Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Other chapters in this book that deal with symptoms emphasize history as the starting point for generating possibilities for the differential diagnosis. This list of diagnostic considerations is then refined during the examination. This chapter calls for a different approach. When the neurologist evaluates a patient with a brainstem disorder, often the most effective method of diagnosis is to organize the differential diagnosis around the objective physical findings, particularly in patients with an altered mental status such as coma. The symptoms are still integrated in the approach, but the physical findings take center stage.
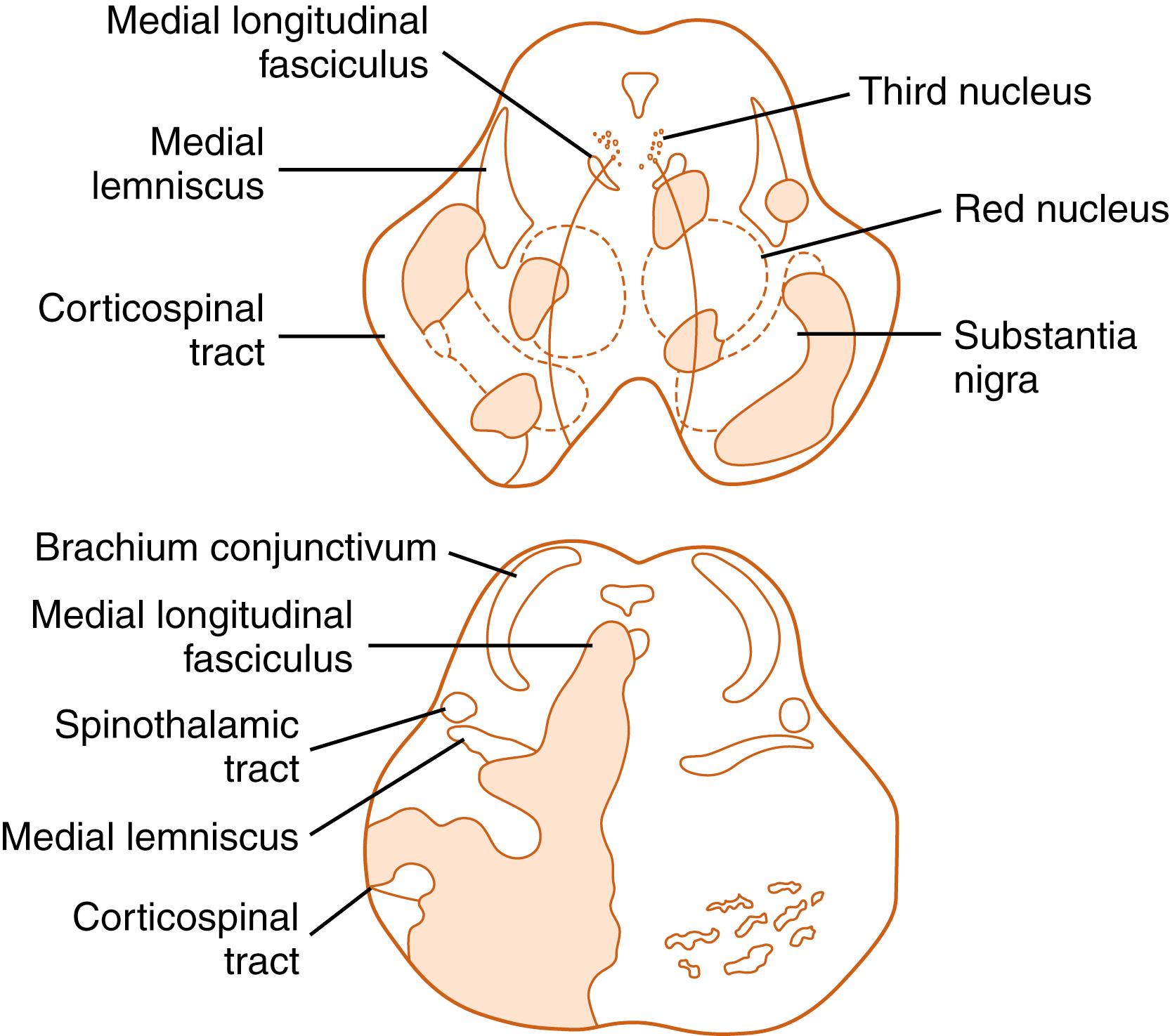
Organization around the physical findings is efficient because very specific neurological localization, which limits the diagnostic alternatives, often is possible. The long tracts of the nervous system traverse the entire brainstem in the longitudinal (rostrocaudal) plane, whereas cranial nerve nuclei and their respective cranial nerves originate and exit at distinct levels of the brainstem. This arrangement allows for exquisite localization of function based on the findings of the neurological examination.
The chapter begins with a discussion of the brainstem ocular motor syndromes, followed by descriptions of miscellaneous brainstem, brainstem stroke, and thalamic syndromes.
