Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter includes an accompanying lecture presentation that has been prepared by the authors: ![]() .
.
The development of early brain retractors accompanied the advent of intradural neurosurgical procedures in the 18th century.
Brain retractors have evolved from simple handheld retractors, to self-retaining retractors, to soft tissue– and skull-mounted retractors, and finally to modern table-mounted and headrest-mounted retractors.
Retractor use is secondary to prioritization of proper patient positioning, maximal bony exposure, and appropriate arachnoid dissection, and can be assisted with techniques such as CSF diversion and stereotactic navigation.
Parenchymal injury secondary to brain retraction is common. Intermittent cessation of retractor pressure can decrease tissue damage.
Modern parenchymal tubular retractors and endoscopic approaches can help to minimize brain retraction and parenchymal injury. With appropriate positioning and dissection, many intracranial lesions can be accessed without retractors.
“Good illumination, unobstructed vision and a view of the whole operative field are of essential value to the surgeon. The better these conditions are, the greater precision with which he can identify the structures of pathophysiological significance.” M. G. Yaşargil, 1958
Retraction is as much art as it is science. Throughout the ages, surgeons have struggled with the concept of retraction. Used by every surgeon at some point in his or her career but truly understood by only some, retraction has just recently become a subject for scientific inquiry.
The goal of brain retraction is to allow the surgeon to safely visualize an area of interest. Early retraction was dependent on the surgeon’s finger, forceps, and/or suction device. Advances in methods of brain retraction reflect the evolution of technology and have been driven by increasingly complex surgical exposures. Irrespective of the sophistication of the retraction method, avoidance of retractor-related brain injury remains a paramount goal and has recently led to an aggressive effort to minimize or eliminate the need for some forms of retraction.
This chapter initially reviews the history of brain retractor methods (online); then outlines the principles of retractor-based surgery and the avoidance of retractor injury; and closes with future developments in retractor technology.
The roots of neurological surgery predate written language, and thus the study of the evolution of the field from antiquity is often difficult. However, the importance of tracing the historical developments of neurosurgery cannot be underestimated, because it provides us with a glimpse into the motivations and ingenuity that have driven the field forward to the modern achievements of our surgical practice today. In particular, today’s surgeons can benefit tremendously from tracing the history of brain retractors throughout neurosurgery. The innovation of brain retraction allowed for the development of more advanced surgical procedures that have driven the field forward in a self-perpetuating manner.
Prehistoric man gave much respect to the dura and brain parenchyma, with focus on cranial surgery that required retraction of extra-axial soft tissues only. This inviolate respect for the dura carried through not only prehistory but also Greco-Roman times.
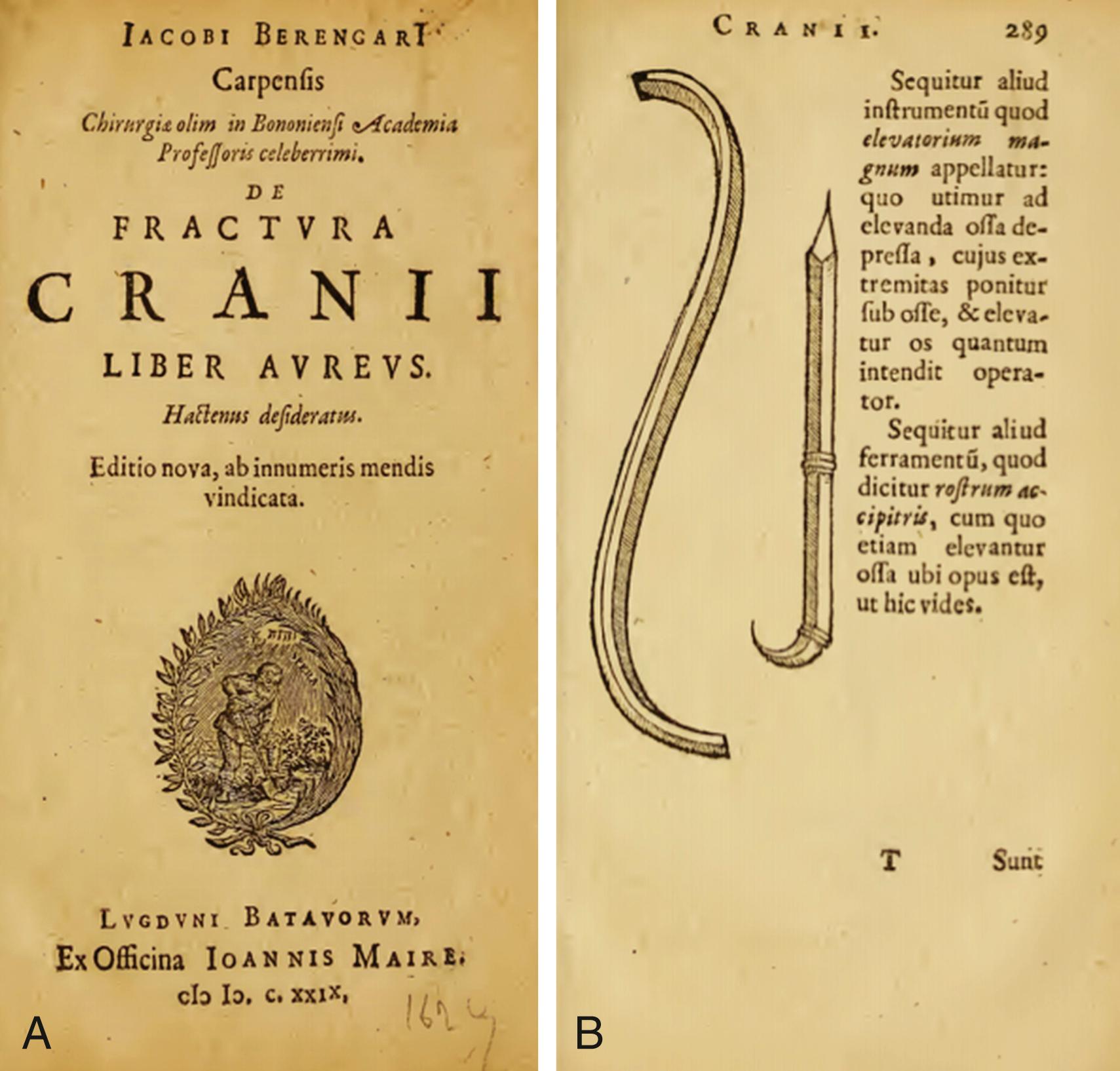
The demise of the Roman Empire shifted the focus of education and learning for centuries. With the prohibition of cadaveric dissections, understanding of cranial anatomy was slow to progress. Trepanation and the practice of Hippocratic ideas remained the mainstay for treatment of neurosurgical ailments through the Middle Ages, with a large focus on head trauma. The only retraction required was that of the extra-axial soft tissue, and surgical instrumentation reflected the crude trepanation procedures using chisels and hammers. Anesthesia and antisepsis were not practiced, and most surgical instrumentation was crafted by blacksmiths who also created the farming equipment of the time. Jacopo Berengario da Carpi ( ce 1460–1530) described an elevator (retractor) used in 16th century trepanation in his book on skull fractures , ( eFig. 33.1 ). The instruments of his time, although decorative, were rather large and clumsy.
