Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Minimally invasive techniques to manage biliary pathology have reduced the need for open operative intervention. Although open exploration for biliary disease has become less common, specific situations like obstructive common duct stones not amenable to endoscopic therapy or restoration of biliary-enteric continuity following resection of bile duct tumors remain indications for surgical approaches. It is important to have a thorough understanding of biliary anatomy (see Chapter 2 ) and a familiarity with various options for operative exposure and management (see Chapter 42 ). Operative techniques encompassing bile duct exploration and biliary-enteric bypass will be the focus of this chapter.
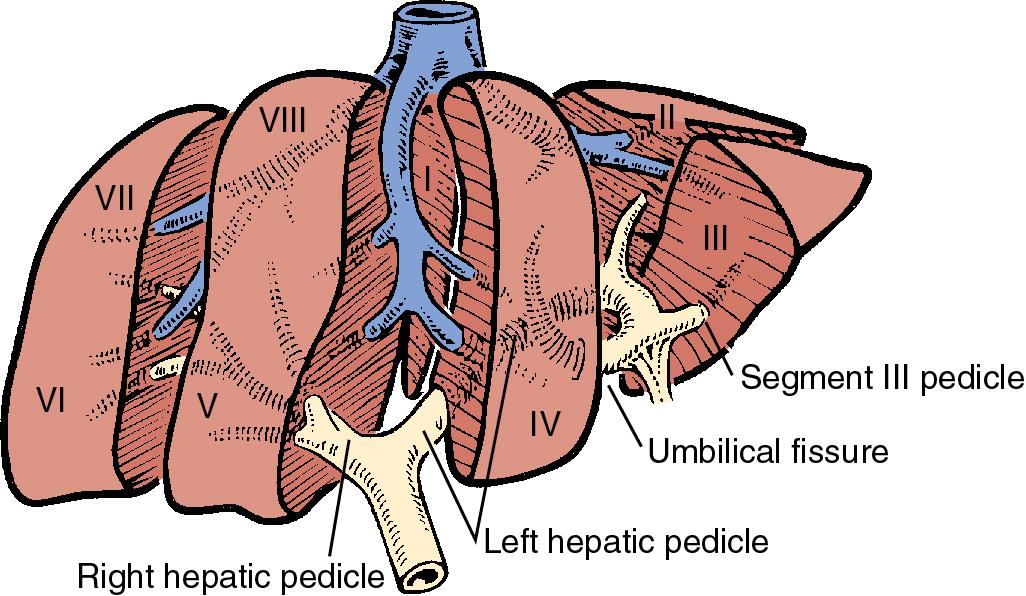
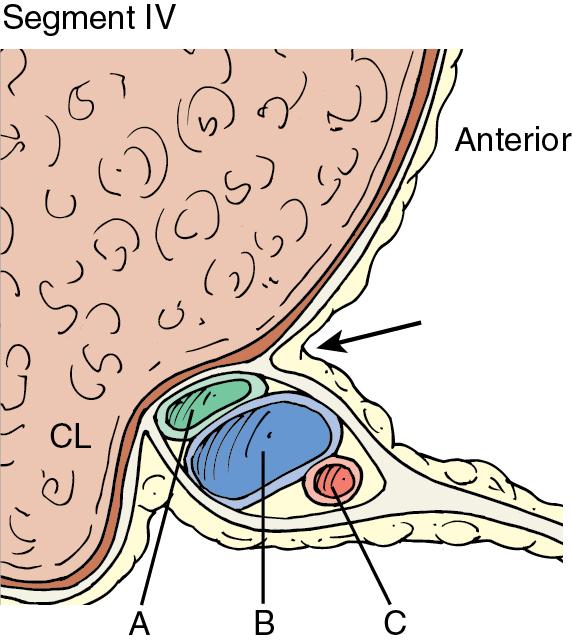
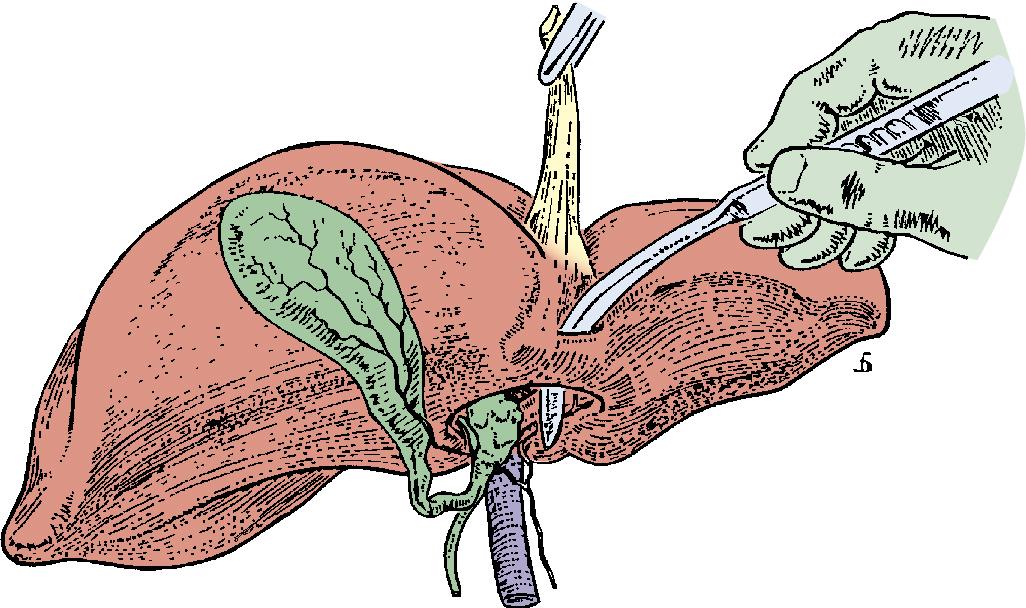
Knowledge of extrahepatic biliary anatomy and an appreciation of anatomic variants are essential for safe operative conduct (see Chapter 2 ). The intrahepatic bile ducts draining the various sections ultimately coalesce into the right hepatic duct draining the right hemiliver and the left hepatic duct draining the left hemiliver. These converge at the liver hilum to form the common hepatic duct, which is generally the most anterior structure and lies along the right border of the porta hepatis at this location. In approximately 80% to 90% of cases, the right hepatic artery courses posterior to the common hepatic duct toward the right liver; however, in a minority of cases, it can be found anterior to the duct. The right hepatic duct has a short extrahepatic segment (approximately 1.5–2 cm) in contrast to the left hepatic duct, which traverses beneath segment IVB for approximately 3 to 4 cm after exiting the liver parenchyma. When segment IVB is broad, the left hepatic duct assumes a longer extrahepatic course with a transverse orientation, as opposed to a shorter and more oblique orientation when segment IVB is narrow ( Fig. 32.1 ). The left hepatic duct and left portal vein travel within a peritoneal reflection of the gastrohepatic ligament; exposure of these structures is facilitated by lowering the hilar plate at the base of segment IVB ( Fig. 32.2 ). As the left hepatic duct and left portal vein enter the umbilical fissure, they are joined by the left hepatic artery, and vascular branches to segments II, III, and IV travel with biliary