Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Paul Zoll developed the first transcutaneous electronic pacemaker in 1952 for the treatment of life-threatening bradycardia. The first internal pacemaker was implanted in 1958 for the treatment of complete heart block and in the management of Stokes-Adams seizures. Early pacemaker models were simple, fixed-rate devices. Thoracic surgeons performed most early implants by placing epimyocardial leads directly on the exposed heart; these leads were connected to an abdominally implanted pulse generator. Modern pacemakers have sophisticated microprocessors that apply diagnostic and therapeutic algorithms, which have dramatically increased their versatility.
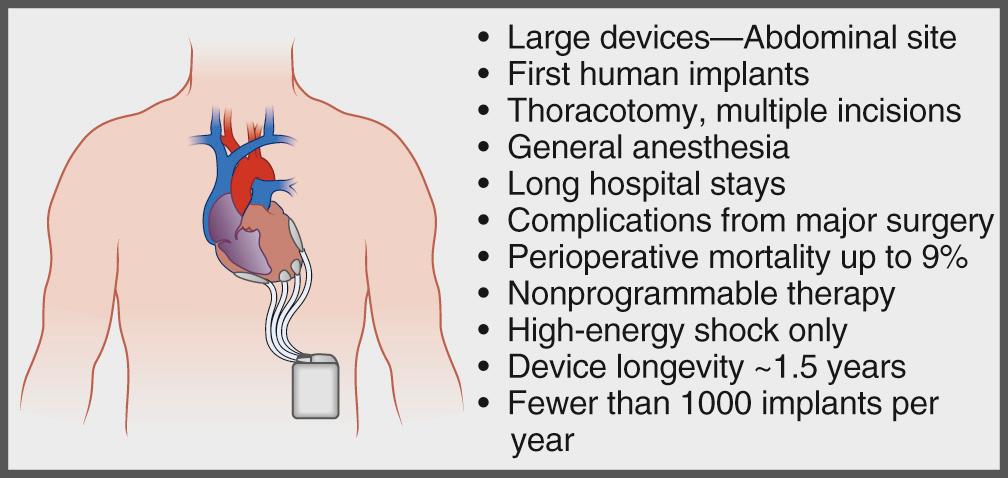
The development of the implantable cardioverter-defibrillator (ICD) was pioneered by Michel Mirowski. The initial purpose of the ICD was to provide immediate, automatic defibrillation to ambulatory patients who were victims of a lethal ventricular arrhythmia. Mirowski performed the first human ICD implantation in 1980. First-generation ICDs were composed of large generators (>200 cm 3 volume) implanted in an abdominal pocket with epicardial defibrillator patches. Whereas these early ICDs were capable of only high-energy shocks, current ICDs are small (<40 cm 3 volume), yet they contain all the advanced pacing functions of modern pacemakers as well as complex tachycardia treatment options ( Figs. 85-1 and 85-2 ). Despite their diminutive size, newer ICDs have become progressively superior in their sensing, diagnosis, and treatment of arrhythmias. Since the late 1990s, ICDs have emerged as the single most effective lifesaving intervention in the prevention of sudden cardiac death.
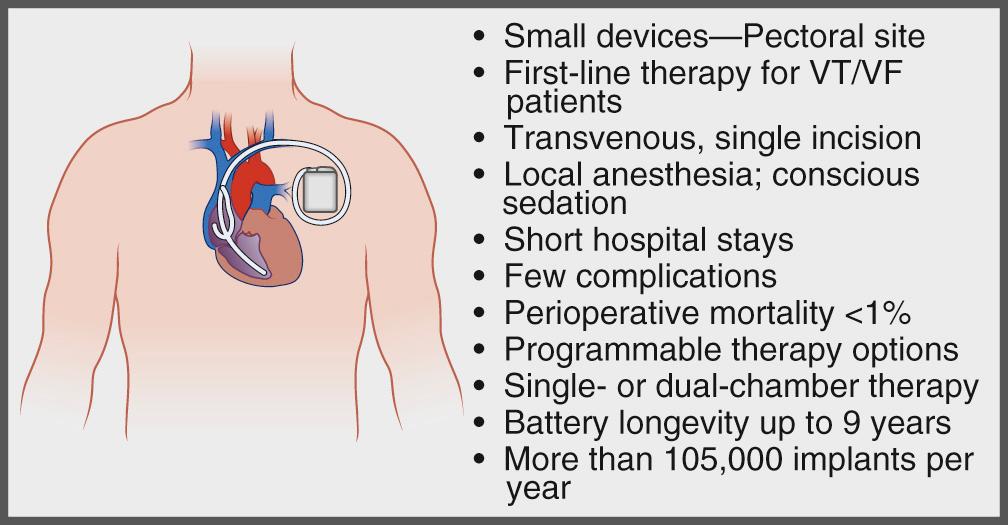
With increased sophistication and miniaturization of pulse generators and the development of the much simpler and safer transvenous approach for implantation of cardiac devices, indications for cardiac pacing as well as for ICDs have dramatically expanded. In addition, the U.S. Food and Drug Administration (FDA) approved the totally subcutaneous ICD in September 2012. It is estimated that approximately 400,000 devices are implanted each year in the United States, and there are more than 3 million patients with implanted cardiac devices currently.