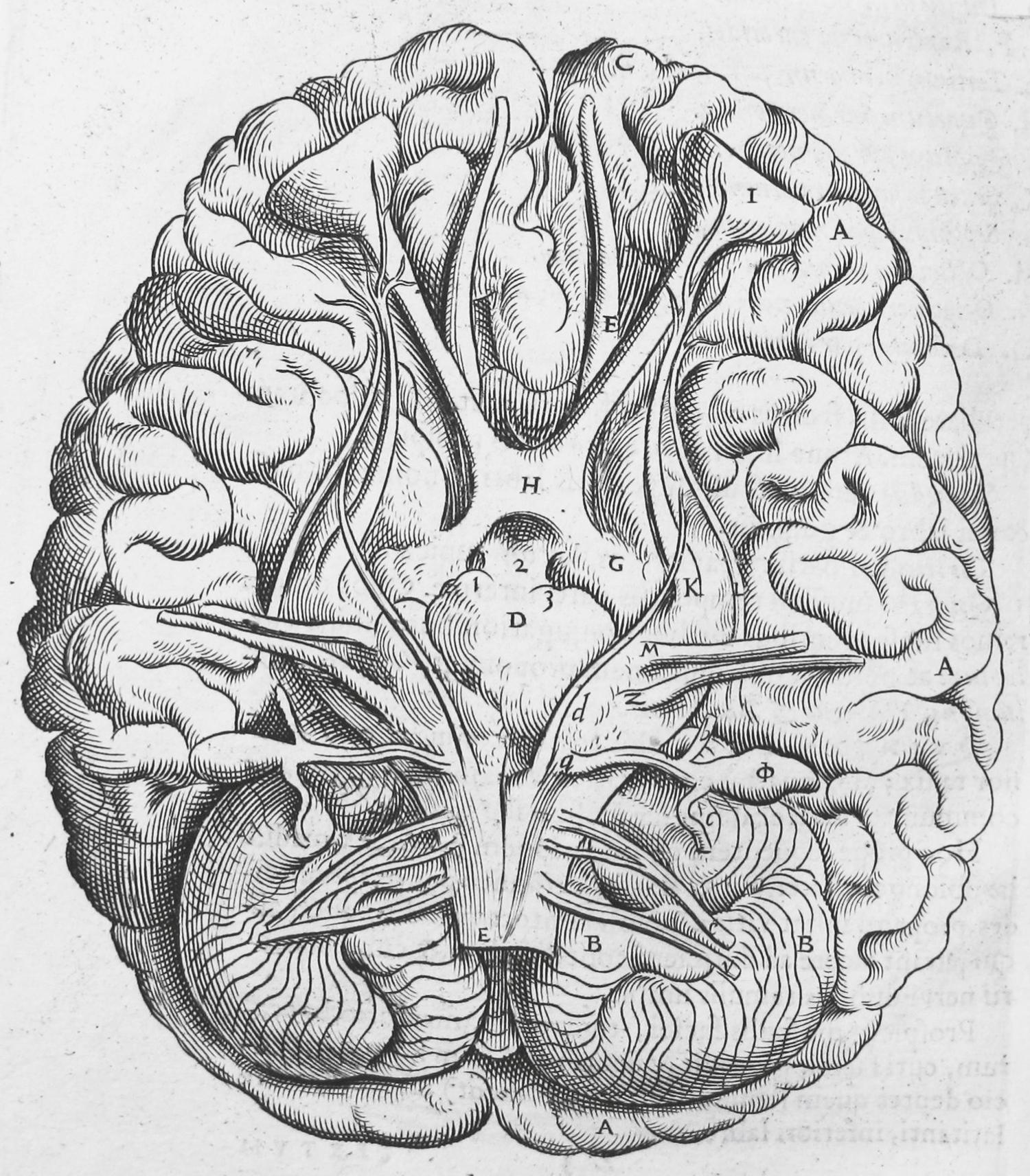
The Renaissance and renewed practice of cadaveric dissections by Leonardo da Vinci (1452–1519) and Andreas Vesalius (1514–1564) led to knowledge of the contents of the cranial vault and detailed anatomic illustrations of the cranial nerves , ( eFig. 33.2 ). However, it was not truly until the 19th century that medicine had advanced enough to allow more intricate cranial openings, which led to exploration beyond the dura. Aided by antisepsis, anesthesia, hemostasis, and, most important, new surgical instrumentation, the stage was set for the beginnings of modern neurosurgery by the 19th century.
The 19th century neurosurgeon could now become more aggressive in the management of intracranial pathology. As such operations became more feasible, neurosurgeons quickly realized the necessity for brain retraction to allow operating deeper into the brain. However, the neurosurgeons of this period used heavy general surgical instruments that were poorly suited for the delicate nature of the brain parenchyma. Consequently, neurosurgeons of the time used a variety of techniques to assist in greater visualization of the brain. Hans Brun (1874–1947) suggested delicate saline injection around intraparenchymal lesions to help retract tumors from normal brain tissue. Sir Charles Ballance (1856–1936), one of the pioneering British neurosurgeons, described marine sponges that would expand and shift the brain tissue for greater visualization. In division of the auditory nerve for tinnitus, Ballance reported a case that involved a technique he did not think had been used anywhere previously:
“The dura was opened and the cerebellar hemisphere displaced backwards and inwards by marine sponge pressure. On removing the sponges the cerebellum remained in the retracted position so that the fifth, seventh, eighth, ninth, tenth, eleventh, and twelfth nerves were exposed to view.”
The first brain retractors were handheld by an assistant, but this often resulted in the assistant’s hand obscuring light and vision as well as occasional retractor slippage. This often led to excessive retraction on the parenchyma and injury. The handheld retractors of this period were generally either flat spatulas made of copper or silver or spoon-shaped. Perhaps the most influential neurosurgical writing of the late 19th century was that of Ernst von Bergmann (1836–1907), who in 1889 published a critical overview of the field. He discussed numerous problems that prevented successful intracranial surgery, highlighting how much more needed to be learned and the need for new techniques and instrumentation.
