Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pediatric critical care began with the pediatric intensive care unit (PICU) created by Dr. Jack Downes in 1967 at Children’s Hospital of Philadelphia, many years after the initial attempts to palliate or repair congenital cardiac anomalies ( ; ). The development of the dedicated PICU offered hope to critically ill children suffering from respiratory failure, sepsis, and trauma. For many years, there were no dedicated pediatric cardiac intensive care units (CICUs), as the field of pediatric cardiac surgery was rudimentary, and few of these patients survived because contemporary surgical and cardiopulmonary bypass (CPB) techniques had not yet been developed. Prior to the advent of dedicated pediatric CICUs, pediatric patients undergoing repair of congenital heart lesions were managed where circumstances permitted. Pediatric CICUs grew evolutionarily from these informal arrangements as the volume and specialized needs of this patient population became more fully manifest ( ).
This unique patient population extends from premature neonates who require ligation of a patent ductus arteriosus (PDA) to infants undergoing palliative repairs of single-ventricle physiology, and from adolescents undergoing cardiac or lung transplantation to adults with congenital heart disease. Pediatric CICUs have evolved into distinct areas of care within children’s hospitals with specialized nursing staff, respiratory therapists, and support services focused on the unique needs of children with congenital heart disease. Pediatric specialists from cardiac surgery, cardiology, intensive care, neonatology, and anesthesiology are all involved in the care of these patients ( ). Dedicated pediatric cardiac anesthesiologists care for these patients and their families during procedures in the cardiac catheterization lab, interventional radiology for long-term vascular access, MRI for cardiac and neuroimaging, and operating rooms. Some procedures are performed in CICU rather than the operating rooms, such as PDA ligation, emergency extracorporeal membrane oxygenation (ECMO) cannulation, or chest closure. Although the pediatric cardiac anesthesiologist may be most frequently involved with these patients, all pediatric anesthesiologists may be required to assist the team or care for the child in the CICU.
This chapter will explore the organizational structure of pediatric CICUs; aspects of patient monitoring commonly found in the CICU; perioperative intensive care of pediatric patients with heart disease; ventricular-assist devices; and special issues, including sedation, nutrition, postoperative complications, and family-centered care.
Distinctive aspects of pediatric CICUs include the age range of the patients, the chronicity of disease, the need for cardiac catheterization or operative intervention for palliation or repair, the mortal burden of some cardiac lesions, and the challenges confronting patients and their families. These patients also have complex cardiopulmonary interactions and the potential for rapid hemodynamic deterioration. Ideals of CICU care include multidisciplinary collaboration, a continuum of service, individualized anticipatory patient care, and gradual transitions ( ). Care has historically been delivered in diverse locations throughout the hospital, but the multidisciplinary nature and acute physiologic demands for such patients have spurred the centralization and integration of care ( ). Pediatric CICUs provide a structure for pediatric cardiologists, intensivists, and cardiothoracic surgeons to coordinate care. Physician and nursing leadership guides the team, streamlines care, and assures that clinical practice follows evidence-based standards. Physicians with specialized training and experience in the delivery of pediatric cardiac care should be tasked for leadership, although controversy exists between pediatric cardiologists and pediatric intensivists regarding the optimal training exposure ( ; ). Increasingly, fellowship programs offer dual training in pediatric cardiology and pediatric intensive care. The complexities of care, the relative paucity of evidence-based data guiding pediatric cardiac intensive care, and the intensities of emotional events converge to create a stressful work environment in the CICU, which makes it all the more necessary for leadership to promote professional performance and interactions and to be sensitive to the potential for providers to suffer from burnout ( ).
The CICU population consists of a mix of perioperative patients and those requiring medical management for cardiac disease. Neonatal patients with congenital heart disease may be admitted directly to the CICU or may be managed in the neonatal intensive care unit (NICU) depending on their degree of prematurity, the complexity of their cardiac disease, comorbidities, prognosis, and prevailing local practice. In the preoperative period, neonatal patients with minor congenital heart defects may be managed in the CICU so that the team is familiarized with the patient and better prepared for postoperative management. Neonates with ductal-dependent lesions for systemic or pulmonary blood flow require initiation of prostaglandin E1 (PGE 1 ) and monitoring in the CICU for apnea, fever, and hypotension from vasodilation, as well as adequacy of mixing. Critically ill patients of any age with congenital or childhood-acquired heart disease are directly admitted to the CICU at some institutions for definitive management ( ). These patients may present after emergent out-of-hospital decompensation, as transfers from other institutions, or for continuation of their postoperative care following surgery.
Perioperative intensive care of the patient with congenital heart disease is guided by the patient’s baseline physical status, their diagnosis, and the procedure being performed. Children at high risk of cardiac decompensation may require monitoring in the CICU following even minor procedures or routine cardiac catheterizations. Diagnoses that merit consideration for admission to the CICU due to their increased risk of cardiac arrest in the perioperative period include decompensated heart failure, Williams syndrome, unpalliated single-ventricle physiology, and pulmonary hypertension ( ; ). CICU bed availability and the need for backup mechanical support services should be verified prior to anesthetizing such children to alert the CICU team in the event such support is required postoperatively. In this section we will discuss the fundamentals of basic perioperative care following cardiac procedures, including transport, handoff, monitoring, pharmacologic support, sedation and analgesia, mechanical ventilation, nutritional support, and management of infection.