Combined vertical gaze ophthalmoplegia is defined as paresis of both upward and downward gaze. Vertical gaze ophthalmoplegia is an example of a brainstem syndrome in which the objective physical findings dictate the diagnostic approach to the problem. Symptoms of vertical gaze ophthalmoplegia, when present, are relatively nonspecific and usually occur in patients who have difficulty looking down, as required for reading, eating from a table, and walking down a flight of stairs. In addition, the patient’s report of symptoms may be unobtainable because of mental status changes caused by dysfunction of the reticular formation that lies adjacent to the vertical gaze generator in the rostral midbrain (see Chapter 18 ).
The neurological examination discloses associated signs of the disorders listed in the differential diagnosis ( Box 21.1 ) ( ). Coma may occur due to reticular system involvement. Long-tract signs and loss of the pupillary reflexes are commonly associated. The syndrome of combined vertical gaze ophthalmoplegia is diagnosed when the ocular findings occur in isolation from long-tract signs.
Stroke
Progressive supranuclear palsy
Cortical-basal ganglionic degeneration
Arteriovenous malformation
Multiple sclerosis
Tumor (thalamic, mesencephalic, pineal)
Hydrocephalus
Whipple disease
Syphilis
Metabolic disorders:
Lipid and lysosomal storage diseases (e.g., Niemann-Pick type C)
Wilson disease
Kernicterus
Wernicke encephalopathy
Bulbar-onset amyotrophic lateral sclerosis (associated with TDP-43–positive inclusions)
Paraneoplastic brainstem encephalitis (e.g., with Ma-2 antibodies)
Creutzfeldt-Jakob disease
With combined vertical gaze ophthalmoplegia, vertical saccades and pursuit are lost. This gaze limitation may be overcome by the oculocephalic (doll’s head or doll’s eye) maneuver, which tests the vestibuloocular reflex (VOR) (see Chapter 18 ); a conjugate eye movement in the direction opposite to that of head movement is the expected response with this maneuver. The Bell phenomenon (reflex movement of the eyes up and out in response to forced eye closure) often is absent and skew deviation (vertical misalignment of the eyes) may occur. Absence of convergence and loss of the pupillary reactions to light are common.
The location of the lesion for combined vertical gaze ophthalmoplegia is the rostral interstitial nucleus of the medial longitudinal fasciculus (riMLF) ( ). Box 21.1 lists the disorders involving the rostral mesodiencephalic region (for the differential diagnosis) that cause combined vertical gaze ophthalmoplegia (see Chapter 18 ). The most common causes of isolated combined vertical gaze ophthalmoplegia are stroke and progressive supranuclear palsy (PSP). In cortical-basal ganglionic degeneration, ocular motility findings can be similar to those in PSP but are less severe. Although the supranuclear vertical gaze ophthalmoplegia may be prominent early in the course of PSP, obvious vertical and horizontal gaze limitation usually is a late finding in cortical-basal ganglionic degeneration ( ).
The diagnostic formulation varies with the age of the patient. Isolated combined vertical gaze ophthalmoplegia usually is due to infarction of the rostral dorsal midbrain. When onset is gradual instead of abrupt or if the patient is young, other disorders should be considered (see Box 21.1 ). In the elderly, PSP (see Chapter 96 ) is likely if the onset is gradual. PSP can be mimicked by several disorders, including the treatable Whipple disease ( ). For Whipple disease, oculomasticatory myorhythmia, which consists of pendular converging and diverging eye oscillations with synchronous jaw oscillations, is pathognomonic. Laboratory investigations used to evaluate combined vertical gaze ophthalmoplegia include computed tomography (CT) or, preferably, magnetic resonance imaging (MRI). Care should be taken not to overlook lesions inferior to the floor of the third ventricle. Lumbar puncture (LP), syphilis serology, erythrocyte sedimentation rate, and antinuclear antibody assay complete the evaluation when the cause is not obvious. Small-bowel biopsy should be considered if Whipple disease is a possible diagnosis. A polymerase chain reaction (PCR) assay performed on the small-bowel biopsy, cerebrospinal fluid (CSF), or other tissues for the 16S ribosomal ribonucleic acid (RNA) gene of Tropheryma whipplei appears to have both sensitivity and specificity for the diagnosis of Whipple disease ( ).
Another brainstem syndrome that can occur without symptoms is the dorsal midbrain syndrome. When symptoms do occur, the patient reports difficulty looking up and may have blurred distant vision caused by accommodative spasm.
The tetrad of findings in the dorsal midbrain syndrome are (1) loss of upgaze, which usually is supranuclear (loss of pursuit and saccades with preservation of the VOR); (2) normal to large pupils with light-near dissociation (loss of the pupillary light reaction with preservation of the response to a near stimulus) or pupillary areflexia; (3) convergence-retraction nystagmus, in which the eyes make converging and retracting movements during attempted upward saccades; and (4) lid retraction (Collier sign).