The remainder of this chapter focuses on the description, implantation techniques, indications, and complications of current implantable cardiac pacemakers and defibrillators.
The American College of Cardiology/American Heart Association/Heart Rhythm Society (ACC/AHA/HRS) guidelines for device-based therapy of cardiac rhythm abnormalities were updated in 2012.
Placement of a temporary pacemaker is indicated whenever hemodynamic compromise is present because of a bradyarrhythmia. Temporary pacemakers should also be placed prophylactically if a high risk for development of hemodynamically untolerated bradycardia is present. Specific guidelines for placement of temporary pacemakers in the setting of acute myocardial infarction exist. Temporary transvenous pacing is indicated in symptomatic sinus bradycardia, sinus pauses of more than 3 seconds, or sinus bradycardia with a heart rate below 40 beats/minute associated with hypotension or hemodynamic compromise, and if unresponsive to a maximum dose (2 mg) of intravenous atropine. Other class I indications for temporary transvenous pacing in acute myocardial infarction include ventricular asystole, alternating left and right bundle branch block, recurrent polymorphic ventricular tachycardia with a heart rate less than 60 beats/minute and prolonged QT, and new bundle branch block or fascicular block and right bundle branch block in the setting of Möbitz II second-degree atrioventricular (AV) block.
Table 85-1 summarizes the different sites that can be used for insertion of a temporary pacemaker. The particular patient and the advantages and disadvantages of each site are important factors in the decision of which site to use. For example, the internal jugular and subclavian veins may be chosen when need for stability and longer pacing requirement is anticipated. If a permanent pacemaker will be required in the future, the temporary pacemaker should be placed through a vein remote from the preferred site for permanent pacemaker implantation. Use of the antecubital veins minimizes bleeding in the coagulopathic patient. However, the risk of cardiac perforation or lead dislodgement is higher if the arm is not kept fully immobilized.
| Site | Advantages | Disadvantages |
|---|---|---|
| Femoral vein | Easy access | Leg must remain immobilized |
| High infection risk | ||
| Fluoroscopy required for proper placement | ||
| Patient must lie flat | ||
| Internal jugular vein | Good site for pacer placement (right better than left) | Risk of pneumothorax, inadvertent carotid artery puncture |
| Patient must lie flat for access; Trendelenburg position preferred to avoid air embolism | ||
| Subclavian vein | Good site for pacer placement (left better than right) | Risk of pneumothorax, hemothorax with inadvertent subclavian artery puncture |
| Patient must lie flat for access; Trendelenburg position preferred to avoid air embolism | ||
| Antecubital vein (basilic, median basilic, or cephalic) | Access is low risk | Risk of dislodgement; arm must remain immobilized |
| Good site for pacer placement (left better than right) | Basilic or median basilic preferred (cephalic has tortuous course to central veins) | |
| Fluoroscopy required for pacer placement |
Justifications for permanent pacemaker implantation include alleviation of symptoms and prevention of subsequent morbidity or mortality as a direct result of bradycardia. Bradycardia can result from a variety of disorders of the sinus node, the AV node, the His-Purkinje system, or a combination of these. Sinus node or AV node disease is often not life-threatening but may cause significant symptoms. On the other hand, disease of the His-Purkinje system may be asymptomatic until the development of AV block and its associated severe adverse events.
Symptoms from bradycardia generally result from inadequate cardiac output. Such symptoms may be vague and include fatigue, decreased exercise tolerance, dyspnea on exertion, lightheadedness, dizziness, congestive heart failure, presyncope, and syncope. Patient-triggered ambulatory cardiac monitoring is often helpful in establishing that such nonspecific symptoms are in fact the result of symptomatic bradycardia. Boxes 85-1 through 85-12 summarize the indications for permanent cardiac pacing published by the ACC/AHA Task Force on Practice Guidelines in 2008 and maintained as part of the 2012 focused update.