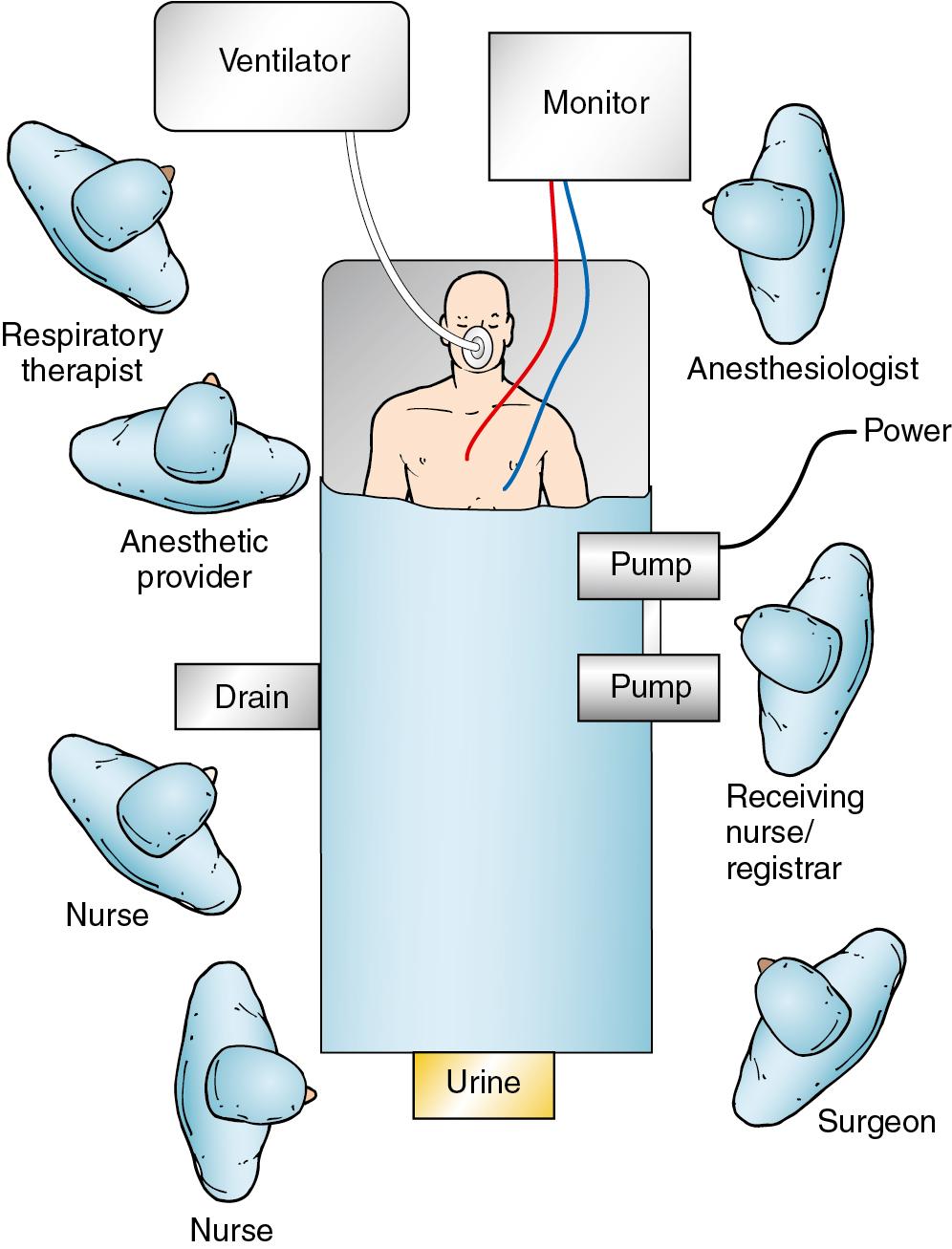
The postoperative period following surgical correction or palliation of congenital heart disease is accompanied by numerous potential complications, including hemorrhage, cardiac tamponade, arrhythmia, heart failure, and cardiac arrest. Patients with complex surgical corrections, redo surgeries, and patients with significantly compromised preoperative status have a higher risk of instability and require closer monitoring. Following the operation the anticipated complications are delineated at the patient handover by the surgeon and intensivist ( ). The transportation and transition from the cardiac operating room environment to the CICU is one of the most critical periods for the anesthesiologist, and this process should be well choreographed and systematic.