The location of the lesion causing the upgaze paresis of the dorsal midbrain syndrome is the posterior commissure and its interstitial nucleus ( ). The presence of the full syndrome implies a lesion of the dorsal midbrain (including the posterior commissure), bilateral lesions of the pretectal region, or a large unilateral tegmental lesion. The differential diagnosis is presented in Box 21.2 . Other than the mild upgaze limitation that can occur with aging, which is caused by involutional changes in the orbital connective tissues ( ), the most common cause of isolated loss of upgaze is a tumor in the pineal region. The next most common causes are stroke and trauma. The upgaze palsy portion of the syndrome can be mimicked by any of several conditions: double elevator palsy, PSP, orbital causes such as thyroid eye disease, the bilateral Brown superior oblique tendon sheath syndrome, pseudodorsal midbrain syndrome secondary to myasthenia gravis (MG), Guillain-Barré syndrome, Miller Fisher syndrome, and congenital upgaze limitation. Forced ductions (see Chapter 18 ) may be performed by grasping anesthetized conjunctiva with forceps and moving the globe through its range of motion; the presence of restriction of movement with forced ductions implies a lesion within the orbit.
Pineal and other tumors
Stroke
Trauma (including iatrogenic from surgery)
Hydrocephalus and shunt malfunction
Multiple sclerosis
Transtentorial herniation
Congenital aqueductal stenosis
Infections:
Encephalitis
Cysticercosis
Midbrain arteriovenous malformation
Metabolic disorders:
Lipid storage disease
Wilson disease
Kernicterus
Wernicke encephalopathy
The diagnostic formulation for the dorsal midbrain syndrome varies with age. In children and adolescents, pineal region tumors or obstructive hydrocephalus are usually the cause. In young and middle-aged adults, the disorder is uncommon, and the cause may be trauma, multiple sclerosis (MS), or arteriovenous malformation (AVM). In the elderly, stroke and PSP are the most common causes.
The investigation needed to evaluate dorsal midbrain syndrome is MRI. If no structural lesion is present and an infectious or inflammatory cause is suspected, an LP should be performed.
Isolated downgaze paresis is uncommon. Symptoms, when they occur, are related to difficulty in reading, eating, and walking down stairs.
Neurological examination reveals loss of downward pursuit and saccades, although pursuit may sometimes be spared. The vertical oculocephalic maneuver may be normal or may disclose gaze limitation. Convergence may be lost, and gaze-evoked upbeat nystagmus may be present on upward gaze. In young patients, forced ductions should be performed to assess for congenital restrictive downgaze limitation.
The site of the lesion for isolated downgaze paresis is bilateral involvement of the lateral portions of the riMLF. The main considerations in the differential diagnosis are ischemic stroke, PSP, and Whipple disease. Investigations to support the clinical diagnosis include CT or MRI. Lesions may be detected in the rostral mesodiencephalic junction inferior to the floor of the third ventricle.
The diagnostic formulation for isolated downgaze limitation is uncomplicated. When acute in onset, this disorder usually is due to stroke. In an elderly patient with a progressive course, PSP should be considered.
Internuclear ophthalmoplegia (INO) is characterized by paresis or slowing of adduction of one eye, with horizontal nystagmus in the contralateral eye when it is abducted ( ![]() ). It is due to a lesion of the MLF ipsilateral to the side of the adduction weakness.
). It is due to a lesion of the MLF ipsilateral to the side of the adduction weakness.
Bilateral internuclear ophthalmoplegia in a patient with multiple sclerosis.
Surprisingly, most patients with INO do not have symptoms. The symptoms that may be associated with INO are diplopia, oscillopsia of one of the two images, and blurred vision. When diplopia is present, it can be due to medial rectus paresis (horizontal diplopia) or skew deviation (vertical diplopia).
The MLF carries information for vertical pursuit and the vertical VOR. Consequently, other associated findings with MLF lesions are abnormal vertical smooth pursuit and impaired reflex vertical eye movements (VOR, Bell phenomenon). Vertical saccadic eye movements are unaffected. Gaze-evoked vertical nystagmus (usually on upgaze) and skew deviation may be present with the higher eye on the side of the lesion. Skew deviation is a pure vertical ocular misalignment that is not due to a cranial nerve palsy, orbital lesion, or strabismus but is caused by unilateral or asymmetrical damage to the otolith-ocular pathways ( ).
INO, discussed further in Chapter 18 , may be a false localizing sign. Brainstem compression due to subdural hematoma with transtentorial herniation and cerebellar masses may cause INO. MG, Guillain-Barré syndrome, and Miller Fisher syndrome also may simulate INO.
