Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Sampling of the cerebral tissue environment to gain clinical insight into the state of a patient's evolving neurologic health is an evolving trend in neuroscience and critical care medicine. A start to this can be traced back to Ungerstedt and Pycock; when in 1974, they published a paper studying the biochemistry of dopamine in the animal brain. They not only looked at animal behavior and motor skills, but they wanted to see real-time relevant changes in the extracellular chemical environment of the brain. Interestingly, this was accomplished in an awake and unrestrained rat by inserting a catheter through the temporal bone and subsequently through the entire brain including the caudate nuclei before passing out the other side of the skull. This novel catheter had an outer diameter of 0.25 mm and allowed molecules to diffuse in through a permeable outer sheath that was perfused with Krebs–Ringer solution at 0.5–20 μL/min. What made this an advancement in neuromonitoring was that they could see real-time changes in extracellular tritium radiolabeled dopamine based on their interventions to the test animal due to analysis of the returned catheter perfusate. They were also able to introduce amphetamine into the caudate, thereby increasing the activity of the animal through this device as well. This was the start of real-time catheter-based monitoring of the neural environment, a window into the evolving state of the brain post intervention or injury.
Later in 1992, Persson showed that longer term microdialysis monitoring of patients in the neuroscience ICU was feasible. There was no long-term morbidity associated with the catheter, though it has been noted that animal subjects have shown some mild gliosis around the catheter tracks that was attributed to unsterile probes. Persson noted that the automated catheters were easy to staff, and the self-calibrating device was dependable for clinical decision-making. The dialysate data matched clinical changes in the small patient population they were following, and this strengthened the case for incorporating cerebral microdialysis into the armamentarium of ICU care.
A panel of expert clinical and scientific reviewers met in 2003 and published a consensus statement in 2004 regarding the role cerebral microdialysis can play in advancing clinical care. This was updated in 2014 by an international group of experts that added their opinions in the setting of additional data, noting that most of the expanded data has been seen in the setting of neurocritical care. The new 2014 consensus guidelines differed from previous recommendations in several ways. The primary advances for the new guidelines involved larger membrane pores with different perfusates, better defined reference values, a tiered approach microdialysis metabolite analysis, and more specific guidance on traumatic brain injury (TBI) and subarachnoid hemorrhage (SAH) management in the ICU.
A microdialysis catheter can simply be thought of as a double-lumen tube that has fluid running through it. The crucial aspect is that the outer tube is made of a semipermeable membrane, which is the key to providing information about the extracellular environment in the brain. This membrane essentially performs a sampling dialysis of the environment outside the filter yielding biochemical information about the tissue surrounding the catheter. The outer tube consisting of the membrane wall is considered an inlet tube. Fluid travels proximally in this tube that is isotonic to the surrounding tissue. This isotonic fluid collects molecules from the tissue by diffusion as the concentration gradient facilitates transfer of the molecules in the interstitial extracellular fluid of the brain into the isotonic fluid of the outer tube of the microdialysis catheter. The concentration gradient is manipulated by a constant inflow of the isotonic fluid in the inlet tube of the catheter, which allows for constant real-time collection of molecules. Finally, the fluid flows back through the inner outlet tube of the catheter and is collected in a chamber for analysis ( Fig. 8.1 ).

Overall the first and main factor of clinical importance is the balance of extracellular molecules in relation to the infused fluid that determines what is absorbed and returned for analysis. Usually the molecules of importance are lactate, pyruvate, glutamate, and glucose. Interestingly the ratio of lactate to pyruvate is becoming increasingly more clinically significant. The second factor that is determined by the manufacturing of the catheter is the permeability of the dialysis filter that contacts the extracellular environment. The clinical impact of this is simply we can only observe what is allowed to pass through.
Most microdialysate catheters have a molecular weight filter of 20 kDa or 100 kDa. The earliest research used 20 kDa as the standard molecular weight microfilter since that can successfully collect glucose, lactate, pyruvate, glycerol, and glutamate. There has been increasing focus on larger molecular weight filters, mostly 100 kDa, which are not yet FDA approved but have the advantage of collecting larger molecules such as inflammatory cytokines. While the initial catheters used an isotonic fluid, the larger 100 kDa catheters can use a colloid perfusate that has a higher recovery rate of larger molecules for analysis, the most common initially were albumin and dextran. Some disadvantages of a colloid solution include the leakage of smaller colloid molecules from inside the catheter to outside the catheter, altering the brain tissue environment and possibly causing regional swelling; this can be avoided with the use of high-weight dextrans. Also, there is a higher influx of fluid into the catheter since the colloid perfusate has a higher oncotic pressure, which can dehydrate the extracatheter environment. One solution to this is to use human serum albumin, which can still recover larger cytokines but contributes to less dehydration in the surrounding extracellular space.
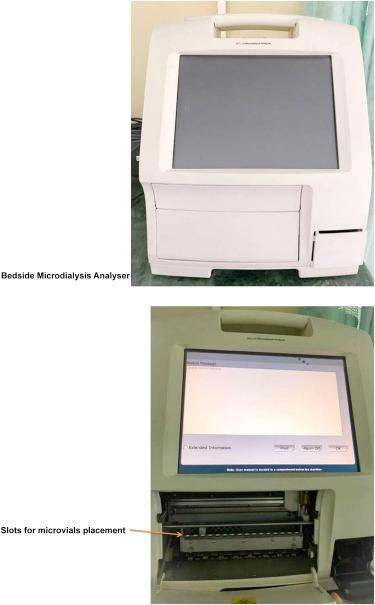
A more in-depth look takes into consideration the flow rate of the dialysate and membrane area. It is important to realize that there will not be total equilibration, and what can be studied is the relative recovery of the molecules in relation to the extracellular environment. Most catheter systems have a flow rate of 0.3 μL/min. It is recommended to not analyze the first 1–6 h of microdialysate since it is confounded by insertion trauma and the initial pump flushing. Overall trending may be of more beneficial clinical relevance due to interpatient variability and tracking of worsening disease ( Figs. 8.1 and 8.2 ).
Based on the inherent design of the catheter system, which depends on dialysate perfusion, it can only extract molecules and deliver information pertaining to the immediate surrounding tissue. For clinical use the recognition of metabolic disturbances or chemical changes in tissue that is likely to be affected secondarily to TBI or areas of vasospasm postsubarachnoid hemorrhage (SAH) are popular placement sites. Currently the goal of clinical care is to preserve as much brain as possible from devastating secondary injury, and the changes in biochemical markers in an “at risk” area could help the clinician in awareness of impending tissue damage. When there is less concern for an acute change due to secondary injury and one is looking at a broader injury such as diffuse axonal injury, most placements are in the nondominant frontal lobe. The end of the catheter has a radio opaque tip, usually gold, to help with position assessment on postplacement radiologic imaging ( Fig. 8.3 ).

Cerebral microcatheters used for dialysis have a favorable safety profile with no increased morbidity over commonly used conventional intraparenchymal pressure sensors. Catheters can be inserted by either a twist drill hole or transcranial bolt; most adverse events are related to the insertion technique instead of the catheter itself. Finally, it can be inserted during operative craniotomy as well. Some critical care units that employ cerebral microdialysis catheters have one-to-one nursing for those patients, which can affect staffing.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here