-designed clinical studies that address these deficiencies. What is often underappreciated is that noncarotid bifurcation cerebrovascular disease is responsible for at least the same number of ischemic strokes as carotid bifurcation disease and represents an equally important target for stroke prevention.
This chapter summarizes the current status of carotid bifurcation intervention and the most frequently performed noncarotid bifurcation cervical cerebrovascular interventions, notably of the proximal vertebral artery (VA). The emerging role of intracranial intervention in acute stroke management is also introduced.
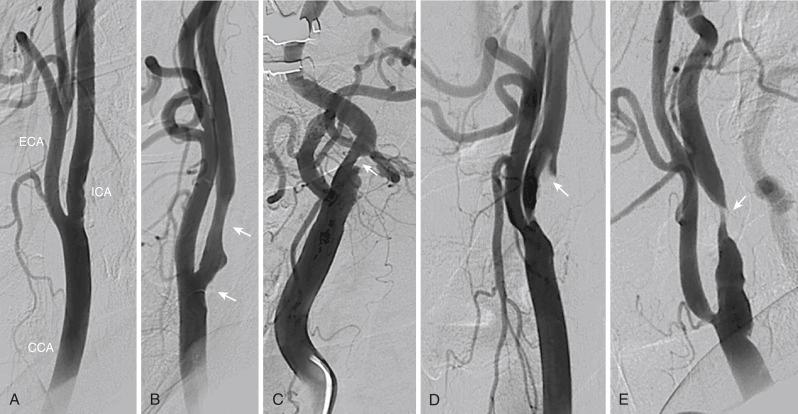
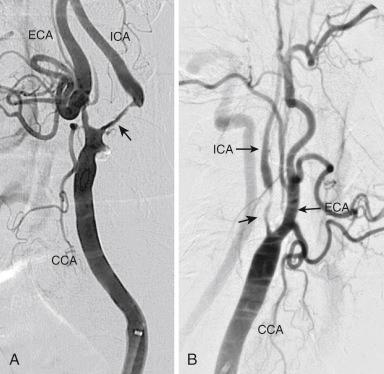
The carotid bifurcation has a remarkable predilection for the development of atherosclerosis, which is typically located at the origin of the internal carotid artery (ICA) ( Fig. 46.2 ). This plaque is similar to that found at other sites throughout the arterial system in that it contains a dense cap of connective tissue with embedded smooth muscle cells and an underlying core of lipid and necrotic debris. Histologic studies of plaque from the carotid bifurcation of symptomatic and asymptomatic individuals have revealed features associated with the development of symptoms that are similar to those associated with plaque vulnerability in the coronary circulation: reduced amounts of collagen, increased inflammation, thinning of the fibrous cap, and increased cholesterol in the necrotic core. Based on our current understanding, these processes result in plaque fissuring or rupture at the carotid bifurcation, causing either occlusive or nonocclusive thrombus formation. The dominant mechanism of stroke is believed to result from distal thromboembolism to the anterior cerebral circulation. However, a number of considerations, such as the size and composition of the embolus, the presence of contralateral disease, the anatomy of the circle of Willis, and the activity of fibrinolytic pathways, may attenuate or accentuate the clinical consequence of the pathologic event. Consequently, the same pathologic event may result in a reversible neurologic deficit (i.e., transient ischemic attack [TIA]), an irreversible neurologic deficit (i.e., stroke), or no symptoms at all.
In clinical practice, two dominant factors are used to determine the risk of ischemic complications from a lesion of the carotid artery bifurcation: the symptomatic status of the lesion and the severity of stenosis. Although many of these data are derived from the medical arms of the large randomized CEA trials performed between the late 1980s and early 2000s, these considerations continue to be used as the major criteria for choosing patients for endovascular procedures and for enrolling subjects in carotid endovascular trials.