The diagnostic considerations are many and varied. Examination can differentiate a lesion of the MLF from a partial third cranial nerve palsy, MG, strabismus, or thyroid eye disease. For example, intact convergence eye movements would be expected in an isolated MLF lesion but not in conditions affecting the third cranial nerve, medial rectus muscles, or neuromuscular junction. The common causes of INO are stroke (including vertebral artery dissection) in older age groups and MS in the young. One series reported that approximately one-third of INO cases are caused by stroke, one-third by MS, and one-third by other causes ( ). Less common causes include trauma, herniation, infections, tumor, vasculitis, and surgical procedures.
Investigations that are performed to elucidate the cause include MRI. Thin cuts are often needed to find the lesion when INO is isolated. Investigations should be performed to evaluate for MG unless there are associated signs of obligatory brainstem dysfunction.
The diagnostic formulation for INO first necessitates accurate localization of the lesion. Limitation or slowing of adduction initially is formulated simply as an adduction deficit. It may also be due to (1) a lesion of the midbrain or third cranial nerve disrupting innervation; (2) a disorder of the neuromuscular junction (MG); or (3) a lesion involving the medial rectus muscle.
Although there are no common symptoms of horizontal gaze paresis, this condition seldom occurs in isolation. Patients may complain of inability to see or to look to the side. Because supranuclear gaze pareses are conjugate by definition, diplopia does not occur.
On examination, with unilateral isolated involvement of the paramedian pontine reticular formation (PPRF), loss of ipsilateral saccades and pursuit is evident. However, full horizontal eye movements can be demonstrated with the oculocephalic maneuver (VOR).
Lesions of the sixth cranial nerve nucleus cause horizontal gaze paresis with inability of the oculocephalic maneuver (VOR) to overcome the limitation. Although an associated ipsilateral peripheral facial palsy is usually seen due to involvement of the fascicle of the seventh cranial nerve coursing over the sixth cranial nerve nucleus, cases of isolated horizontal gaze paresis caused by sixth nerve nuclear lesions have been reported ( ). With bilateral lesions, loss or limitation of horizontal saccades and (usually) pursuit in both directions is characteristic. Gaze-paretic nystagmus may be present. In the acute phase, transient vertical gaze paresis and vertical nystagmus or upgaze paresis can also be seen. In the chronic phase, vertical eye movements are full, although nystagmus may be noted on upgaze.
The location of the lesion for horizontal gaze paresis is the frontopontine tract, mesencephalic reticular formation, PPRF, and sixth cranial nerve nucleus. The explanation for gaze palsy occurring with a nuclear lesion is given later in the chapter (see Syndromes Involving Ocular Motor Nuclei).
The diagnostic possibilities are varied. As with other ocular motility disorders, MG may cause gaze limitation that simulates a central nervous system (CNS) lesion. The diagnostic formulation varies with age, rapidity of onset, and associated clinical findings. For patients with an acute onset who are older than 50 years of age, stroke is a likely cause. With a subacute onset before the age of 50 years, a diagnosis of MS should be considered. Congenital cases usually are due to Möbius syndrome ( ). Systemic lupus erythematosus (SLE), syphilis, and Wernicke encephalopathy should be considered for any acquired cases.
Investigations for horizontal gaze paresis should include MRI. If there are no obligatory signs of CNS dysfunction, MG must be considered.
The characteristic symptom of global paralysis of gaze is an inability to look voluntarily in any direction. However, global paralysis of gaze rarely occurs in isolation, and signs and symptoms of involvement of other local structures usually are present.
The location of the lesion is the frontopontine tract for saccades, and the parietooccipitopontine tract for pursuit, where they converge at the subthalamic and upper midbrain level ( ). The differential diagnosis for total ophthalmoplegia is given in Box 21.3 . The common causes for this presentation are diseases that do not involve the CNS, such as Miller Fisher syndrome, Guillain-Barré syndrome, MG, and chronic progressive external ophthalmoplegia (CPEO); for intraaxial lesions, considerations include stroke, Wernicke encephalopathy, PSP, and other neurodegenerative disorders (e.g., spinocerebellar ataxias).
Acute:
Miller Fisher syndrome
Guillain-Barré syndrome
Bilateral pontine or midbrain-thalamic stroke
Myasthenia gravis
Pituitary apoplexy
Botulism
Anticonvulsant intoxication
Multiple cranial neuropathies from infection or neoplasm
Wernicke encephalopathy
Chronic/Progressive:
Chronic progressive external ophthalmoplegia syndromes
Oculopharyngeal muscular dystrophy
Myotonic dystrophy and other congenital myopathies
Congenital cranial dysinnervation syndromes
Neurodegenerative diseases (e.g., progressive supranuclear palsy, late spinocerebellar ataxia type 2)
Myasthenia gravis
Thyroid eye disease (especially in combination with myasthenia gravis)
The diagnostic formulation usually is focused on extraaxial (cranial nerve, neuromuscular junction, or muscle) pathology, because a brainstem lesion rarely causes isolated complete ophthalmoplegia. Miller Fisher syndrome, Guillain-Barré syndrome, bilateral cavernous sinus lesions (e.g., metastases, pituitary apoplexy), meningitis, and MG (sometimes in combination with thyroid eye disease) are likely possibilities if the onset is subacute ( ). If the presentation is long-standing, slowly progressive, and accompanied by ptosis, CPEO syndromes, such as Kearns-Sayre, and other myopathic processes, such as oculopharyngeal muscular dystrophy (particularly in patients of French-Canadian descent), should be considered. In these extraaxial disorders, the gaze limitation cannot be overcome with the oculocephalic maneuver (VOR). PSP is a diagnostic possibility in the elderly, whereas Wernicke encephalopathy should be considered in alcoholics and nutritionally deprived patients. Whipple disease also can cause this rare clinical presentation.
