Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Disclaimer: The opinions or assertions contained herein are the private views of the authors, and are not to be construed as official or as reflecting the views of the Department of the Army or the Department of Defense.
Mass casualty events and disasters are marked by a period of mismatch (disproportion) between supply and demand. Rescue organizations must work to reduce the duration of this period of mismatch. During the acute phase, actions follow the principles of disaster medicine : The goal is to save as many lives as possible even if it means postponing care for an individual patient. After the mismatch between supply and demand has been addressed, the principles of individual medicine can be restored. One goal in mass casualty care is to minimize the period of time it takes to restore care to the individual medicine paradigm. This period's length depends on such structural aspects as the existence and validity of a disaster plan, a regard for disaster capacity in health planning, and the educational level of medical services. These facts are often neglected in disaster planning, from the political aspect of planning and from the practical aspect of disaster capacity.
Ideally, treatment should be based on the state of the art in medical science. During a disaster, treatment with the “best available means” may weaken the quality of care for individuals. Therefore, in mass casualties and disasters, the infrastructure of a country or region may be unable to cope with a higher number of victims of special trauma types while maintaining the state of the art. When it is predictable that the state of the art cannot be maintained in a jurisdiction because of dwindling resources, help from other jurisdictions must be planned and coordinated—the time for international cooperation has come! Such instances include mass casualties with burn injuries. Resources available for specialized treatment are limited, but the demands of state-of-the-art treatment are high, meaning that even a small number of victims from one accident can push an area's or country's burn treatment system to its limits.
The purpose of this chapter is to introduce concepts of disaster medicine as applied to burn patients. A glossary of disaster medicine terms is provided. Examples of major burn disasters and the lessons learned are described. Phases in the typical response to a disaster are summarized. Special aspects of emergency care during a disaster are discussed. The role of communication in disaster response is detailed. The strategic approach to matching burn resources and patients is considered. Finally, the special case of humanitarian crisis response is discussed. Every disaster we have studied is somewhat different. There is, however, a common theme running through all of them: Prior planning and realistic training are essential to success.
A shared language is critical for the process of planning for and responding to a disaster. The following provides a basic vocabulary for burn mass casualty and disaster response.
Mass casualty event: an emergency in which there is a greater number of victims than can be accommodated by the rescue forces and their supplies. Infrastructure in the affected area is intact. With force mobilization, the crisis can be mastered. The period of mismatch between supply and demand is short. The goal is to reestablish treatment according to principles of individual medicine as quickly as possible and without transferring the supply–demand mismatch from the scene to hospitals. The challenge to save as many lives as possible, even disregarding the medical needs of an individual, stands in contrast to the paradigms of individual medicine in which any individual life claims the maximum medical effort. The procedure for this challenge is selection of patients—triage, based on urgency of medical procedures, chance of success, and distribution among the available qualified treatment centers (see later discussion).
Disaster: an event in which infrastructure is at least partly destroyed or degraded and that cannot be handled by regional rescue means alone. The first goal is to reestablish the minimal level of infrastructure required to provide basic medical care. (This is different from mass burns treatment in a resource-poor country, where infrastructure never existed.) One way to treat burns successfully in a disaster is to bring infrastructure, staff, and materials to the area to treat burns. Another is to move victims to a place with existing infrastructure. The maximum treatment possible locally is determined by the degree of infrastructure and resources in, or brought to, the disaster area.
Although mass casualty events remain in the purview of local rescue organizations, disasters are for regional or national authorities. This means different ways of handling the situation and different funding resources.
Mass burn casualty disaster: defined by the American Burn Association (ABA) as “any catastrophic event in which the number of burn victims exceeds the capacity of the local burn center to provide optimal burn care.” Capacity includes the availability of burn beds, burn surgeons, burn nurses, other support staff, operating rooms, equipment, supplies, and related resources. This definition is inapplicable where, as in Germany, a central burn-bed bureau always organizes the distribution of burn victims; the definition supposes a very different degree of preparedness in these countries.