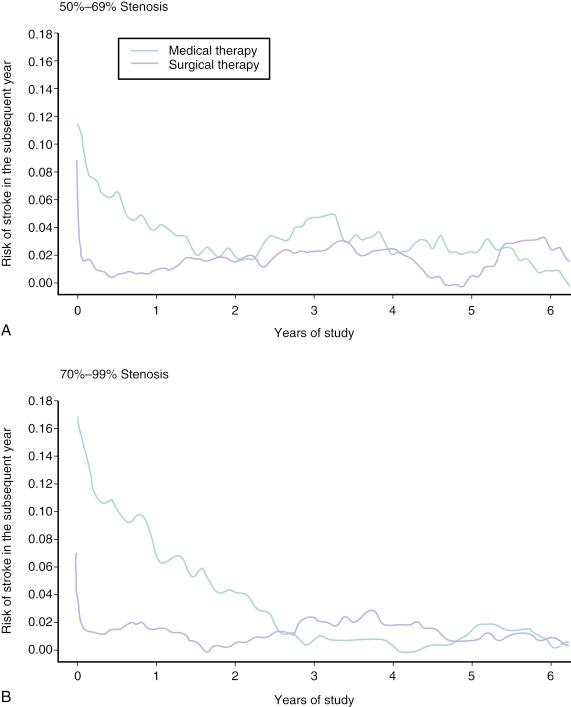
Symptomatic lesions of the carotid bifurcation are associated with a high risk of recurrent ischemic stroke. In the North American Symptomatic Carotid Endarterectomy Trial (NASCET), the risk of any ipsilateral stroke at 2-year follow-up in medically treated patients with symptomatic stenoses of 70% to 99% was 26%. Among patients with symptomatic stenoses of 50% to 69%, the 5-year risk of any ipsilateral stroke was 22.2%. There is a close temporal relationship between these recurrent strokes and the index event, with a steep exponential decline in risk within the first months, followed by a more gradual decline and ultimate normalization of risk at 2 to 3 years ( Fig. 46.3 ).
By contrast, asymptomatic lesions of the carotid bifurcation are associated with a much lower risk of ischemic stroke. Over a 5-year period after an asymptomatic carotid stenosis was diagnosed (more than 60% by ultrasound), the risk of any stroke among medically treated patients in the Asymptomatic Carotid Surgery Trial (ACST) was 11%. Not surprisingly, the risk of stroke was constant over the duration of the study. The implication from these findings is that carotid revascularization should be performed as expediently as possible after a neurologic event caused by a culprit symptomatic stenosis, whereas intervention for an asymptomatic lesion may be approached in a more elective fashion.
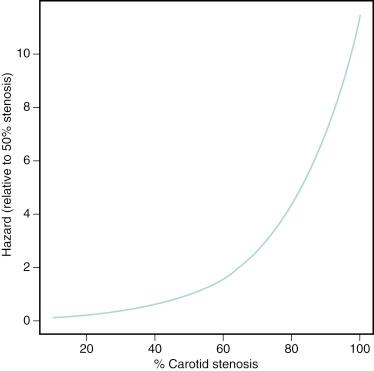
Among symptomatic patients, a close relationship between the severity of stenosis as assessed by careful angiographic methods and subsequent risk of ipsilateral stroke has been demonstrated. The relationship is nonlinear, with a steep increase in risk associated with the tightest degree of stenosis ( Fig. 46.4 ). However, for symptomatic patients with “near-occlusion” of the ICA—defined as a stenosis causing obstruction to flow sufficient to result in a decrease in the ICA diameter beyond the lesion ( Fig. 46.5 )—there are data to suggest that the risk of recurrent stroke is reduced compared with patients with severe stenosis without features of near-occlusion. One potential explanation for this finding is the reduced likelihood of distal cerebral embolization caused by diminished flow distal to a critical stenosis. Among asymptomatic patients, the association between stenosis severity and risk of subsequent stroke has been inconsistent. This finding likely underscores the heterogeneous nature of carotid plaque histology in asymptomatic patients and suggests that assessments of plaque vulnerability may be a more potent predictor of recurrent events than severity of stenosis in this patient group.
Currently there are more sophisticated models to predict the risk of stroke in patients with carotid disease, particularly for symptomatic patients. In addition to stenosis severity, these models incorporate variables such as age, sex, nature of the presenting symptomatic event, time since the index event, plaque surface morphology, and transcranial Doppler findings to provide a more individualized estimate of risk. However, these models have yet to be incorporated into patient selection criteria in randomized trials to more fully establish their clinical relevance.