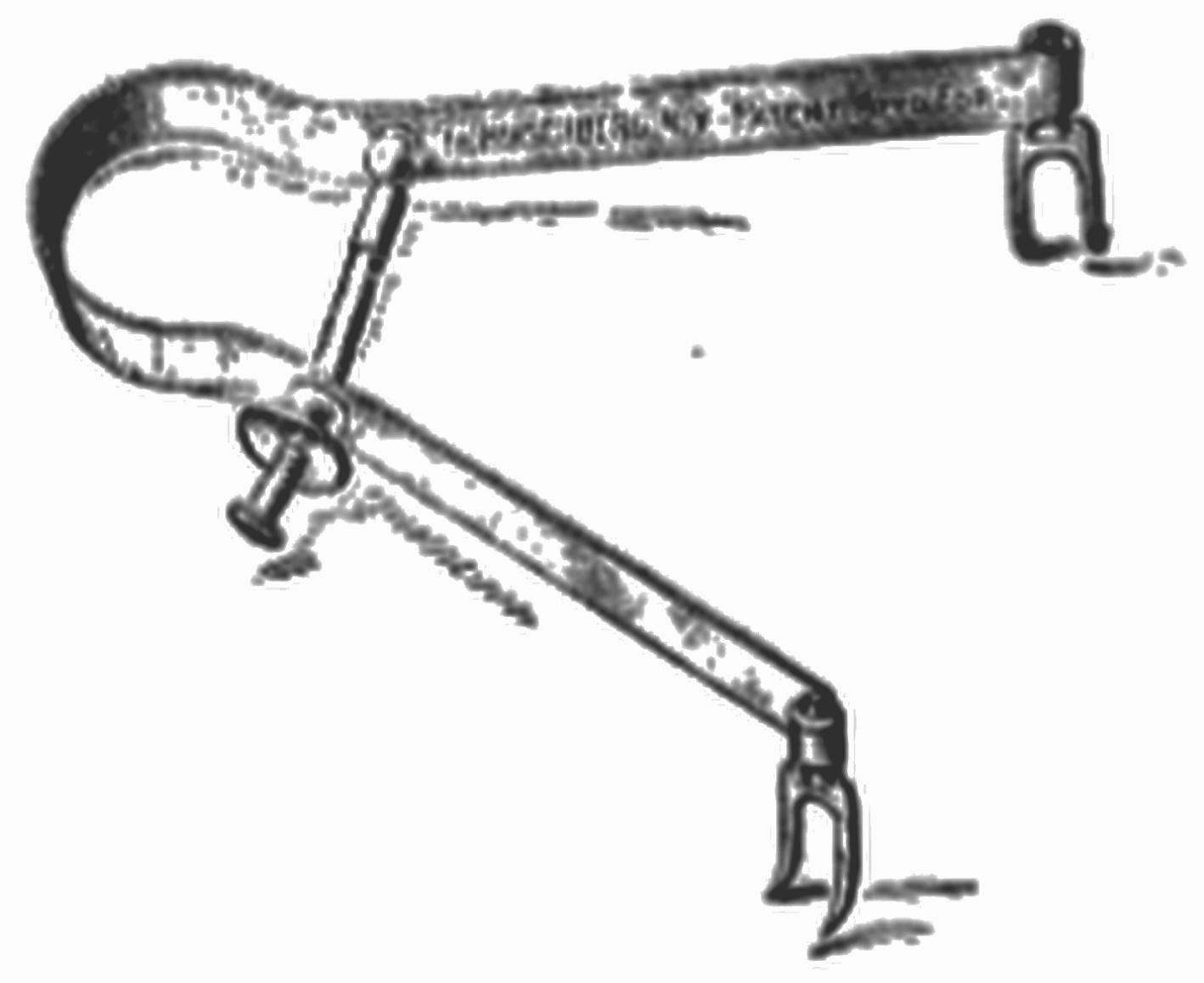
The early 20th century saw the evolution of the simple handheld retractor to a multipurpose tool. Neurosurgeons in France began using brain retraction, and in 1913 Thierry de Martel (1875–1940) developed a malleable retractor that he attached to the edge of the cranial defect. This was the first development of the mounted retractor, to be discussed later. de Martel’s German contemporary, Fedor Krause (1857–1937), began using a suction-retraction technique to help visualize and dissect gliomas. His method involved vacuum suction of the tumor to make the dissections less traumatic, and was found to be especially useful in the posterior fossa ( eFig. 33.3 ). Charles Frazier (1870–1936) developed a spoon-shaped handheld brain elevator, specifically designed for use at the base of the brain. This device was designed such that it would be angled in a manner that when held did not obscure the surgeon’s line of sight ( eFig. 33.4 ).
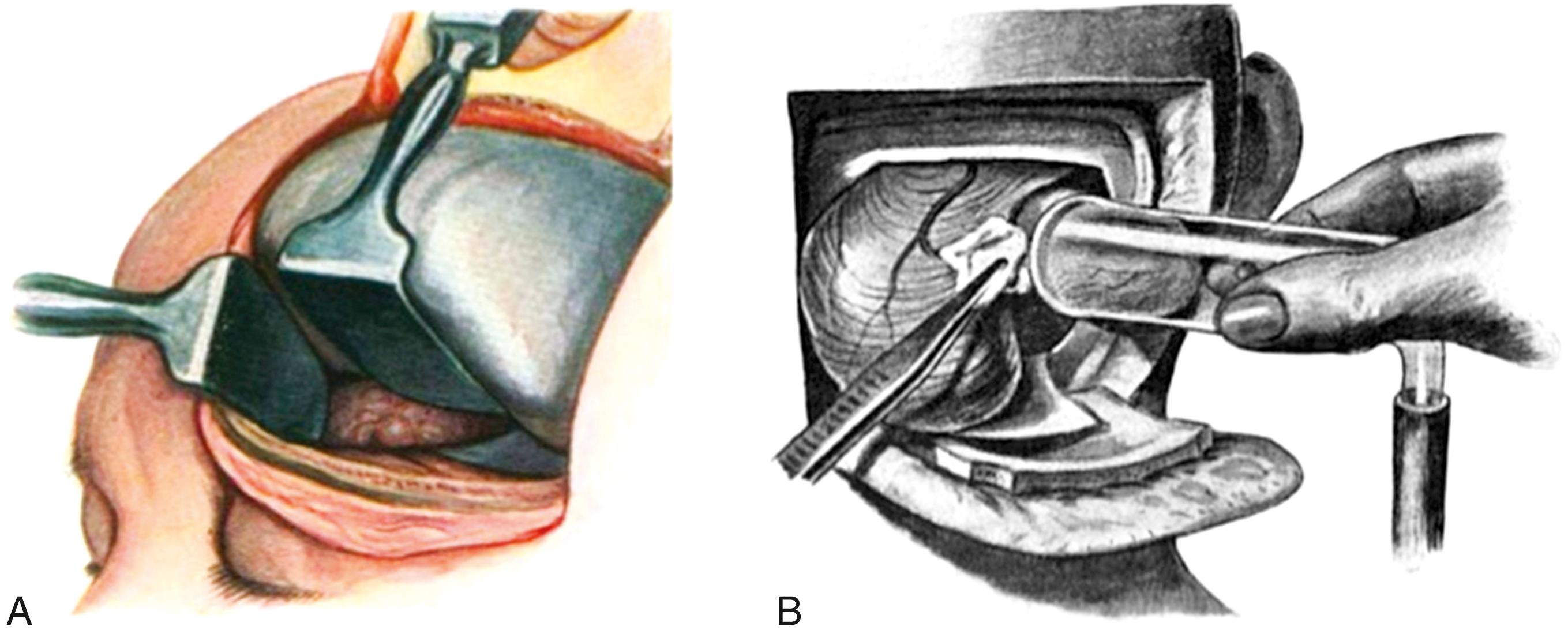
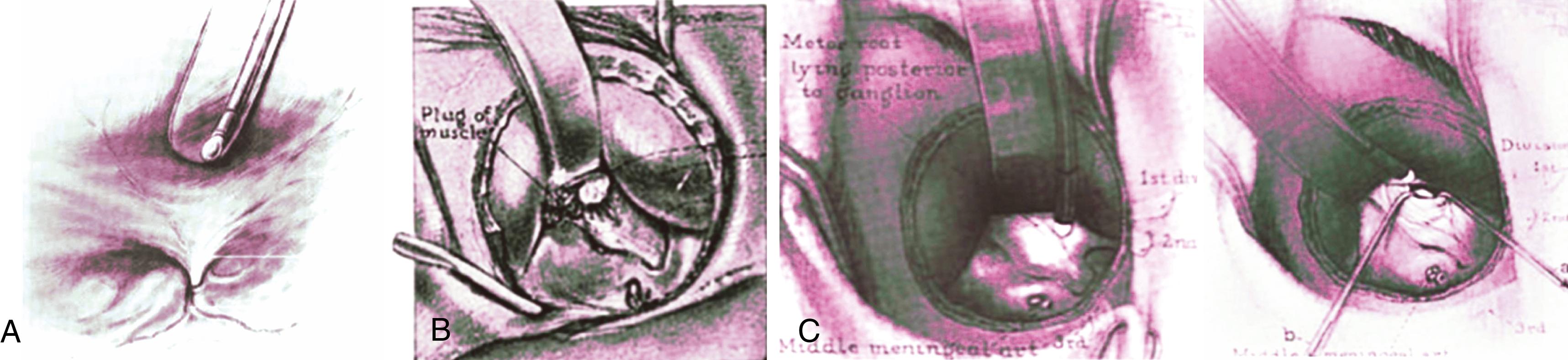
The next major development in brain retraction was the addition of light sources to illuminate the surgical area deep within the operative field. Although Temple Fay (1895–1963) is often given credit for use of the first lighted retractor in 1927, there is compelling evidence that his mentor, Dr. Frazier, was using such an instrument years before. In a 1921 edition of Annals of Surgery, Frazier vividly illustrated a novel approach to the sphenopalatine ganglion with a lighted retractor:
“… I have found my illuminated retractor—so satisfactory in the Gasserian ganglion operation—amply illuminates the field” ( eFig. 33.5A ).
Predating both Fay and Frazier, Alfred Washington Adson (1887–1951) was using a lighted retractor for temporal lobe elevation to access the trigeminal ganglion as early as 1920 ( eFig. 33.5B–C ).

Spatulas and spoon-shaped retractors served their purpose for elevating and dissecting different areas of brain tissue during surgery, but other retraction methods were necessary to assist in opening and visualizing the operative field as surgical approaches became increasingly complex. Self-retaining retraction allowed for much greater surgical freedom for the primary surgeon and his assistant.