Triage: the process of sorting individual patients into categories according to priority of treatment. An example of triage categories is delayed, immediate, minimal, and expectant (DIME). Several factors influence triage decisions; these include available resources, number of patients, the severity of injury of each patient, and the timeframe during which the injuries must be addressed. Triage is not a one-time event, but it should be repeated throughout the mass casualty event (see later).
Basic capacity: the normal number of patients who can be treated, based on the availability of burn beds, burn surgeons, burn nurses, other support staff, operating rooms, equipment, supplies, and related resources
Capacity utilization: the degree of utilization of burn beds in a center over a certain time. This should be expressed as use of intensive-care burn beds and other beds. The average value over a year gives an overview of a burn center's disaster capacity.
Actual capacity: the number of burn patients that a center can admit on an actual day. It varies daily, can depend on the season, and is likely to fluctuate with seasonal or accidental presence or absence of severe patients.
Surge capacity: the increased capacity available in mass casualties and disasters. In burns, it is defined by the ABA as the capacity to handle, in a disaster, 50% more than the normal maximum number of burn patients. Surge capacity must be developed and maintained, requiring action by health systems. Surge capacity must include continued medical care for all other patients. Elective medical and surgical care can be postponed temporarily to maintain surge capacity. When capacity is breached, patients must be transferred safely to other treatment facilities.
Sustained capacity: the maximum capacity that a burn center can sustain over a longer time without lowering treatment quality.
Burn capacity of a health system: the total capacity of burns that can be treated in a national health system. This capacity should be known; it should take into account the various requirements of burn treatment, such as the number of victims needing intensive care. The average capacity utilization over the year is part of resource planning for a health system.
Time to establish surge capacity: how much time a burn center needs to rise to maximum surge capacity. A good parameter is the number of complete burn teams available at various hours. This number is highly important in a hospital's organization of care.
National Disaster Medical System (NDMS): manages a country's national medical system in disasters. In the United States, the NDMS is a function of the Federal Emergency Management Agency (FEMA) under the Department of Homeland Security. It acts as a partner of the U.S. Department of Health and Human Services (HHS), the Department of Defense (DoD), and the Department of Veterans Affairs (VA). Other countries' structures are comparable. The U.S. NDMS has three functions: (1) medical response at the disaster site, (2) transport of patients to unaffected areas, and (3) definitive medical care in unaffected areas.
Burn specialty team (BST) or burn assessment team (BAT): a special form of disaster medical team that provides expertise in burns. In the United States, a BST consists of 15 burn-experienced medical and nonmedical staff. These teams do not exist in many countries. Such teams can be formed only when burn experts are numerous enough and not already engaged in other aspects of disaster response.
Technical relief: the general “civil defense” functions required to support disaster response. In Germany, these functions are provided by the Bundesanstalt Technisches Hilfswerk and include lighting, debris removal, search and rescue, flood mitigation, electricity, water supply, sewage disposal, catering, command center support, communications, logistics, equipment repair, and transportation of supplies. In the United States, these functions are provided by FEMA or by equivalent agencies at the state and local levels.