In the intensive care unit (ICU) a structured handover process significantly reduces the loss of critical information and improves select outcomes in the first 24 hours of postoperative pediatric cardiac care ( ; ). The standardized approach shares much in common with that used in other high-risk, time-pressured multidisciplinary team scenarios such as those seen in the aviation and professional auto racing industries ( ). Prospective studies in both pediatric and adult ICUs have shown improvement in efficiency ( ) and various safety outcomes ( ) when a structured protocol is used. Throughout this period the anesthesiologist retains management of the patient ( Fig. 59.1 ).
The format of this report will differ by institution but should begin with the patient’s name and demographics; a brief history, including the indication for surgery; other medical diagnoses; and the procedure performed. Details of induction method, airway management, and vascular access are conveyed. The anesthetic maintenance technique and the administration of any long-acting opioids are described. Intraoperative hemodynamic perturbations and their management are discussed, including the initiation and titration of vasoactive medications, cardioversion/defibrillation, need for repair of residual lesions, or inability to separate from bypass without extracorporeal support. An account of fluids and blood products administered is provided. Finally, the most recent administration times of opioids, sedative-hypnotics, neuromuscular blockers, antibiotics, and current rates of vasoactive medication infusions are given, as well as most recent arterial blood gas (ABG), hematocrit, and relevant coagulation assays.
The surgeon describes the operative approach in detail, including the cannulation strategy, the actual procedure performed (which may differ fundamentally from what was planned), and the specifications of any prosthetic material placed such as grafts, conduits, or valves. Details of drainage tubes, pacing wires, and any intracardiac monitoring catheters are provided. For cases involving the use of CPB, the duration of bypass, aortic cross-clamp or ischemic times, and any period of circulatory arrest should be reported. The key findings from intraoperative transesophageal echocardiograph (TEE) examination are discussed, including the presence of residual shunts, valvular regurgitation or stenosis, gradients, or impaired function. The surgeon should conclude with any specific postoperative concerns, as well as hemodynamic targets indicated by the patient’s repair and physiology.
The intensivist should conclude the handover process with a focus on repeating significant events, outlining plans for immediate care, including ventilatory strategy, extubation readiness preparation, titration parameters for vasoactive support, cardiac pacing, plans for continued sedation and analgesia, and a rational schedule for laboratory and point-of-care testing. As dictated by the operation, a plan may be needed for anticoagulation, early renal replacement therapy, and immune suppression.