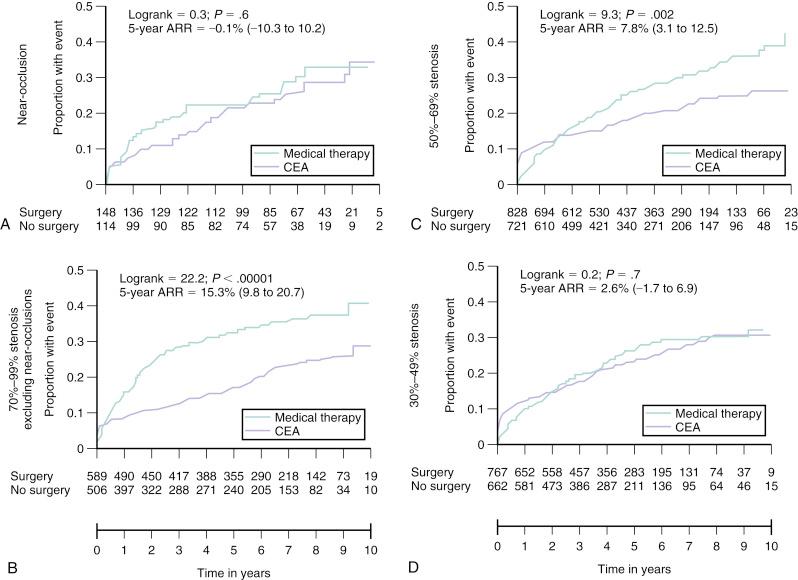
The benefit of carotid revascularization in patients with carotid artery disease has been documented in several randomized controlled trials (RCTs) comparing medical therapy with surgical revascularization (i.e., CEA). These data are extremely important in any discussion of endovascular therapy for carotid bifurcation disease because they form the cornerstone justifying revascularization in certain subsets of patients. In a pooled analysis of data from the three major RCTs in symptomatic patients, CEA compared with medical therapy reduced the end point of stroke or operative death at 5 years in patients with carotid stenoses of 50% or greater, as assessed by carotid angiography using the NASCET criteria ( Fig. 46.6 ). This benefit was more pronounced in patients with stenoses of 70% to 99% (absolute risk reduction [ARR] 15.3%; 95% confidence interval [CI] 9.8% to 20.7%) than in those with stenoses of 50% to 69% (ARR 7.8%; 95% CI 3.1% to 12.5%). In addition, the crossover of the event-free curves occurred very early in the patient cohort with 70% to 99% stenoses (1 to 2 months) compared with the patient cohort with 50% to 69% stenosis (1 year). The incidence of perioperative stroke and/or death in these studies was uniformly less than 6%; the benefits derived from CEA are predicated on the maintenance of similar procedural outcomes. No significant benefit was observed in patients with near-occlusion of the carotid artery (ARR 0.1%; 95% CI −10.3 to 10.2), likely related to the lower risk of recurrent stroke with medical therapy in this group. These studies were performed in the late 1980s and early to mid-1990s; therefore the only stipulated medical therapy in the nonsurgical arm was aspirin. Contemporary medical therapy would likely attenuate the observed benefit associated with CEA. However, given the magnitude of the observed benefit associated with CEA in symptomatic patients, investigators have been reluctant to repeat randomized studies using contemporary medical therapy alone as a treatment arm.
Compared with medical therapy, CEA has also been shown to significantly reduce the incidence of stroke or operative death at 5-year follow-up in asymptomatic patients with carotid stenoses of 60% or greater, as assessed by carotid ultrasound (11.8% vs. 6.4%; ARR 5.4%; 95% CI 3% to 7.8%). It is important to emphasize that in this asymptomatic population, the early hazard associated with revascularization persists up to 2 years from the time of CEA. If the life expectancy of the patient is less than 5 years, then significant benefit should not be anticipated. In addition, participation in these trials involving patients with asymptomatic carotid stenoses required documentation of a perioperative stroke and death rate of less than 3% at the investigation site, and the generalization of these findings is predicated on reproducing similar procedural outcomes.
Initial animal experimentation with percutaneous carotid revascularization began in the late 1970s and was followed by the first clinical reports of carotid angioplasty in the early 1980s. The first rigorous clinical testing of percutaneous carotid revascularization began in the mid-1990s. Although these studies demonstrated feasibility, two subsequent pivotal developments allowed percutaneous carotid revascularization to emerge as a viable alternative to CEA in the treatment of carotid disease: the ability to provide protection from distal embolization at the time of intervention, using a variety of embolic protection devices (EPDs), and the use of self-expanding stents. Carotid artery stenting (CAS) using self-expanding stents in combination with embolic protection represents the contemporary approach to carotid revascularization.