Even with the best preparation, a disaster remains a disaster for a certain period; the goal is to minimize that period. Although retrospectively correcting problems is impossible, lessons learned from the past should be applied to the future. Recurring themes that appear in the following case studies include the following:
Communication problems
Need to send major burn patients to burn centers
Need for central incident command post
Movement of patients to hospitals by private vehicles
Importance of control of traffic leaving the disaster area
Lack of coordination of patient evacuation from the scene
Value of retriage out of the disaster area to other burn centers
Infection control problems; multidrug-resistant organisms
Lack of experience in burns by nonburn providers
Need for psychological support of providers
Value of international teamwork
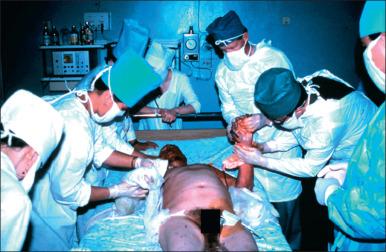
In New York, two hijacked airliners were flown directly into the Twin Towers of the World Trade Center. Although many were injured or killed, few survivors had severe burns. The victims were sent mainly to two burn centers, although more centers were easily reachable. Nineteen were seen at New York Presbyterian Hospital; there, the victims' average age was 44 years, and the burn size averaged 52.7%. In total, 39 burns were reported by nine hospitals; 27 patients were admitted. Although enough burn beds within 1 hour's transport were available, only 26% of burned patients were triaged first to burn centers. Two thirds of burn injuries were ultimately treated in a burn center. The usual portion of burn victims triaged to burn centers in New York City in a year is 75.2%. BST-1 from Boston, Massachusetts, responded to this event within hours ( Fig. 5.1 ).

A suicide bomber detonated a backpack bomb in a nightclub. People fled to the outside, where a car bomb exploded. There were 202 deaths and an additional 209 injured. The Australian Defence Force (ADF) initiated Operation Bali Assist, the largest Australian aeromedical evacuation since the Vietnam War. An aeromedical staging facility (ASF) was prepared in a Bali airport hangar, whence 5 C-130 planes flew 61 Australian patients to Royal Darwin Hospital (RDH). Of the 61 patients, 28 had major injuries (Injury Severity Score >16). At RDH, 55 escharotomies were performed, along with 43 other surgical procedures. Three patients had been intubated in Bali; 12 more were intubated at RDH. Within 36 hours after first admission to RDH and 62 hours after the bombing, 48 patients were evacuated to burn centers. There were no “walking wounded.” BATs were used for initial care at RDH.
Eleven patients were transferred to Concord Repatriation General Hospital. Burn injuries ranged from 15% to 85% total body surface area (TBSA), mostly full-thickness burns. All patients showed injuries from both the first and second blasts. There were complications from infections with Acinetobacter baumannii and Pseudomonas aeruginosa and from fragment injuries. Many ophthalmic injuries occurred, some being detected only later.
Royal Darwin Hospital received its first information about the incident from a patient who had been treated in Bali and then fled to Australia. The hospital learned nothing of the number of patients or the severity of injuries before the first wave of patients arrived. Palmer et al describe a need for improvement mainly in military–civilian communication. Communication in the hospital also was problematic: Mobile phones had no reception, there was no time to read electronic texts, and land lines were not mobile. ADF provided satellite phones to the medical staff for communication between the hospital in Bali and ADF.
Bomb attacks on four commuter trains killed 191 and injured 2051 of 6000 persons present. Thirteen bomb bags each contained 10 kg of dynamite plus fragments. Three bombs failed to explode. Of the 191 dead, 175 died instantly, and 16 died later. It was not known that unexploded bombs remained on the trains while ambulance staff worked. Ambulance staff worked without coordination and were oblivious to overall medical priorities. Patients with only minor injuries were transported. Ambulances ran out of all medical supplies. No joint field medical command post was set up.
Patients were taken to 15 hospitals in Madrid and two field hospitals, ranging from 5 to 312 patients each. Communication problems in hospitals and among organizations arose. Only 33% of patients were transported in ambulances under medical control; 67% found their way to hospitals without triage and medical or organizational control. Most went to the nearest hospital, which received patients with both serious and minor injuries. Of 312 patients taken to Gregorio Marañón University General Hospital, 45 had burns. The most common injuries were tympanic perforation (in 41%), chest injury (40%), fragment injury (36%), extremity fracture (18%), eye injury (16%), head injury (12%), abdominal injury (5%), and amputation (5%).