Standard management of PICU patients includes continuous monitoring of oxygenation, ventilation, circulation, urine output, and temperature. CICU patient monitoring routinely includes five-lead electrocardiogram (ECG), ST-segment monitoring, noninvasive blood pressure, and capnography for intubated patients ( ; ). In cyanotic neonates, preductal and postductal oxygen saturation is typically monitored. Postoperative care includes monitoring of output from chest tubes, Foley catheters, and peritoneal drains. Mixed venous saturation and serial lactate measurements can help identify decreased cardiac output. Serial lactate levels have been demonstrated as a predictor of death or the requirement for ECMO following neonatal repair of complex congenital heart disease ( ). Near-infrared spectroscopy (NIRS) is frequently used to follow regional cerebral and renal saturation to estimate oxygen extraction and trend cardiac output ( Box 59.1 ). Increasingly, continuous electroencephalography (EEG) in the neonatal period is being used in the immediate postoperative period due to the significant risk of subclinical seizures after CPB ( ).
Peripheral temperature/core temperature gradient
Capillary refill time
Pulse and blood pressure
Blood pH, base deficit, and lactate
Urine output
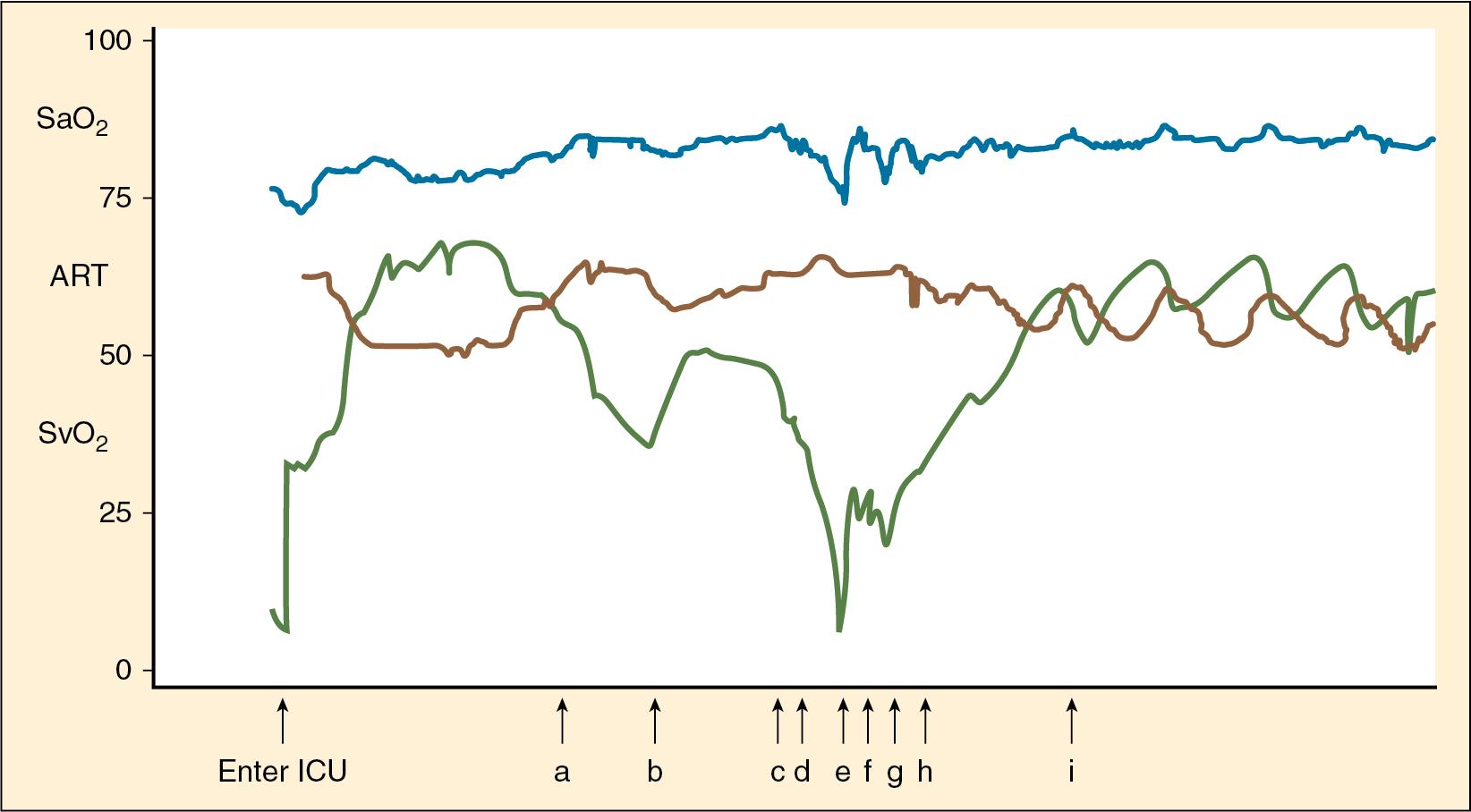
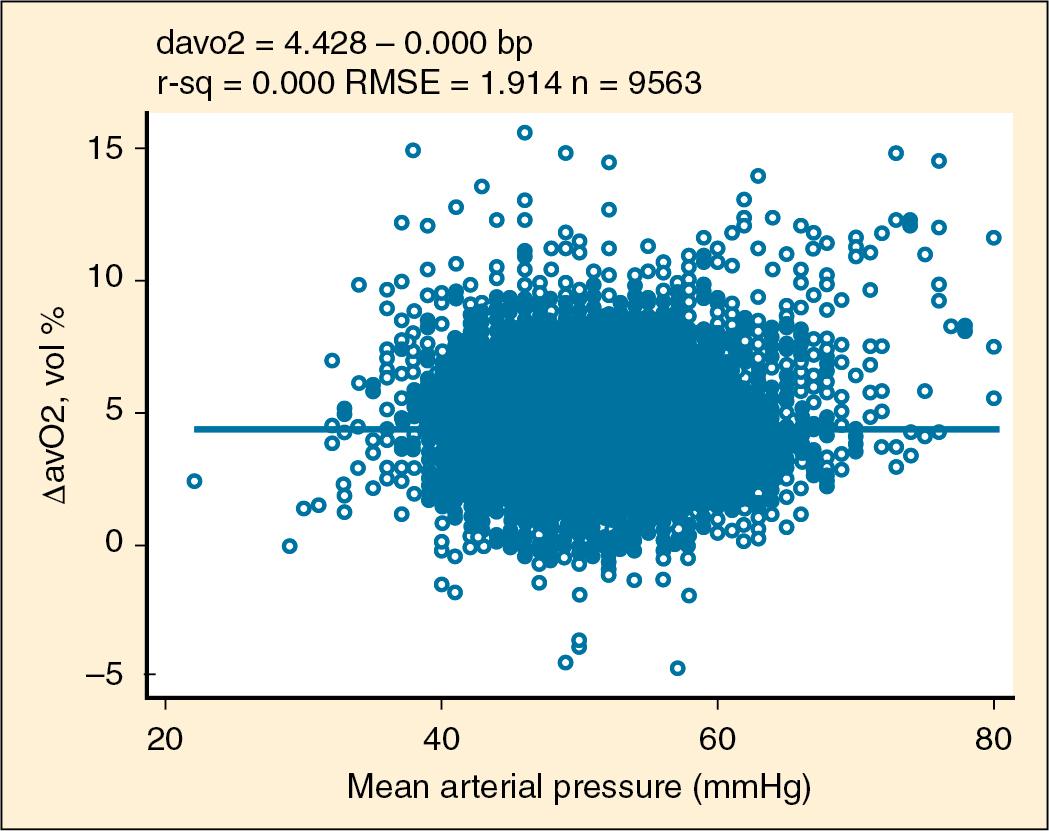
Invasive monitoring is a vital aspect of CICU care to supplement and guide a clinician’s findings on physical examination. Invasive monitors used in the CICU include peripheral and central arterial lines, umbilical arterial and venous catheters, central venous lines, pulmonary arterial catheters, and right and left atrial lines directly placed during surgery. The evidence to support currently used standard monitoring is based on expert opinion, case studies, and consensus guidelines from professional societies. Caution must be exercised, as the measured blood pressure may be preserved despite developing circulatory failure ( Fig. 59.2 ) ( ; ). Many clinicians are confident in their ability to estimate cardiac output by following clinical indicators, including physical exam findings, hemodynamic parameters, and lab values ( ). However, there is a poor correlation between a clinician’s estimate of cardiac output and measured femoral artery thermodilution ( ; ). Similarly, there is a poor correlation between traditional assessment of capillary refill and core-peripheral temperature gap and hemodynamic status ( Fig. 59.3 ) ( ). The goal of monitoring is to manage oxygen transport balance and optimize oxygen delivery ( ), and in the CICU this task is complicated by the predictable poor ventricular function following CPB and cardiac surgery ( ).