In terms of self-retaining retractors specific to cranial neurosurgery, there are four main groups: soft tissue mounted (secured by tension in the soft tissue and muscles), skull mounted (directly attached to the skull or indirectly attached with a skull clamp), table mounted (attached to the operating table), and headrest mounted (attached to the skull clamp). , We now provide an overview of each of these subgroups as they developed concurrently with advancing neurosurgical techniques.
The earliest self-retaining retractors were the soft tissue–mounted retractors. These instruments were screw driven and cumbersome. They required the surgeon to use both hands for placement, they proved troublesome to clean, and it was often difficult to access the screw once the retractor was in place. Retractors such as the Broz wound dilator ( eFig. 33.6 ) consisted of strong steel springs with tension regulated by the screw. The shortcomings of the first self-retaining retractors were obvious, and in 1905 Franz Weitlaner (1872–1944) developed his Weitlaner retractor, similar in style to what is used today. It is scissor-shaped with blades that open when the handles are closed, and it can be adjusted with just one hand.
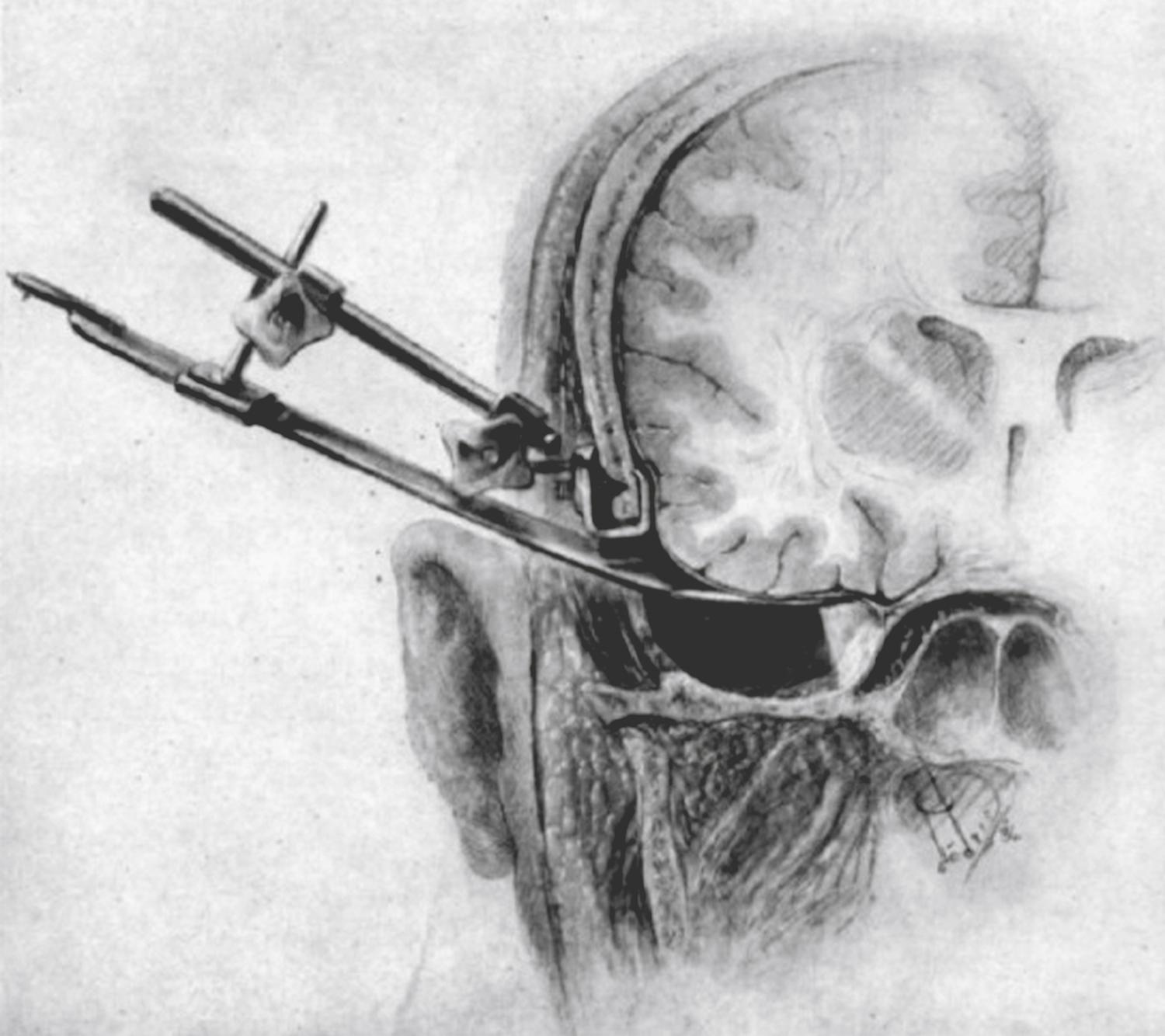
Returning to de Martel in the 1930s, we can see the development of the first skull-mounted retractor. Designed in 1930, his retractor consisted of a cylindrical metal post inserted into the skull, with a rectangular retractor blade on the opposite end. However, the problems with this device are obvious: one could not place the retractors in all craniotomy locations, given the varying thickness of the skull bone across the cranium. Even more important, each retractor placement required a separate drill hole. Norman Dott (1897–1973), known widely for his engineering skill set, helped alleviate one of these limitations by attaching multiple retractor blades to one rod. He described his Dott-Gillingham retractor as “the nice little machine we use to hold the brain out of the way when we are dealing with tumors of difficult access.” Yet again, this instrument required drilling extra holes in the skull for placement. Thus in 1937 Wallace Hamby (1903–1999) introduced his clamp that allowed attachment of retractors at the craniotomy edge, eliminating the need to drill additional holes into the skull ( eFig. 33.7 ). However, Hamby’s retractor could not be used in all locations because placement depended on skull thickness.