Before any CAS procedure is undertaken, clinical assessment of the patient and anatomic assessment of the aortic arch and carotid/cerebral vasculature are essential. Advanced age (>80 years) has been associated with significantly worse outcomes with CAS and should be carefully considered for the appropriateness of intervention. Decreased cerebral reserve, manifested by the presence of dementia or cognitive impairment, and a history of prior strokes or lacunar infarcts increase the likelihood that distal embolization will be clinically manifested and are relative contraindications for the procedure. Anatomic assessments usually can be made based on noninvasive studies, notably computed tomography (CT) angiography and magnetic resonance (MR) angiography. CT angiography offers higher spatial resolution and superior visualization of the aortic arch compared with MR angiography, and it allows an assessment of the degree of calcification of the aortic arch and carotid bifurcation lesion that is not possible with MR angiography. Table 46.1 lists the anatomic features that should be reviewed and highlights the importance of each. Overall, these anatomic features allow the operator to more accurately determine the procedural risk and facilitate the planning of appropriate technique for procedural success.
| Angiographic Assessment | Impact on Interventional Procedure |
|---|---|
| Arch Anatomy | |
|
|
| Lesion Characteristics | |
|
|
| ICA Distal to Lesion | |
|
|
| Patency of External Carotid Artery | |
|
|
In most circumstances, CAS procedures are performed with the use of femoral artery access. Although the extent of baseline angiography varies depending on the preprocedural noninvasive assessment, high-quality angiography of the carotid bifurcation, the ipsilateral ICA, and intracranial anterior circulation is essential. We administer a heparin bolus of 25 mg/kg before any diagnostic cerebrovascular procedure in an effort to minimize the risk of thrombotic complications. A variety of catheter types are used to perform angiography, depending on the personal preference of the operator and the anatomy of the aortic arch and great vessels. For patients with uncomplicated anatomy (i.e., type I aortic arch, no tortuosity of the great vessels), a Bernstein catheter functions well. For more complicated anatomies (e.g., type II or III arch, tortuosity of the great vessels, bovine origin of the left common carotid artery [CCA]), a Vitek or Simmons catheter is usually required.
The technique for CAS placement follows a number of well-defined steps. Before CAS placement, all patients should receive aspirin. In addition, it is our practice to administer clopidogrel before the procedure. During the procedure, anticoagulation using unfractionated heparin to achieve an activated clotting time (ACT) of 275 to 300 seconds is standard. For patients with a contraindication to heparin, a direct thrombin inhibitor such as bivalirudin has been shown to be safe. In a cohort of 3555 patients from the Carotid Artery Revascularization and Endarterectomy (CARE) registry, bivalirudin was associated with less need for transfusion (0.9% vs. 1.5%; P = .01) and no difference in myocardial infarction (MI), stroke, and death at 30 days, compared with unfractionated heparin in a propensity score analysis. Most operators perform the procedure without the administration of sedatives, which enhances the ability to screen for any neurologic change during the procedure.
To deliver the range of contemporary equipment required for CAS, a 6-Fr sheath or 8-Fr guide must be placed in the distal CCA. In patients with difficult aortic arch anatomy, bovine origin of the left CCA, occlusion of the external carotid artery (ECA), distal CCA lesions, or significant tortuosity of the great vessels, this can be one of the most technically challenging parts of the procedure. This portion of the procedure is “unprotected” in that there is no distal EPD to protect against distal embolization, so the safety of this step is heavily operator dependent.
The standard procedure for delivery of a 6-Fr sheath in the CCA is as follows. The CCA of interest is engaged with a diagnostic catheter. A stiff-angled Glidewire is advanced into the ECA, and the diagnostic catheter is advanced over it. The Glidewire is exchanged for a superstiff Amplatz or SupraCore wire, and then the diagnostic catheter is removed. The 6-Fr sheath and its dilator are delivered over the stiff wire to the distal CCA, after which the dilator is removed.
Although this standard approach is sufficient for approximately 70% of cases, a number of variations to the technique may be necessary, depending on the specific anatomic features of the individual patient. Much of the learning curve in CAS involves achieving experience with these variations and learning how to predict which variation is appropriate for an individual patient’s anatomy. One of the pivotal dogmas in CAS is that guidewires and catheters should never be placed across the carotid lesion to deliver the sheath or guide to the CCA. It is preferable to refer the patient for CEA than to persist in risky attempts to deliver the guide or sheath.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here