Four bombs in the transit system killed 56 (53 at the scene) and wounded 775. Train bombs exploded in three locations; the fourth bomb exploded on a double-decker bus. The number of explosion sites was initially unclear because passengers left the subway at various exits. Triage was performed; 55 patients were classified as severely wounded (P1 and P2). Communication was difficult: All but one mobile-telephone network failed; radio communication between the scenes and ambulance control was very difficult. The fire brigade established an inner cordon and ascertained that there were no signs of chemical substances threatening the rescuers, but the presence or absence of more bombs was not confirmed before rescue work began. Patients mainly in triage groups 1 and 2 were transported to six university hospitals after minimal triage and treatment.
Fire in an overcrowded discothèque during a Halloween party killed 61 teenagers at the scene; 2 died later; 235 were wounded ( Fig. 5.2 ). Initial information was poor, resulting in incorrect alerts. There was no triage officer at the scene. Hospital disaster plans in some cases were unknown or not implemented. Preexisting disaster plans had the same personnel simultaneously performing conflicting roles. Within 2 hours, 150 patients were admitted to four Swedish hospitals. Thirty-one patients presented with significant burn injuries; 11 patients were transferred secondarily to other burn centers in and outside Sweden.

Despite the initial chaos at the scene, there were timely escharotomies and triage in the hospitals before transfer to burn centers. Inhalation injuries were diagnosed in 158; 54 of them were treated simply with suction and expectorants. In 51 of 61 deaths, carbon monoxide (CO) was the cause. Eleven patients were transferred secondarily to burn centers in four other cities, one in Norway. All 11 had second- or third-degree burns of more than 20% of the TBSA.
A fire at a New Year's Eve party killed 8 and injured 203 of 350 present. An early error in directing emergency traffic caused transportation chaos. Emergency-services tents were insufficiently staffed, and tent placement was problematic. In all, 241 patients went to hospitals: 110 by ambulance, 18 by bus, and 113 by self-referral to the nearest hospital. Of 182 admitted, 112 went to intensive care units (ICUs). Nineteen hospitals provided initial care. The closest hospital, receiving 73 patients, was overwhelmed.
After primary treatment in the hospitals, burn specialists did tertiary triage, distributing patients to hospitals and burn centers in and outside the Netherlands. Burn center criteria were adapted on the basis of both burn extent and inhalation injury: The indications for burn center treatment were greater than 30% TBSA burn with inhalation injury.
Fire at The Station, a nightclub, killed 100 and injured 215 of 439 present. The building totally collapsed within 30 minutes. Rhode Island Hospital (RIH) first became aware of this incident from breaking news on television; shortly after, RIH got official notification that 200–300 burn victims were expected. A triage site was established. Sixteen area hospitals evaluated 215 patients. Patients admitted to RIH numbered 47. TBSA averaged 18.8%. There were 33 burns of less than 20% TBSA, 12 with TBSA of 21–40%, and 2 of greater than 40% TBSA. Of 32 patients presenting with inhalation injuries, 28 required intubation; 12 needed escharotomies; and in just 6 weeks, 184 bronchoscopies were necessary. Retrospective analysis called for improvement in communication with the disaster scene and in specific instructions for patient transport.
Fire at the overcrowded República Cromañón nightclub killed 194 and injured 714 of 3000 present. CO and hydrogen cyanide poisoning were the main causes of death. At the scene, 46 ambulances and 8 fire crews sent the victims to the 8 closest hospitals, which were overwhelmed by critically ill patients within 2 hours. In Buenos Aires city, 38 hospitals were engaged and another 5 elsewhere in Buenos Aires province.
Ramos et al describes the experience of Argerich Hospital, to which 74 patients were taken. All had inhalation injuries. There were no severe burn injuries. Eighteen patients (24%) were pronounced dead on arrival. Twenty-five showed respiratory insufficiency and reduced level of consciousness and were intubated. Initially, 22 patients were sent to the ICU; the 14 sent to the operating room for mechanical ventilation were transferred to other hospitals in Buenos Aires Province within 48 hours.