The Leyla retractor ( eFig. 33.8 ), designed by Mahmut Gazi Yaşargil (born 1925) in 1968, is a flexible self-retaining retractor that initially was designed to attach at the edge of the craniotomy site. Unfortunately, its arm was difficult to tighten, which caused device shifting during use, lengthy arm interference with the hands of the surgeon, and damage to the soft tissue and dura around the craniotomy clamp. Thus the Leyla retractor went from being attached at the craniotomy edge to being attached to the operating table, with a ball-and-socket joint for fixation and maneuverability to the table edge.
The 1960s onward saw the popularization of numerous surgical approaches thanks to the establishment of microneurosurgery. The pterional approach, initially used by Yaşargil starting in 1969 for intracranial aneurysms, soon became one of the most common procedures given its access to the anterior and middle cranial fossae. Yaşargil provided the era’s neurosurgeons with important advice:
“… it should never be forgotten that there is much more to microtechnique in neurosurgery than the possession of a highly perfected optical instrument. This is alone of little value without special methods of bipolar coagulation, carefully adapted instruments, and, above all, atraumatic operation techniques.”
The development of table-mounted retractors was in line with Yaşargil’s intentions. These retractors eliminated some of the problems of the aforementioned retractor systems by being secured at the operating table. The Leyla retractor was modified in 1974 by Yaşargil and Fox, who attached it to a retractor-holding bar; the instrument now had greater maneuverability on the surgical field and was less likely to interfere with the surgeon’s hands ( eFig. 33.9 ).
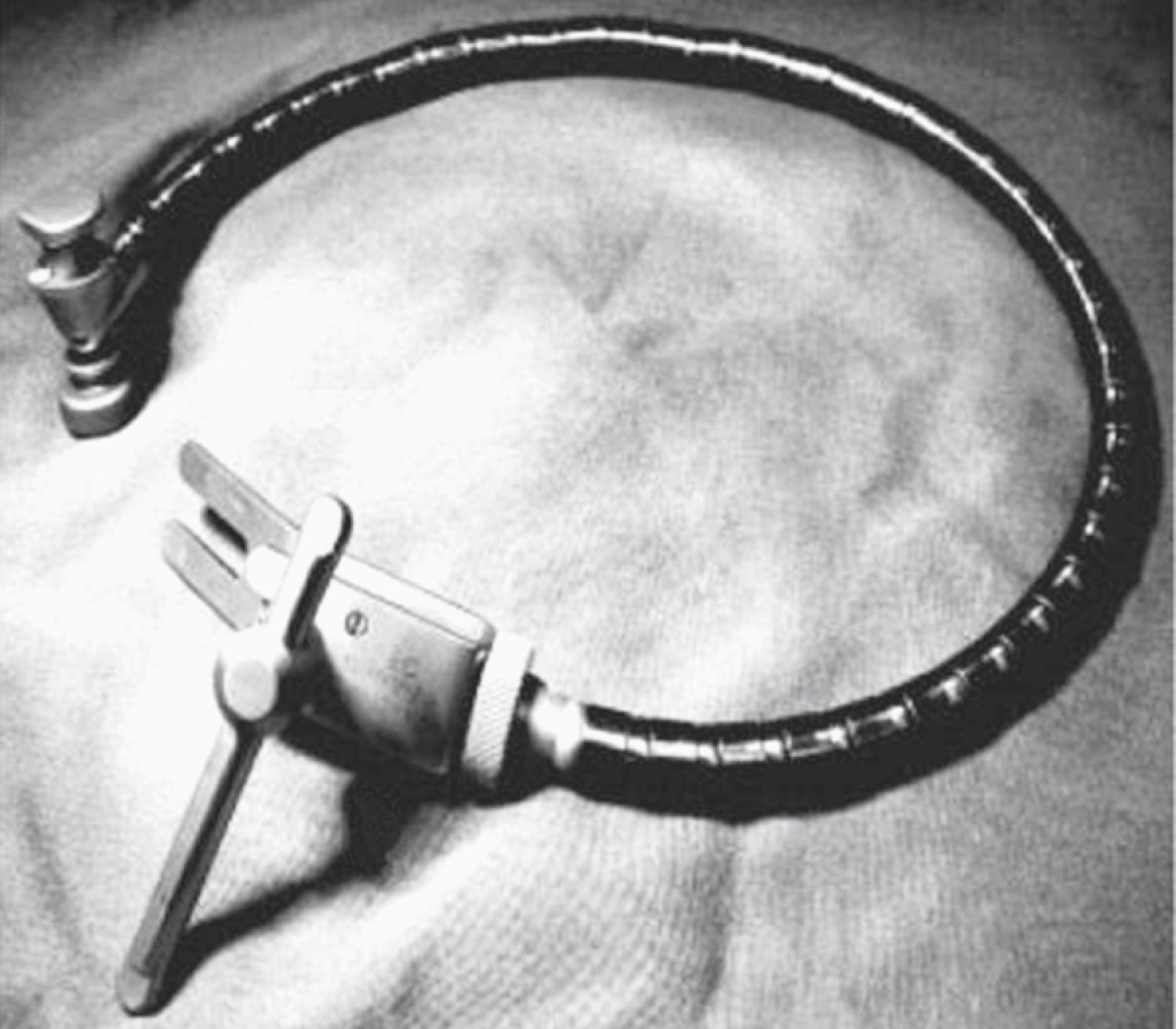
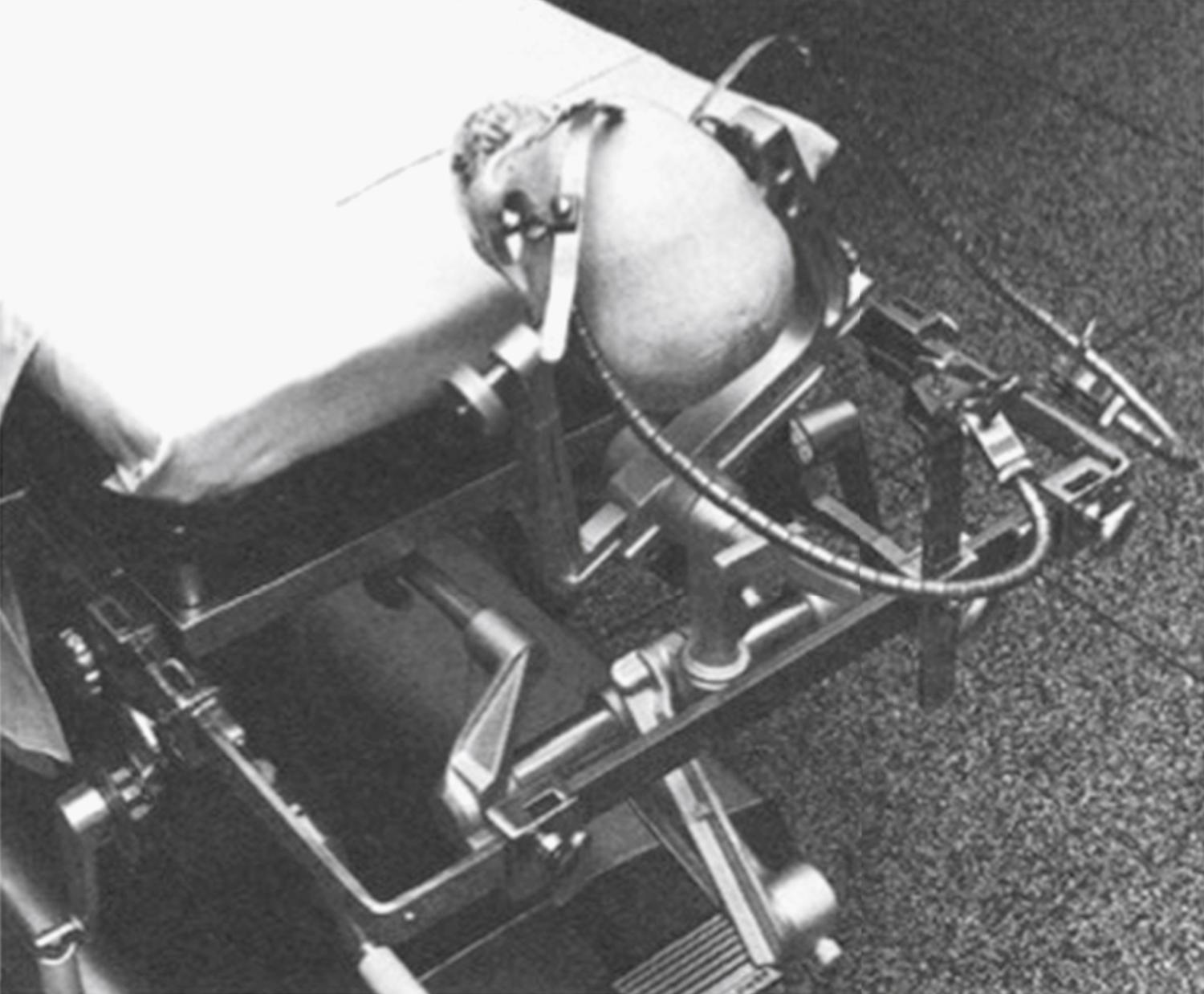