Permanent pacemaker implantation is indicated for sinus node dysfunction (SND) with documented symptomatic bradycardia, including frequent sinus pauses that produce symptoms. (Level of Evidence: C)
Permanent pacemaker implantation is indicated for symptomatic chronotropic incompetence. (Level of Evidence: C)
Permanent pacemaker implantation is indicated for symptomatic sinus bradycardia that results from required drug therapy for medical conditions. (Level of Evidence: C)
Permanent pacemaker implantation is reasonable for SND with heart rate less than 40 beats per minute (bpm) when a clear association between significant symptoms consistent with bradycardia and the actual presence of bradycardia has not been documented. (Level of Evidence: C)
Permanent pacemaker implantation is reasonable for syncope of unexplained origin when clinically significant abnormalities of sinus node function are discovered or provoked in electrophysiologic studies. (Level of Evidence: C)
Permanent pacemaker implantation may be considered in minimally symptomatic patients with chronic heart rate less than 40 bpm while awake. (Level of Evidence: C)
Permanent pacemaker implantation is not indicated for SND in asymptomatic patients. (Level of Evidence: C)
Permanent pacemaker implantation is not indicated for SND in patients for whom the symptoms suggestive of bradycardia have been clearly documented to occur in the absence of bradycardia. (Level of Evidence: C)
Permanent pacemaker implantation is not indicated for SND with symptomatic bradycardia due to nonessential drug therapy. (Level of Evidence: C)
Permanent pacemaker implantation is indicated for third-degree and advanced second-degree atrioventricular (AV) block at any anatomic level associated with bradycardia with symptoms (including heart failure) or ventricular arrhythmias presumed to be due to AV block. (Level of Evidence: C)
Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level associated with arrhythmias and other medical conditions that require drug therapy that results in symptomatic bradycardia. (Level of Evidence: C)
Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level in awake, symptom-free patients in sinus rhythm, with documented periods of asystole greater than or equal to 3.0 seconds or any escape rate less than 40 beats per minute (bpm), or with an escape rhythm that is below the AV node. (Level of Evidence: C)
Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level in awake, symptom-free patients with atrial fibrillation (AF) and bradycardia with 1 or more pauses of at least 5 seconds or longer. (Level of Evidence: C)
Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level after catheter ablation of the AV junction. (Level of Evidence: C)
Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level associated with postoperative AV block at any anatomic level associated with postoperative AV block that is not expected to resolve after cardiac surgery. (Level of Evidence: C)
Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level associated with neuromuscular diseases with AV block, such as myotonic muscular dystrophy, Kearns-Sayre syndrome, Erb dystrophy (limb-girdle muscular dystrophy), and peroneal muscular atrophy, with or without symptoms. (Level of Evidence: B)
Permanent pacemaker implantation is indicated for second-degree AV block with associated symptomatic bradycardia regardless of type or site of block. (Level of Evidence: B)
Permanent pacemaker implantation is indicated for asymptomatic persistent third-degree AV block at any anatomic site with average awake ventricular rates of 40 bpm or faster if cardiomegaly or left ventricular (LV) dysfunction is present or if the site of block is below the AV node. (Level of Evidence: B)
Permanent pacemaker implantation is indicated for second- or third-degree AV block during exercise in the absence of myocardial ischemia. (Level of Evidence: C)
Permanent pacemaker implantation is reasonable for persistent third-degree AV block with an escape rate greater than 40 bpm in asymptomatic adult patients without cardiomegaly. (Level of Evidence: C)
Permanent pacemaker implantation is reasonable for asymptomatic second-degree AV block at intra- or infra-His levels found at electrophysiologic study. (Level of Evidence: B)
Permanent pacemaker implantation is reasonable for first- or second-degree AV block with symptoms similar to those of pacemaker syndrome or hemodynamic compromise. (Level of Evidence: B)
Permanent pacemaker implantation is reasonable for asymptomatic type II second-degree AV block with a narrow QRS. When type II second-degree AV block occurs with a wide QRS, including isolated right bundle branch block, pacing becomes a class I recommendation. (See Section 2.1.3, “Chronic Bifascicular Block.”) (Level of Evidence: B)