Investigations for patients with global paralysis of gaze should include MRI. Investigations for MG should be considered. When botulism is suspected, electromyography with repetitive nerve stimulation and serum or stool assay for botulinum toxin should be performed.
The one-and-a-half syndrome is characterized by an ipsilesional horizontal gaze palsy, together with an ipsilesional INO (impaired adduction of the ipsilesional eye). The common symptoms are diplopia, oscillopsia (the illusion that objects or scenes are oscillating), and blurred vision. Associated findings include skew deviation and gaze-evoked nystagmus on upgaze or lateral gaze. Acutely, there may be an exotropia (one eye deviated outward) in primary position. Other features may include limitation of upgaze, impaired vertical pursuit, and loss of convergence.
The location of the lesion is the PPRF or sixth cranial nerve nucleus, with extension to involve the internuclear fibers crossing from the contralateral sixth cranial nerve nucleus, which causes the INO. Entities to consider in the differential diagnosis include MS, stroke, AVM, and tumor of the lower pons. A pseudo-one-and-a-half syndrome may occur with MG, Miller Fisher syndrome, or Guillain-Barré syndrome. The diagnostic formulation for the one-and-a-half syndrome is similar to that for INO. Before the age of 50 years, the cause usually is MS; after age 50 years, it usually is stroke.
Variations of the one-and-a-half syndrome have been described, including the eight-and-a-half syndrome, which consists of a one-and-a-half syndrome with an ipsilateral facial palsy, and eight syndrome, which consists of a lateral gaze palsy (without INO) and a facial palsy ( ).
Appropriate investigations for the one-and-a-half syndrome and its variants are MRI and, if indicated, LP.
Patients with lesions involving the third or sixth cranial nerve nucleus present not only with accompanying long-tract signs but also show different ocular motility disturbances than seen with lesions involving the third or sixth fascicle or cranial nerve.
The common manifestations of third cranial nerve nucleus lesions are diplopia and ptosis. The signs present on the side of the lesion are weakness of the inferior and medial recti and the inferior oblique muscles. Upgaze limitation is present in both eyes because the superior rectus subnucleus is contralateral, and the axons from this subnucleus cross within the nuclear complex. In addition, ptosis and dilated unreactive pupils may be present on both sides because the levator subnucleus (also known as the central caudal nucleus) and Edinger-Westphal nuclei are bilaterally represented.
The main considerations in the differential diagnosis are stroke (either ischemic or hemorrhagic), metastatic tumor, and MS. Of these diagnoses, only ischemic stroke is common. Disorders that simulate nuclear third cranial nerve palsy include MG, CPEO, thyroid eye disease, Miller Fisher syndrome, and Guillain-Barré syndrome.
The pertinent investigation for this syndrome is MRI, which usually demonstrates an ischemic stroke. Once the proper localization has been made, the diagnostic formulation is straightforward.
The sixth cranial nerve nucleus has two populations of neurons. The abducens motor neurons innervate the ipsilateral lateral rectus muscle. Internuclear neurons decussate at the level of the sixth cranial nerve nucleus, travel up the MLF, and terminate on the medial rectus subnucleus of the contralateral third cranial nerve. Accordingly, a lesion of the sixth cranial nerve nucleus causes ipsilateral horizontal gaze palsy.
Patients with an isolated horizontal gaze palsy are often asymptomatic. If they do have symptoms, they report difficulty looking to one side. On examination, a conjugate horizontal gaze paresis is present, which cannot be overcome by the oculocephalic maneuver or caloric stimulation. A peripheral seventh cranial nerve palsy usually accompanies a lesion of the sixth cranial nerve nucleus. Considerations in the differential diagnosis include stroke ( ), Wernicke encephalopathy, MS, and a tumor of the pontomedullary junction.
Evaluation of a lesion of the sixth cranial nerve nucleus includes MRI, possibly LP, and investigations (e.g., edrophonium or prostigmine test) for MG if there are no long-tract signs to indicate intraaxial disease.
Common symptoms of the diencephalic syndrome include emaciation with increased appetite, euphoria, vomiting, and excessive sweating ( ). Patients also may have an alert appearance with motor hyperactivity. Most cases occur in children younger than 3 years.