To facilitate use of the Yaşargil-Leyla retractor, in 1976 Jose Kanshepolsky crafted a U-shaped frame attached to the sliding rails of the operating table ( eFig. 33.10 ). It consisted of three metal bars attached by a series of holding clamps, with adjustable height and a movable portion that could be secured anywhere on the frame. Kanshepolsky remarked that the advantage of this holder, aside from being easily maneuverable and comfortable for the surgeon, was that the device was not clamped to the skull, “thus completely avoiding one other possible etiology for postoperative epidural hematoma.”
However, these table-mounted retractors again had their shortcomings; there was the chance of unintended retractor arm or head movement, which could result in consequential movement at the brain-retractor interface.
The stabilization of the head was a critical factor in accessing different brain regions with the operating microscope. To allow for this, Frank Mayfield (1908–1991) and George Kees (1925–2010) crafted the Mayfield General Purpose and Horseshoe Headrests in 1967 ( eFig. 33.11 ). Soon after, Mayfield and Kees developed the Mayfield three-pin skull clamp, which allowed for much better stabilization of the head for the smaller craniotomy sites that were now possible with microneurosurgery.
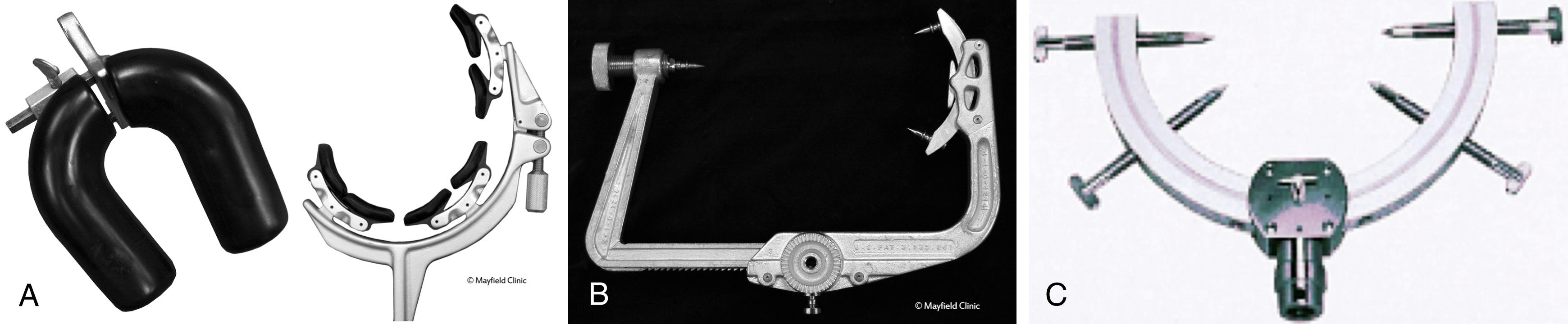
In 1978, Kenichiro Sugita (1932–1994) developed his own four-pin fixation head holder. Both the Mayfield and Sugita pin skull clamps were ideal for the operating microneurosurgeon—with the patient’s head firmly pinned to the frames, the likelihood of head movement was reduced to minimal, and these rigid head frames could also serve as attachments for additional self-retaining retractors. Numerous surgeons went on to develop retractors that attached easily to these pin skull clamps, including Mark Greenberg, Takanori Fukushima, Kenichiro Sugita, and Keiji Sano.