Permanent pacemaker implantation may be considered for neuromuscular disease such as myotonic muscular dystrophy. Erb dystrophy (limb-girdle muscular dystrophy), and peroneal muscular atrophy with any degree of AV block (including first-degree AV block), with or without symptoms, because there may be unpredictable progression of AV conduction disease. (Level of Evidence: B)
Permanent pacemaker implantation may be considered for AV block in the setting of drug use and/or drug toxicity when the block is expected to recur even after the drug is withdrawn. (Level of Evidence: B)
Permanent pacemaker implantation is not indicated for asymptomatic first-degree AV block. (See Section 2.1.3, “Chronic Bifascicular Block.”) (Level of Evidence: B)
Permanent pacemaker implantation is not indicated for asymptomatic type I second-degree AV block at the supra-His (AV node) level or that which is not known to be intra or infra or infra-Hisian. (Level of Evidence: C)
Permanent pacemaker implantation is not indicated for AV block that is expected to resolve and is unlikely to recur (e.g., drug toxicity, Lyme disease, or transient increases in vagal tone or during hypoxia in sleep apnea syndrome in the absence of symptoms). (Level of Evidence: B)
Permanent pacemaker implantation is indicated for advanced second-degree atrioventricular (AV) block or intermittent third-degree AV block. (Level of Evidence: B)
Permanent pacemaker implantation is indicated for type II second-degree AV block. (Level of Evidence: B)
Permanent pacemaker implantation is indicated for alternating bundle branch block. (Level of Evidence: C)
Permanent pacemaker implantation is reasonable for syncope not demonstrated to be due to AV block when other likely causes have been excluded, specifically ventricular tachycardia (VT). (Level of Evidence: B)
Permanent pacemaker implantation is reasonable for an incidental finding at electrophysiologic study of a markedly prolonged HV interval (greater than or equal to 100 milliseconds) in asymptomatic patients. (Level of Evidence: B)
Permanent pacemaker implantation is reasonable for an incidental finding at electrophysiologic study of pacing-induced infra-His block that is not physiologic. (Level of Evidence: B)
Permanent pacemaker implantation may be considered in the setting of neuromuscular diseases such as myotonic muscular dystrophy, Erb dystrophy (limb-girdle muscular dystrophy), and peroneal muscular atrophy with bifascicular block or any fascicular block, with or without symptoms. (Level of Evidence: C)
Permanent pacemaker implantation is not indicated for fascicular block without AV block or symptoms. (Level of Evidence: B)
Permanent pacemaker implantation is not indicated for fascicular block with first-degree AV block without symptoms. (Level of Evidence: B)
Permanent ventricular pacing is indicated for persistent second-degree atrioventricular (AV) block in the His-Purkinje system with alternating bundle branch block or third-degree AV block within or below the His-Purkinje system after ST-segment elevation myocardial infarction (MI). (Level of Evidence: B)
Permanent ventricular pacing is indicated for transient advanced second- or third-degree infranodal AV block and associated bundle branch block. If the site of block is uncertain, an electrophysiologic study may be necessary. (Level of Evidence: B)
Permanent ventricular pacing is indicated for persistent and symptomatic second- or third-degree AV block. (Level of Evidence: C)
Permanent ventricular pacing may be considered for persistent second- or third-degree AV block at the AV node level, even in the absence of symptoms. (Level of Evidence: B)
Permanent ventricular pacing is not indicated for transient AV block in the absence of intraventricular conduction defects. (Level of Evidence: B)
Permanent ventricular pacing is not indicated for transient AV block in the presence of isolated left anterior fascicular block. (Level of Evidence: B)
Permanent ventricular pacing is not indicated for new bundle branch block or fascicular block in the absence of AV block. (Level of Evidence: B)
Permanent ventricular pacing is not indicated for persistent asymptomatic first-degree AV block in the presence of bundle branch or fascicular block. (Level of Evidence: B)
Permanent pacing is indicated for recurrent syncope caused by spontaneously occurring carotid sinus stimulation and carotid sinus pressure that induces ventricular asystole of more than 3 seconds. (Level of Evidence: C)
Permanent pacing is reasonable for syncope without clear, provocative events and with a hypersensitive cardioinhibitory response of 3 seconds or longer. (Level of Evidence: C)
Permanent pacing may be considered for significantly symptomatic neurocardiogenic syncope associated with bradycardia documented spontaneously or at the time of tilt-table testing. (Level of Evidence: B)