Pulmonary artery catheters (PACs), commonly used in adult cardiac critical care, are used far less often in the pediatric CICU to determine cardiac output and assure adequate oxygen delivery. The evidence supporting the use of PACs is primarily restricted to level 4 (nonrandomized and historical controls) and level 5 (case series, uncontrolled studies, and expert opinion) data. Select pediatric patient groups, such as those with pulmonary hypertension or refractory shock, may benefit from PACs. There is no evidence that PACs increase mortality in children. The PAC should be used sensibly and for the shortest time necessary in children ( ). Due to their relatively infrequent use in the pediatric CICU, practitioners must be particularly cautious in calibrating and measuring with the PAC and interpreting the data obtained in children.
A preferred method of monitoring would be a noninvasive measurement of cardiac output and oxygen delivery that is reproducible and easy to perform ( ). Beyond the PAC, there are alternative hemodynamic monitoring systems. Calibrated pulse contour analysis devices such as the Pulse Index Continuous Cardiac Output (PiCCO) and the Lithium Dilution Cardiac Output (LiDCO) require arterial and central venous access. The PiCCO is not reliable in patients with intracardiac shunts, limiting its use in many patients with complex congenital heart disease. Vigileo is a noncalibrated pulse contour analysis device that requires arterial access and has not supplanted the PAC. Other techniques such as Doppler ultrasound, pulse dye densitometry, and thoracic electrical bioimpedance are not supported by evidence for their validity in young patients with congenital heart disease to be widely accepted. Presently, the PAC remains the gold standard for invasive hemodynamic monitoring ( ).
Near-infrared spectroscopy (NIRS) detects absorption in nonpulsatile tissue generating a regional oxygen saturation (rSO 2 ) reflecting the saturation of capillary-venous and, to a lesser extent, arterial blood. The cerebral rSO 2 correlates well with the jugular venous bulb saturation, particularly in smaller infants weighing <10 kg ( ). While the absolute NIRS value is not reliably predictive of tissue oxygenation, the trend of the rSO 2 can be an important indicator of tissue oxygen consumption, particularly when accompanied with serial lactates, and has been shown to be predictive of postoperative low cardiac output state ( ). Intraoperative cerebral oxygen desaturation has been associated with a significantly increased risk of postoperative cognitive decline and increased length of hospital stay in adults following CPB ( ). Using rSO 2 monitors in two sites, cerebral and somatic renal, is suggested as a means of monitoring global and regional perfusion in high-risk patients ( ). Being noninvasive, NIRS is widely used, but caution is advised because there remains no level 1–based evidence that NIRS improves patient outcomes ( ; ).
Of primary importance in the care of postoperative cardiac surgical patients is ensuring adequate tissue oxygen delivery (DO 2 ). DO 2 can be calculated directly if accurate measurement of cardiac output can be made. However, this is not done routinely in neonatal and pediatric patients, due to the technical challenges with PAC placement in small patients and the impact of intracardiac shunts on thermodilution methods. A more clinically relevant parameter is the central venous oxygen saturation (ScvO 2 ), which is reflective of the balance between oxygen uptake and delivery. The ScvO 2 , and the arterio-venous oxygen difference derived from it, require either continuous invasive oximetric measurement or intermittent sampling, and reflect global oxygen balance. What may be of more clinical value is the status of regional oxygenation in critical tissues, namely, the brain and visceral organs.