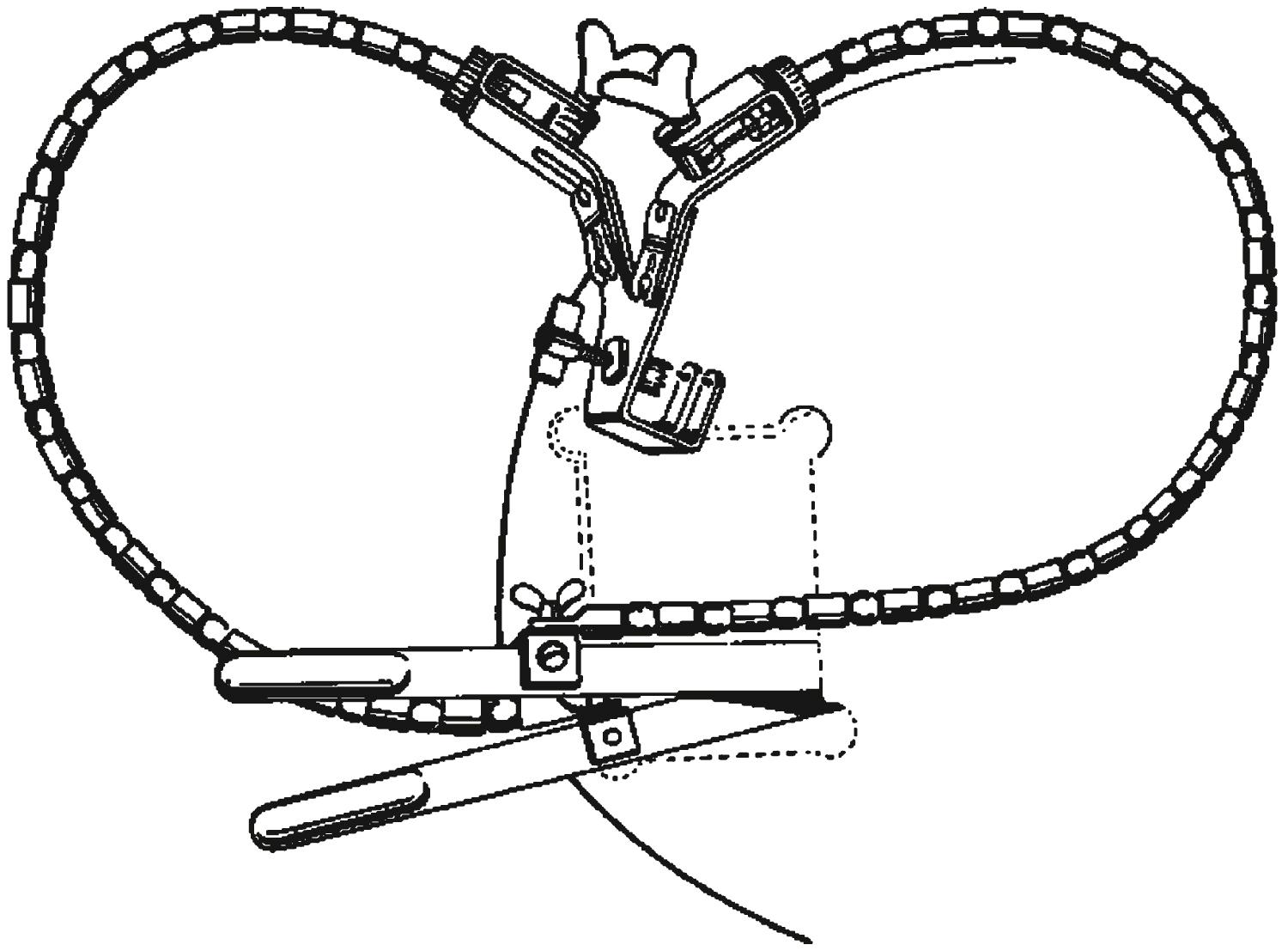
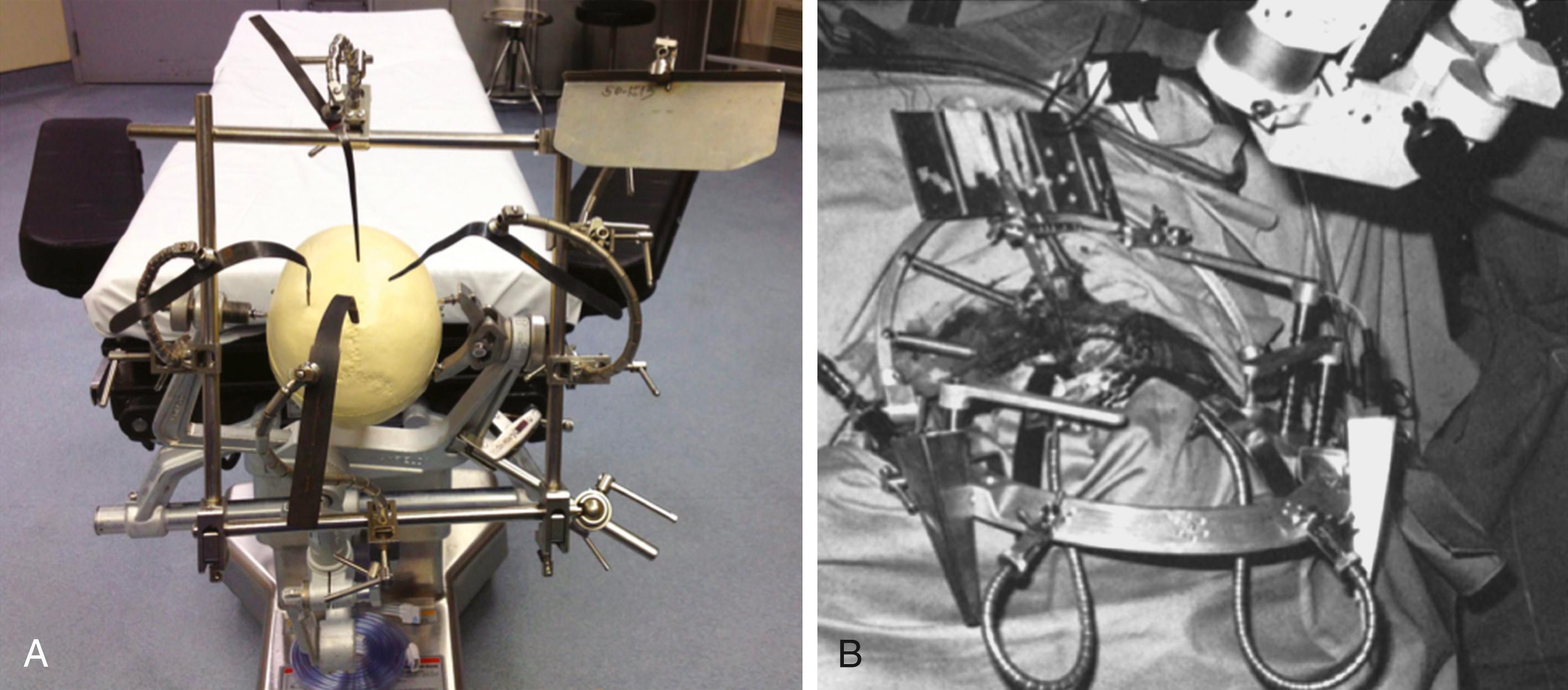
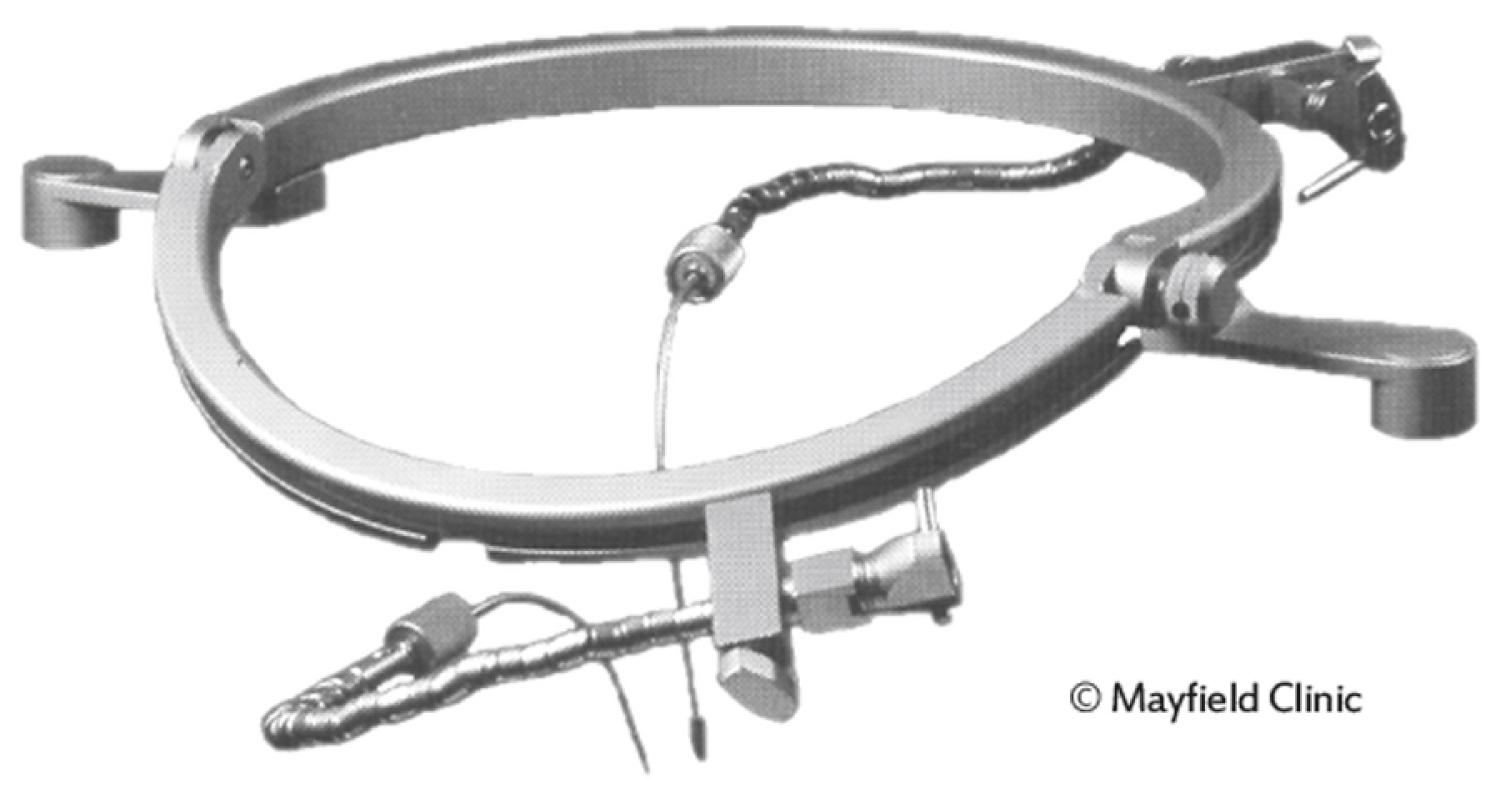
The Greenberg self-retaining retractor and handrest system remains one of the most popular retractor systems today. Developed in 1975, its design is based on functional staircase organization, with handrests for stabilization, primary and secondary clamps, retractor blades, and flexible rod holders ( eFig. 33.12 ). One advantage of the Greenberg system compared with others was that it could be used with a variety of skull clamps. In contrast, the Sugita multipurpose microneurosurgical head frame system (1977) was able to be used only with the skull clamp included with its setup (see eFig. 33.12 ). Sugita and colleagues commented that with their retractor system, even when the patient’s head required rotation during surgery, the brain retractors could be kept in the same exact position. The system contains a head holder with attachments for self-retaining retractors, microsurgical instrument holders, skin-flap spring retractors, and a plate for cotton patties. Such accessory areas of both the Sugita and Greenberg retractor systems were particularly helpful for the operating surgeon because they would allow the surgeon to keep his eyes at the microscope while easily picking up instruments without looking at them. The Budde Halo brain retractor system, developed in 1981 by Richard Budde and Jim Day, was another headrest-mounted retractor designed to attach to the Mayfield skull clamp ( eFig. 33.13 , and see for a demonstration).
The goals of retractor-based surgery are several: (1) gently create and maintain a safe corridor to surgical targets by which surgical instruments can be introduced; (2) visualize structures that are deep and usually unseen with the brain and other structures in their native state; (3) protect vital structures from injury by keeping them away from the surgical corridors of instrument transit; and (4) separate the tissue interfaces such that normal and abnormal tissue can be identified and the “surgical planes” developed. These goals must be achieved with the least amount of disruption to the structures, with the smallest possible footprint, and with no adverse sequelae. With these guiding principles as the guiding force for success, certain techniques can be employed to maximize the likelihood of achieving our goals of surgery.
The principles of retractor-based surgery are also related to patient, technical, and adjuvant factors, as discussed in the following sections.
A clear understanding of the surgical anatomy and the natural corridors that exist in reaching the target lesion are important for minimizing retraction and optimizing visualizing. Reviewing the relevant imaging findings and identifying these corridors before surgery prove helpful in the positioning of the patient.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here