The differential diagnosis should include hyperthyroidism, diabetes mellitus, a tumor in the region of the fourth ventricle, vein of Galen malformation, and a hypothalamic tumor. Most patients appear pale despite lack of anemia. Ophthalmological findings include optic atrophy and, less commonly, nystagmus.
Investigations for diencephalic syndrome may show an elevated serum growth hormone level that is incompletely suppressed by hyperglycemia. MRI often demonstrates a hypothalamic mass lesion. Malignant cells may be present in the CSF and are diagnostic. The CSF also may contain human chorionic gonadotropin in patients with germinomas. An LP should not be performed if neuroimaging studies demonstrate a mass effect.
The common symptoms of thalamic syndrome include pain (thalamic pain), numbness, and hemisensory loss. The pain may be spontaneous or evoked by any form of stimulation. It often has a disagreeable and lasting quality. Patients also may complain of a distorted sense of taste. Right thalamic lesions appear to predominate.
On examination, a marked hemianesthesia is present which may be dissociated: that is, pain and temperature or light touch and vibration sense may be separately lost. Proprioceptive loss, often with astereognosis, is a common feature. A transitory hemiparesis sometimes occurs.
The usual location of the lesion for this type of pain is the ventroposterolateral nucleus of the thalamus. In addition to the thalamus, thalamic-type pain can occur with lesions of the parietal lobe, medial lemniscus, and dorsolateral medulla ( ). The differential diagnosis includes stroke and tumor. The diagnostic formulation depends on the rate of onset of symptoms, associated signs, and findings on neuroimaging studies. The apoplectic onset of symptoms implicates stroke. Gradual onset is characteristic of tumor. Neuroimaging studies, preferably MRI, should confirm the clinical impression.
The symptoms associated with tectal deafness are bilateral deafness associated with other related CNS symptoms such as poor coordination, weakness, or vertigo. The main considerations in the differential diagnosis for the deafness are conductive hearing loss, cochlear disorders, bilateral eighth cranial nerve lesions, tectal deafness, and pure word deafness.
On examination, deafness that usually spares pure tones is confirmed. Pure word deafness with lesions of the inferior colliculi has been reported ( ). Other brainstem signs, including the dorsal midbrain syndrome, often are associated. The location of the lesion is the inferior colliculi; the most common causes are trauma, stroke, or a tumor of the brainstem, cerebellum, or pineal region. The diagnostic formulation for hearing loss caused by lesions rostral to the cochlear nuclei is the presence of hearing loss characterized by sparing of pure tone, with marked deterioration when background noise distortion or other aural stimuli are added. Signs of damage to adjacent nervous system structures are often present.
The pertinent investigations include MRI and an audiogram. Tests that reveal CNS auditory loss are distorted speech audiometry, dichotic auditory testing, and auditory brainstem evoked responses, although findings on evoked responses may be normal ( ).
Foramen magnum syndrome is characterized by upper motor neuron–type weakness and sensory loss in any modality below the head. Detecting this syndrome is important because it often is caused by benign tumors such as meningiomas or fibromas, which may be removed completely when detected early in their course. Its only manifestations may be identical to those of a high spinal cord syndrome (see Chapter 27 ).
The common initial symptoms include neck stiffness and pain, which may radiate into the shoulder. Occipital headache also may be an early symptom. Other common symptoms are weakness of the upper or lower extremities, numbness (most commonly of hands or arms), clumsiness, and gait disturbance.
Considerations in the differential diagnosis include cervical spondylosis, syringomyelia, MS, transverse myelitis, atlantoaxial subluxation (e.g., in rheumatoid arthritis), Chiari malformation, and foramen magnum or upper cervical cord tumor.
On examination, hemiparesis or quadriparesis and sensory loss are common. The loss of sensation may involve all modalities. It may be dissociated and capelike or may occur in a C2 distribution. Some patients have hemisensory loss below the cranium or involvement of only the lower extremities.
Pseudoathetosis resulting from loss of joint position sense may be an early sign. Atrophy of muscles of the upper extremities may occur at levels well below that of the lesion. Electric shock–like sensations radiating down the spine, which may be transmitted into the extremities, may occur with neck flexion (Lhermitte sign). This phenomenon may occur with lesions of the posterior columns, most commonly from MS. Lower cranial nerve palsies are less common. The presence of downbeat nystagmus in primary position or lateral gaze strongly suggests a lesion involving the craniocervical junction; this may be missed unless the nystagmus is sought when the patient gazes laterally and downward.
The differential diagnosis includes a foramen magnum or upper cervical cord tumor. The tumor is often a meningioma, neurofibroma, glioma, or metastasis. Cervical spondylosis, MS, syringobulbia, and the Chiari malformation (often accompanied by a syrinx) are other diagnostic considerations. The definitive investigation for evaluation of this syndrome is MRI.