If oxygen consumption (VO 2 ) is constant, a decline in ScvO 2 must by definition indicate a fall in oxygen delivery, usually from a reduction in cardiac output or regional blood flow. NIRS uses a noninvasive disposable sensor to measure the light absorbance spectrum in chromatophores, namely, hemoglobin. The ratio of oxyhemoglobin to deoxyhemoglobin is reflected in the regional oxygen saturation, or rSO 2 . Several studies have shown rSO 2 to correlate with ScvO 2 in postoperative pediatric patients from procedures using CPB ( ; ). Therefore as a continuous, real-time monitor, NIRS has the potential to serve as an early warning marker of dysoxic states. It should be noted that other investigators have found a lack of tight correlation between absolute values, but rather a concordance of relative trends in rSO 2 and ScvO 2 . Furthermore, correlation is found between Paco 2 changes and changes in cerebral rSO 2 but not somatic rSO 2 , highlighting the complex effects of CO 2 tension on cerebral vasoregulation, a concept of great importance in the management of infants with superior cavopulmonary anastomoses ( ).
NIRS probes are routinely placed in both cerebral (over forehead off midline) and somatic (on flank over kidney) locations, to afford surveillance of regional oxygen delivery to brain and abdominal viscera. Intraoperatively, this can serve to assess adequacy of DO 2 while on CPB, especially useful when low-flow and/or hypothermic arrest techniques are employed, as in complex neonatal palliations. In the immediate postoperative period, NIRS has been shown to predict hyperlactatemia ( ), suggesting its utility in identifying hypoperfusion states. Finally, neurodevelopmental outcomes following neonatal cardiac surgery can be correlated with perioperative NIRS thresholds ( ), a finding of great importance as more children survive their initial repair and confront the reality of subsequent neurocognitive impairment.
Children with congenital heart disease are at increased risk of neurologic injury that can occur prenatally, preoperatively, intraoperatively, or postoperatively ( ). Some institutions monitor the brain intraoperatively with EEG and transcranial Doppler ( ). EEG monitoring is indicated and used for patients with suspected seizures in the postoperative period, particularly for those who are maintained under neuromuscular blockade. Its use in the neonatal period after cardiac surgery in currently being studied. Ultimately, bedside monitoring is needed to guide clinicians as they attempt to optimize oxygen delivery to tissues. Monitors are not a replacement for serial clinical examinations, for review of vital sign trends, or for communication with nurses, respiratory therapists, and parents who, as bedside providers with direct patient contact over time, can provide insight into a patient’s trajectory.
The perioperative care of the patient with congenital heart disease requires precise manipulation of preload, rate, rhythm, contractility, and afterload to ensure adequate cardiac output and organ perfusion. Pharmacologic circulatory support is a dynamic process, guided by both the clinical exam and hemodynamic monitoring, and should not simply be empiric. Although there will be some institutional variance in practice, what follows is an overview of the indications, pharmacodynamics, and off-target effects of commonly used vasoactive drugs in the pediatric CICU.
Inotropic drugs improve myocardial contractility and are used to increase cardiac output. The primary indications are low cardiac output states or heart failure, where intrinsic ventricular dysfunction is the dominant problem. This commonly occurs in the immediate postoperative period where the effects of CPB, and specifically myocardial ischemia from aortic cross-clamping, lead to compromised ventricular contractility. More chronically, these drugs are used in decompensated heart failure to support circulatory function while awaiting recovery, mechanical device support, or transplant. Although many drugs have mixed inotropic and vasoactive effects, the following is a discussion of pure inotropes.
Isoproterenol is a synthetic sympathomimetic with both β 1 - and β 2 -adrenergic effects. The net hemodynamic effect is to increase the heart rate from β 1 stimulation of intrinsic pacemakers as well as β 2 -mediated vasodilation; this results in increased systolic blood pressure, with reductions in diastolic and mean pressure. Its historical use was primarily as a bronchodilator prior to the availability of aerosolized albuterol. Current pediatric uses have been to manage severe bradycardia in beta-blocked children in shock ( ) and in congenital complete heart block as a bridge to pacemaker ( ). It is also employed in the catheterization lab in provocative electrophysiology protocols aimed at inducing tachyarrhythmias ( ). The major side effect is tachycardia-induced increased myocardial oxygen demand, which may be deleterious in patients with ischemic myocardium. Dosing is typically between 0.05 and 0.5 mcg/kg per minute.
Dobutamine is a synthetic sympathomimetic structural analog of isoproterenol. It is a racemate, with the (+) isomer having mixed potent β 1 and weak β 2 effects, and the (−) isomer having α 1 effects. The net effect is positive inotropy and chronotropy; systemic blood pressure effects are variable and unpredictable, although hypotension may occur due to β 2 -mediated vasodilation in patients with suboptimal volume status. Its indications are low cardiac output states with elevated systemic vascular resistance (SVR), and normal or elevated filling pressures. Prior to the widespread use of milrinone, dobutamine was used perioperatively to support cardiac output after CPB ( ) and in decompensated heart failure ( ). Chronotropic effects, which are less intense than isoproterenol, may lead to ischemia from increased myocardial oxygen consumption. It is typically dosed between 1 and 10 mcg/kg per minute. Dobutamine has indications for use in pediatric stress echocardiography in less mobile children in whom exercise stress testing is unable to be performed, or when segmental wall motion abnormalities are suspected.