In this fire, 242 people were killed, and more than 630 others were wounded because of the use of fireworks. Firefighters had to create a hole in the outer wall to help people to escape. From the estimated 1200–1300 people present in the disco, 169 were hospitalized because of inhalation injuries and burns. The extent of the disaster was not communicated to the response workers. Triage was hindered by crowded bystanders and victims. The military police had to hinder relatives from entering the disaster site that was filled with smoke and toxic gases. Many of them were in critical conditions, emergency departments (EDs) of 5 hospitals, and ICUs of 6 hospitals, and all of the emergency units were crowded. Fifty-four patients had to be transported by helicopters and ground transport to hospitals in Porto Alegre and Caxias do Sul and Cachoera do Sul and Canoas. Transport was supervised and coordinated by a Brazilian Air Force officer and the Brazilian government corporation responsible for operating the main commercial airports. The main issues were with command and control at the incident scene and the absence of a disaster plan.
Fire in the nightclub caused by fireworks during a show killed 26 on the spot, 38 died in hospitals, and 184 were injured. About 200–400 people present in the club were engulfed in a stampede when they realized there was fire. The fire started at 22:30, first and emergency call was sent over 112. The first ambulances arrived 12 minutes later. A field hospital was set up. Resuscitation of the unconscious was tried; the effect was not described. At 23:30, the police isolated a perimeter of several streets around the night club. Seventy-five special vehicles of the Inspectorate for Emergency Situations and 57 SMURD trucks and ambulances were in place. A total of 500 emergency service personal were mobilized. Victims accessed hospitals driven by bystanders, taxis, and ambulances. Twelve hospitals received between 57 and 15 victims each, and some had to be redistributed to other hospitals because of overburdening. Ventilation devices had to be moved from other hospitals to the places they were needed. After 1 week, victims were distributed to burn centers in Israel, The Netherlands, Belgium, Austria, the United Kingdom, Norway, Germany, and France. Patients died during or immediately after the transport because of the severity of their injuries. In Bucharest, enzymatic debridement was used to reduce the logistic challenge. There were problems in identifying 29 of 146 hospitalized victims because of the severity of their burns. On March 14, 2016, the last victim treated in a Romanian hospital died.
A tanker truck carrying liquefied flammable gas exploded beside the Los Alfaques campground, killing 102 at the scene and injuring 288; eventually, the dead totaled 215 ( Fig. 5.3 ). The burning tanker divided the scene into two parts. The 58 patients transported north to Barcelona received adequate care before transfer. The 82 patients taken south to Valencia received minimal treatment before and during transport. Both Valencia and Barcelona had state-of-the-art burn centers. There was no significant difference in age or the extent and depth of burns between these two groups. After the first 4 days, Barcelona's survival rate was 93%, and Valencia's was 45%. Ultimately, the mortality rate did not differ.

A driver of a liquid petroleum gas tanker lost control over the vehicle and caused an over roll followed by a boiling liquid expanding vapor explosion after 15 minutes. Sixty-nine patients were admitted mainly to Dicle University Faculty of Medicine and Diyarbakir Training and Research Hospital, including 62 male and 7 female patients. The average TBSA was 51 ± 32%, including 4 patients with minor burns (<2%), 9 with moderate burns (2–10%), and 56 with severe burns (>10%). In 75%, fasciotomies had to be performed. Twenty-seven (48%) required endotracheal intubation, and 13 (23%) needed tracheostomy. A total of 76% of the patients with severe burns had to be transferred to a burn ICU. Forty-seven (68%) of the patients were distributed to 14 different locations. The overall mortality rate was 49%. The length of hospital stay was 19.4 ± 19.8 days for the survivors and 6.4 ± 4.2 days for those who died.