Patients with foramen magnum tumors may have a relapsing-remitting clinical course with features that simulate those of MS. Because many of the tumors are meningiomas, the clinician should be alert for patients at risk. Meningiomas occur with increased frequency in women in their childbearing years and increase in size during pregnancy. Cervical spondylosis usually is associated with a related radiculopathy and is not accompanied by downbeat nystagmus or lower cranial nerve abnormalities. Diagnosis requires a high index of suspicion; foramen magnum tumors are often difficult to diagnose early because signs may be minimal despite a large tumor.
Syringobulbia is a disorder of the lower brainstem caused by progressive enlargement of a fluid-filled cavity that involves the medulla and almost invariably the spinal cord (syringomyelia). The symptoms and signs are caused by dysfunction of the central spinal cord.
The common symptoms of syringobulbia and syringomyelia are lack of pain with accidental burns, hand numbness, neck and arm pain, leg stiffness, and headache, together with oscillopsia, diplopia, or vertigo. On examination, signs of lower brainstem dysfunction are evident. Lower motor neuron signs of the ninth through twelfth cranial nerves may be present. Nystagmus, if present, can be horizontal, vertical, or torsional. Signs of a spinal cord lesion characteristically coexist. In the upper extremities, dissociated anesthesia of an upper limb or forequarter (i.e., loss of pain and temperature sensation with sparing of other modalities) may be noted. The sensory loss also may be in a hemisensory distribution and deep tendon reflexes in the upper extremities are often absent or decreased.
Spastic paraparesis, usually asymmetrical, may occur. Loss of facial sensation can occur in an onion-skin pattern emanating from the corner of the mouth. Charcot (neuropathic) joints and trophic skin disorders may be present in long-standing cases. Horner syndrome and sphincter disturbances are other occasional findings.
The lesion is located in a rostrocaudal longitudinal cavity from the medulla into the spinal cord. The cavity usually is located near the fourth ventricle or central canal of the spinal cord. The most reliable and sensitive investigation for syringobulbia is MRI.
The main considerations in the differential diagnosis are an intrinsic central cord and lower brainstem lesion (syrinx, tumor, or trauma) and compressive foramen magnum syndrome caused by a tumor or a Chiari type I malformation. Less likely causes are MS and spinal arachnoiditis.
The diagnostic formulation for syringobulbia is based on data from the history, examination, and investigations. It most often is a disease of young adults, with a peak incidence in the third and fourth decades of life. Painless burns and dissociated segmental anesthesia of the upper extremities are highly suggestive of the diagnosis. A diagnosis of MS requires the presence of other noncontiguous lesions, oligoclonal bands in the CSF, and characteristic MRI findings. Tumors usually produce a more rapid course.
Vertebrobasilar ischemic lesions often have a rostrocaudal or patchy distribution ( Fig. 21.1 ), rather than a simplified transverse distribution ( ). Thus a single lesion may not explain all of the clinical features.
The cardinal manifestations of brainstem stroke are involvement of the long tracts of the brainstem in combination with cranial nerve deficits. Crossed cranial nerve and motor or sensory long-tract deficits are characteristic. The cranial nerve palsy is ipsilateral to the lesion, whereas the long-tract signs are contralateral—hence the term crossed . Coma, ataxia, and vertigo, which are common with vertebrobasilar (posterior circulation) stroke, are uncommon with carotid (anterior circulation) stroke. INO, unreactive pupils, lower motor neuron cranial nerve impairment, and skew deviation, when caused by stroke, occur only with posterior circulation lesions. The same is usually true for nystagmus and most other ocular oscillations.
Another characteristic of vertebrobasilar ischemia is bilateral involvement of the long tracts. This can result in locked-in syndrome, which is usually caused by a lesion of the basis pontis and characterized by quadriplegia, corticobulbar tract involvement, and loss of the ability to produce speech. The reticular activating system is spared, so consciousness is preserved. Eye movements and blinking may be all that is left under voluntary control.
Another feature of bilateral lesions of the long tracts is pseudobulbar palsy. The symptoms resemble those that occur with medullary lesions. However, the cranial nerve nuclei have lost their cortical input, which results in dysarthria, dysphagia, bilateral facial weakness, extremity weakness, and emotional lability. A more appropriate term for this syndrome is supranuclear bulbar palsy .
Cortical blindness occurs with bilateral posterior cerebral artery occlusion and concomitant occipital lobe infarction.
Ischemic stroke syndromes are outlined next. These syndromes can occur in isolation, as presented here, or in combination. The combinations can be medial with lateral involvement or often rostrocaudal extension. Several classic stroke syndromes, such as the Wallenberg lateral medullary syndrome and Weber cerebral peduncle syndrome, exist. However, an investigation that looked prospectively at 304 cases of brainstem stroke found one of 24 eponymous syndromes in only 20 cases; approximately 20% of cases showed different unnamed crossed brainstem syndromes ( ).