Milrinone belongs to a class of drugs known as phosphodiesterase inhibitors (PDEIs), which increase cyclic AMP, increase activation of protein kinase A, and lead to widespread phosphorylation of cardiomyocyte calcium channels and myofilaments. The net effect is increased contractility, diastolic relaxation, and peripheral vasodilation; for this reason, the drug is referred to as a lusitropic inodilator. Milrinone has salutary effects on hemodynamics following pediatric cardiac surgery, lowering filling pressures and improving biventricular performance ( ). It is established that adrenergic receptors may be downregulated in chronic pediatric heart failure ( ). As the mixed actions of milrinone are independent of adrenergic receptor activity, milrinone may be especially useful in these patients. It is also a potent pulmonary vasodilator, adding to its utility in situations where right ventricular dysfunction predominates. Side effects include platelet inhibition, reversible thrombocytopenia, and tachyarrhythmias. The drug is renally cleared with a long elimination half-life, and toxicity may develop in patients with impaired renal function. Dosing is usually between 0.25 and 1 mcg/kg per minute, with or without a loading dose. Other lusitropic inotropes such as levosimendan and istaroxime have not been rigorously evaluated in children.
Vasopressors act to increase arterial blood pressure via either adrenergic or hormonal mechanisms. Many of the catecholamines in this category have inotropic effects as well; the dominant effect is dose related. The primary indication for all of these agents is to increase mean arterial blood pressure and restore adequate perfusion pressure to vascular beds of vital organs, where loss of autoregulatory control may lead to conditions of pressure-dependent flow. The target blood pressure goal must be individualized and established in context and correlated with other markers of adequate perfusion. The vasopressors discussed are ordered from highest to lowest degree of pure α 1 activity.
Phenylephrine is a synthetic sympathomimetic with vasoselective α 1 activity. It is used to increase mean arterial blood pressure in vasodilated hypotensive patients. While its use is common in the operating room to restore blood pressure during transient hypotensive episodes occurring after anesthetic induction, it has limited use in the pediatric CICU. One notable exception is in patients with Williams syndrome phenotype who have diffuse elastin arteriopathy and often coronary stenosis ( ; ). In these patients, hypovolemia and diastolic hypotension can compromise coronary perfusion markedly, especially in the presence of ventricular dysfunction with subsequently elevated ventricular end-diastolic pressure (EDP). The most common side effect of this drug is a reflex baroreceptor-mediated bradycardia, which can be used to terminate paroxysmal supraventricular tachycardias ( ). Other indications may include the patient with tetralogy of Fallot (TOF) hypercyanotic spell, Blalock-Taussig (BT) shunt thrombosis, or any other scenario during which an increase in SVR is needed to drive pulmonary blood flow. The drug is typically given as a bolus of 1 mcg/kg or by continuous infusion between 0.5 and 6 mcg/kg per minute.
Norepinephrine is an endogenous catecholamine that functions as an adrenal medullary hormone and sympathetic nervous system neurotransmitter. Its adrenergic effects are α 1 predominant with lesser β activity. The net hemodynamic effect is vasoconstriction, with increases in SVR and blood pressure, although heart rate and contractility can also be increased. As such, it is an appropriate choice when vasoplegia is accompanied by normal to low heart rate. As with phenylephrine, this drug is useful in hypotensive distributive or vasodilated conditions, as may occur following CPB, protamine administration, septic shock, anaphylaxis, and adrenal crisis. The intense vasoconstriction mediated by its α 1 effects can be deleterious to splanchnic and renal perfusion, potentially leading to ischemic injury at high doses. The typical dosing range is between 0.02 and 1 mcg/kg per minute.
Dopamine is an endogenous catecholamine and the metabolic precursor of both epinephrine and norepinephrine. Its mixed adrenergic and nonadrenergic effects are dose dependent and difficult to predict. At doses between 0.5 and 4 mcg/kg per minute, the dominant effect is at the dopaminergic receptors, resulting in splanchnic and renal vasodilation. Evidence supporting historical use at low doses to augment renal blood flow has been largely discredited due to lack of improvement in outcome ( ). At doses between 5 and 10 mcg/kg per minute, it acts as a mixed β 1 and α 1 agonist with positive chronotropic and inotropic effects. At doses between 10 and 15 mcg/kg per minute and higher, the drug’s action is α 1 predominant, leading to increased systemic resistance and blood pressure. In the CICU, standard indications are to increase contractility in situations of low output. As with all catecholamines, dopamine can lead to tachycardia and has arrhythmogenic potential. It also has potentially deleterious immunomodulatory ( ) and endocrine effects ( ).