Aircraft collisions and crashes during an air show killed 70 and injured more than 1000 of 300,000 present ( Fig. 5.4 ). Three pilots and 67 spectators died; 346 others had serious injuries. Cooperation was hindered by medical systems that were not adapted to each other. On day 1, 12 hospitals were treating the injured; on day 2, 28; and on day 3, 74.
Outpatients numbered 213; 146 were admitted as inpatients; 84 others were transferred to ICUs. There were 112 with mechanical injuries only; 263 had isolated burn injuries; 68 had both mechanical and thermal injuries. Patients with burns of less than 20% TBSA numbered 209 (79.5% of 263). Patients with TBSA of 20–49% numbered 37; 3 of them died. Six of 9 patients with TBSA of 50–70% died. Another 8 patients, with TBSA greater than 70%, died. Of the 68 patients with combined injuries, 55 had TBSA less than 20%. Three of the 9 with TBSA of 20–40% died. No patient with combined injuries and TBSA burns greater than 40% survived.
The burn center at Ludwigshafen received 28 victims. The existing emergency plan was activated; overstaffing occurred on the first day. Initial care in the burn unit was provided in the normal way, not according to emergency plans. Experienced burn teams evaluated the patients. The disaster plan worked, but incomplete initial documentation greatly increased the next days' workload. During treatment, there were no problems with the expanded nursing staff. Qualified medics who worked double shifts for weeks were exhausted. Heavy use of burn beds caused cross-infection problems. The senior surgeon on duty on day 1 concluded that patients should have been transferred to other burn units, where free beds were available.
Kerosene caused difficulties in respiration and in function of patients' kidneys, livers, and central nervous systems. Evaluating cyclic carbohydrates in the blood soon after the incident may be important for prognosis.
Two planes collided in the air, attempting to land on the same runway. The C-130E was able to land; the F-16D, whose crew ejected, slid into a parked, fully fueled C-141 cargo plane with a crew aboard (see Fig. 5.2 ). Five hundred paratroopers, waiting 50–70 feet from the plane, were sprayed with a fireball of burning aviation fuel, with flying debris, and with the F-16's 20-mm ammunition, which began cooking off from the heat. Fifteen to 30 minutes after the incident, casualties arrived at Womack Army Medical Center (WAMC), a 155-bed hospital 5 minutes away. Fifty-one patients were treated and released; of 55 admitted, 25 went to ICUs. Six patients needing urgent surgery were sent to nearby hospitals. Seven patients were sent to the closest civilian burn center, Jaycee Burn Center at the University of North Carolina at Chapel Hill.
One U.S. Army Burn Flight Team arrived 4 hours after the accident and another after 9 hours. Escharotomies were reevaluated; some had to be repeated. Resuscitation was guided by urine output, but fluid amounts initially were not documented. Use of the Parkland formula (4 mL/kg/TBSA), rather than the modified Brooke formula (2 mL/kg/TBSA), along with untrained personnel's overestimation of TBSA, contributed to overresuscitation. Forty-one patients were transferred to the U.S. Army Institute of Surgical Research (USAISR) Burn Center for treatment, of whom 13 required mechanical ventilation. Patients assessed as having nonsurvivable injuries stayed at WAMC.
Points from Mozingo et al's review include the following:
Initially, patients with the largest burn sizes were transferred to a nearby civilian burn center. Most of them later died. This sapped resources in the burn center with little impact on outcome.
Use of different resuscitation formulas caused difficulties.
Patients with obviously lethal injuries were not transported. This did not meet expectations of the referring hospital (WAMC).
Several burn victims remained at WAMC without burn specialists because all the burn specialists were needed at the USAISR.
There was a lack of burn experience and training at WAMC. Knowledge deficits were noted in techniques (e.g., escharotomy).
Training of nonsurgical staff in Advanced Trauma Life Support (ATLS) and Advanced Burn Life Support (ABLS) was needed because the surgical staff was busy doing emergency procedures.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here