Permanent pacing is not indicated for a hypersensitive cardioinhibitory response to carotid sinus stimulation without symptoms or with vague symptoms. (Level of Evidence: C)
Permanent pacing is not indicated for situational vasovagal syncope in which avoidance behavior is effective and preferred. (Level of Evidence: C)
Permanent pacing is indicated for persistent inappropriate or symptomatic bradycardia not expected to resolve and for other class I indications for permanent pacing. (Level of Evidence: C)
Permanent pacing may be considered when relative bradycardia is prolonged or recurrent, which limits rehabilitation or discharge after postoperative recovery from cardiac transplantation. (Level of Evidence: C)
Permanent pacing may be considered for syncope after cardiac transplantation even when bradyarrhythmia has not been documented. (Level of Evidence: C)
Permanent pacing is reasonable for symptomatic recurrent supraventricular tachycardia (SVT) that is reproducibly terminated by pacing when catheter ablation and/or drugs fail to control the arrhythmia or produce intolerable side effects. (Level of Evidence: C)
Permanent pacing is not indicated in the presence of an accessory pathway that has the capacity for rapid anterograde conduction. (Level of Evidence: C)
Permanent pacing is indicated for sustained pause-dependent ventricular tachycardia (VT), with or without QT prolongation. (Level of Evidence: C)
Permanent pacing is reasonable for high-risk patients with congenital long-QT syndrome. (Level of Evidence: C)
Permanent pacing may be considered for prevention of symptomatic, drug-refractory, recurrent atrial fibrillation (AF) in patients with coexisting sinus node dysfunction (SND). (Level of Evidence: B)
Permanent pacing is not indicated for frequent or complex ventricular ectopic activity without sustained VT in the absence of the long-QT syndrome. (Level of Evidence: C)
Permanent pacing is not indicated for torsade de pointes VT due to reversible causes. (Level of Evidence: A)
Cardiac resynchronization therapy (CRT) is indicated for patients who have left ventricular ejection fraction (LVEF) less than or equal to 35%, sinus rhythm, left bundle branch block (LBBB) with a QRS duration greater than or equal to 150 msec, and New York Heart Association (NYHA) class II, III, or ambulatory IV symptoms on optimal recommended medical therapy. (Level of Evidence: A for NYHA class III/IV; Level of Evidence: B for NYHA class II)
CRT can be useful for patients who have LVEF less than or equal to 35%, sinus rhythm, LBBB with a QRS duration 120 to 149 msec, and NYHA class II, III, or ambulatory IV symptoms on optimal recommended medical therapy. (Level of Evidence: B)
CRT can be useful for patients who have LVEF less than or equal to 35%, sinus rhythm, a non-LBBB pattern with a QRS duration greater than or equal to 150 msec, and NYHA class III/ambulatory class IV symptoms on optimal recommended medical therapy. (Level of Evidence: A)
CRT can be useful in patients with atrial fibrillation and LVEF less than or equal to 35% on guideline-directed medical therapy (GDMT) if (a) the patient requires ventricular pacing or otherwise meets CRT criteria and (b) atrioventricular (AV) nodal ablation or pharmacologic rate control will allow near 100% ventricular pacing with CRT. (Level of Evidence: B)
CRT can be useful for patients on GDMT who have LVEF less than or equal to 35% and are undergoing new or replacement device placement with anticipated requirement for significant (>40%) ventricular pacing. (Level of Evidence: C)
CRT may be considered for patients who have LVEF less than or equal to 30%, ischemic etiology of heart failure, sinus rhythm, LBBB with a QRS duration of greater than or equal to 150 msec, and NYHA class I symptoms on optimal medical therapy. (Level of Evidence: C)
CRT may be considered for patients who have LVEF less than or equal to 35%, sinus rhythm, a non-LBBB pattern with QRS duration 120 to 149 msec, and NYHA class III/ambulatory class IV on optimal medical therapy (Level of Evidence: B)
CRT may be considered for patients who have LVEF less than or equal to 35%, sinus rhythm, a non-LBBB pattern with a QRS duration greater than or equal to 150 msec, and NYHA class II symptoms on optimal medical therapy. (Level of Evidence: B)
CRT is not recommended for patients with NYHA class I or II symptoms and non-LBBB pattern with QRS duration less than 150 msec. (Level of Evidence: B)
CRT is not indicated for patients whose comorbidities and/or frailty limit survival with good functional capacity to less than 1 year. (Level of Evidence: C)
Permanent pacing is indicated for sinus node dysfunction (SND) or atrioventricular (AV) block in patients with hypertrophic cardiomyopathy (HCM) as described previously (see Section 2.1.1, “Sinus Node Dysfunction,” and Section 2.1.2, “Acquired Atrioventricular Block in Adults”). (Level of Evidence: C)
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here