Epinephrine is an endogenous catecholamine, and like norepinephrine it functions as both a hormone and neurotransmitter. It has mixed α and β activity, the dominant effect changing with dose range, similarly to dopamine. The net effect is dose dependent but typically will increase both contractility and systemic resistance. Vasoconstriction predominates in all but the lowest dose range, often necessitating the concomitant use of vasodilators. Common clinical uses are in low cardiac output states with hypotension. It is also a first-line drug for bolus delivery in pulseless arrest to augment diastolic blood pressure and restore coronary perfusion. Significant metabolic effects can be seen, notably lactic acidosis ( ) and hyperglycemia from β-mediated stimulation of glucagon secretion ( ). The dose range is typically between 0.02 and 0.5 mcg/kg per minute.
Vasopressin is a noncatecholamine pituitary peptide hormone. Its pharmacologic effect is mediated via V 1 receptors in the vascular smooth muscle leading to a direct pressor response. This effect is preserved even in catecholamine-depleted states or when severe acidosis or hypoxia has rendered adrenergic receptors unresponsive to catecholamines. Additional mechanisms of action are nitric oxide inhibition and stimulation of endothelin-1 synthesis. It is commonly used as a second-line vasopressor in catecholamine-resistant septic shock. Its nonadrenergic mechanisms make vasopressin especially useful in profound refractory vasoplegic syndromes that may occur after CPB, often in patients with endogenous vasopressin depletion ( ; ). Its renovascular effects are paradoxical; although it is an antidiuretic, the V 1 effect is selective for the efferent glomerular arterioles, promoting increased renal blood flow. There is also evidence that vasopressin may lower pulmonary vascular resistance (PVR) by causing V1 receptor–mediated release of nitric oxide in the pulmonary artery (PA) endothelium, and therefore may be used for increasing pulmonary blood flow in pulmonary hypertensive crises ( ). Dosing for vasopressin in cardiopulmonary shock is by continuous infusion, ranging from 0.2 to 2 mU/kg per minute.
The principle use of vasodilator infusions is to lower systemic and/or pulmonary resistance in order to decrease impedance to ventricular ejection and augment cardiac output. The drugs in this category have variable effects on both arteriolar resistance vessels, which can reduce afterload, and venous capacitance vessels, which lower preload. Both actions are salutary in decompensated heart failure. The other common indication for systemic vasodilators is to control systemic blood pressure when hypertensive increases in EDP can lead to worsening atrioventricular (AV) valve insufficiency and precipitate pulmonary edema. Drugs in this category are chosen for CICU use based on rapid titratability and short duration of action.
Nitroprusside is a vasodilator that acts as a nitric oxide donor. Liberation of nitric oxide stimulates guanylate cyclase to increase cyclic guanosine monophosphate (GMP) levels, in turn activating protein kinase G and leading to protein phosphorylation. In the peripheral vasculature, this leads to vasodilation. Arteriolar effects exceed effects on the venules. The combined effect of increased venous capacitance and reduced arteriolar resistance leads to a reduction in filling pressure and afterload, which makes the drug ideal for patients in acute heart failure. In low cardiac output states with normal to high blood pressure, nitroprusside lowers blood pressure but improves perfusion and indices of oxygen delivery. It is also used to rapidly manage malignant hypertension in patients with normal ventricular function, often as a bridge to more stable enteral alternatives. It has a long-standing record of utility in the ICU ( ). Nitroprusside dosing is between 0.5 and 5 mcg/kg per minute. Like all vasodilators, it should be used with caution in patients with left-sided obstructive lesions and compensatory hypertension such as aortic stenosis or aortic coarctation, where the net effect may be decreased systemic resistance and hypotension without an effect on left ventricular afterload. Nitroprusside breakdown liberates cyanide, which is converted to thiocyanate in the presence of vitamin B 12 and thiosulfate. If this process is overwhelmed, cyanide toxicity can ensue and lead to histotoxic hypoxia, heralded by acidosis and rising mixed venous saturations. Infants are particularly vulnerable, and treatment is with sodium thiosulfate / sodium nitrite rescue ( ).
Nitroglycerin is another vasodilator, which is metabolized to nitric oxide and exerts effects similar to nitroprusside, although with venous predominance. Its use in the CICU is for similar indications. It also acts as a coronary vasodilator and can be administered by direct intracoronary injection in the management of coronary artery spasm from coronary angiography in the catheterization lab ( ). Nitroglycerin has also been used to treat ischemic events in children with Kawasaki disease ( ) and as adjunctive agent to reverse coronary vasoconstriction in infants following arterial switch operation ( ). The dose range is between 0.25 and 5 mcg/kg per minute.
Nicardipine is a dihydropyridine calcium channel blocker used primarily as a vasodilator in hypertension and ischemic events. Unlike calcium channel blockers in the nondihydropyridine class, which exert direct negative inotropic effects, nicardipine is relatively vasoselective, with more selectivity for coronary and cerebral vasculature than other calcium channel blockers in its class. It does not lead to the reflex tachycardia and is free of significant side effects. For this reason it is an optimal choice in hypertensive patients for whom nitrovasodilators are either contraindicated or ineffective. It has been used with good safety and efficacy in pediatric postcoarctectomy patients ( ) and following cardiac transplantation ( ). Nicardipine dosing is between 0.5 and 3 mcg/kg per minute.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here