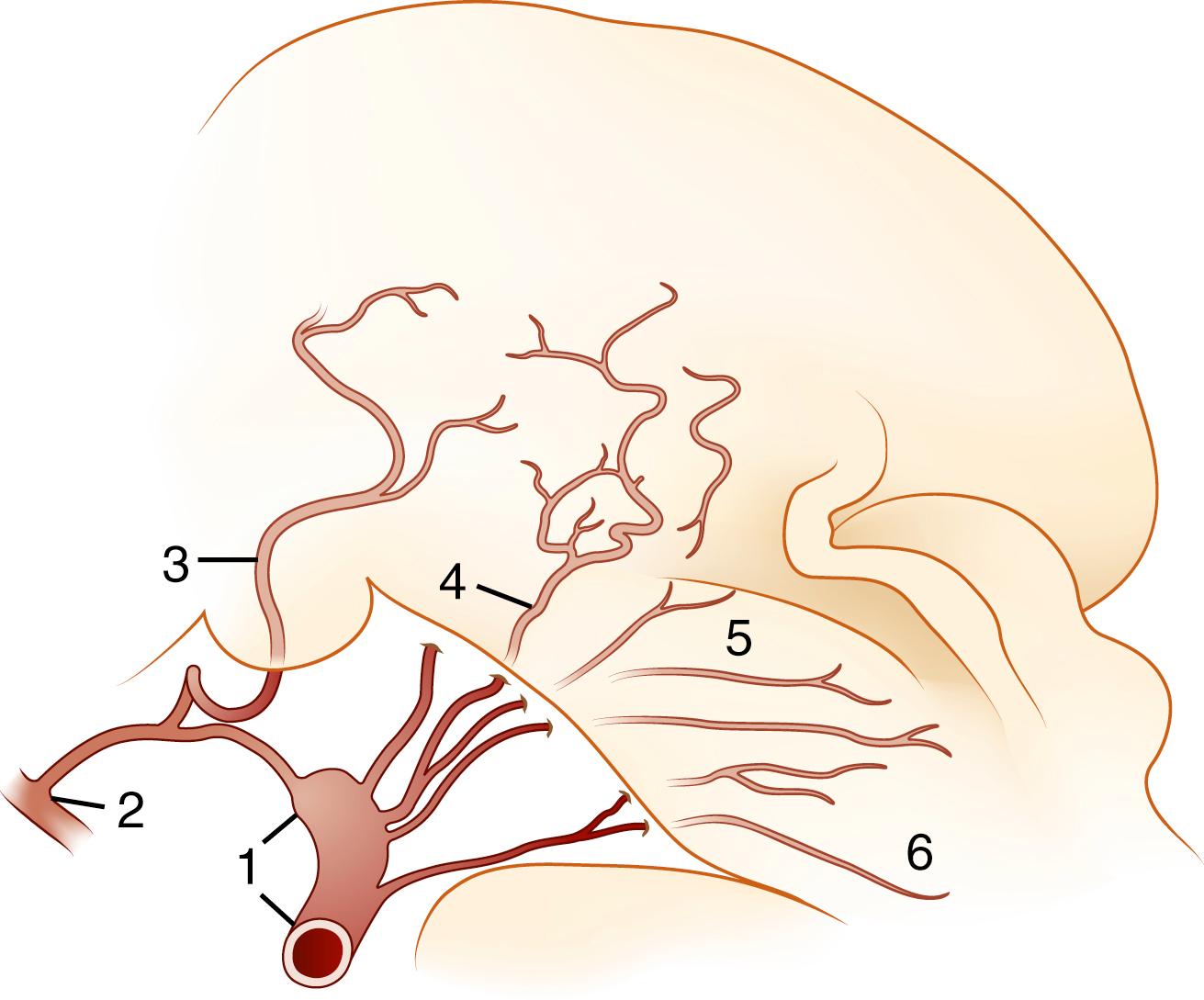
The blood supply of the thalamus arises from the posterior cerebral, posterior communicating, basilar communicating (P1 segment of the posterior communicating artery) ( Fig. 21.2 ), and anterior and posterior choroidal arteries. Thalamic stroke syndromes are listed in Box 21.4 . Fig. 21.3 illustrates the arterial territories of the thalamus.
Contralateral weakness, vision loss
Confusion
Disorientation
Language disturbance
Contralateral:
Hemiparesis
Hemiataxia
Hemisensory loss
Homonymous hemianopia
Right-sided lesion: visuospatial abnormalities, hemineglect, nonverbal intellect affected
Left-sided lesion: disorientation, aphasia
Thalamic polar (tuberothalamic) artery (see Figs. 21.2 and 21.3 )
Disorientation and confusion
Coma with occlusion of mainstem variant
Visual blurring
Vertical gaze ophthalmoplegia
Loss of pupillary reflexes
Loss of convergence
Disorientation and confusion, stupor, coma, and various neuropsychiatric disturbances
Posterior thalamosubthalamic paramedian artery (thalamic paramedian or deep interpeduncular profundus artery; see Figs. 21.2 and 21.3 )
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here