drainage from these segments. To maximize access to these structures, a bridge of hepatic tissue at the base of the umbilical fissure (bridging segments III and IV) must often be divided ( Fig. 32.3 ). The ligamentum teres (obliterated umbilical vein) at the base of the falciform ligament runs across the umbilical fissure, separating segment IV from segments II and III. Segment I hepatic ducts flow into both the right and left biliary systems, with the majority of drainage entering the left hepatic duct just proximal to common hepatic duct.
Safe operative conduct requires a close familiarity with anatomic variations of biliary drainage, as they occur in up to 25% of patients. There are a number of ductal anomalies related to the convergence of the left and right hepatic ducts and the insertion of the cystic duct. Although the left biliary system is fairly consistent, the right biliary system is prone to anatomic variation; the most common variants include the right anterior or posterior section ducts traversing a longer extrahepatic course before joining the left biliary system (see Chapters 2 and 42 ).
It is estimated that approximately 10% of the US adult population is affected by cholelithiasis, with nearly one-third of these patients requiring cholecystectomy over their lifetime (see Chapter 33 ). Approximately 10% to 15% of patients undergoing cholecystectomy have choledocholithiasis, and common bile duct stones remain the most common indication for biliary exploration (see Chapters 32 and 37 ). There are a number of techniques available for evaluation and clearance of the common bile duct, including percutaneous, endoscopic, laparoscopic, and open methods (see Chapters 30 , 31 , and 37 ). Although open common bile duct exploration (CBDE) is only necessary in a small subset of patients, it is performed at a similar rate to the laparoscopic approach: a review of the NSQIP database between 2008 and 2013 revealed that just over half of 2,635 CBDEs were performed in an open manner. This subset includes patients undergoing an open cholecystectomy (or a laparoscopic cholecystectomy converted to open) in which choledocholithiasis is suspected, patients with large or multiple stones, and patients requiring transduodenal sphincteroplasty (see Chapter 117D ). Because percutaneous, endoscopic, and laparoscopic modalities are discussed in alternate chapters, OBDE will be the focus of the following section.
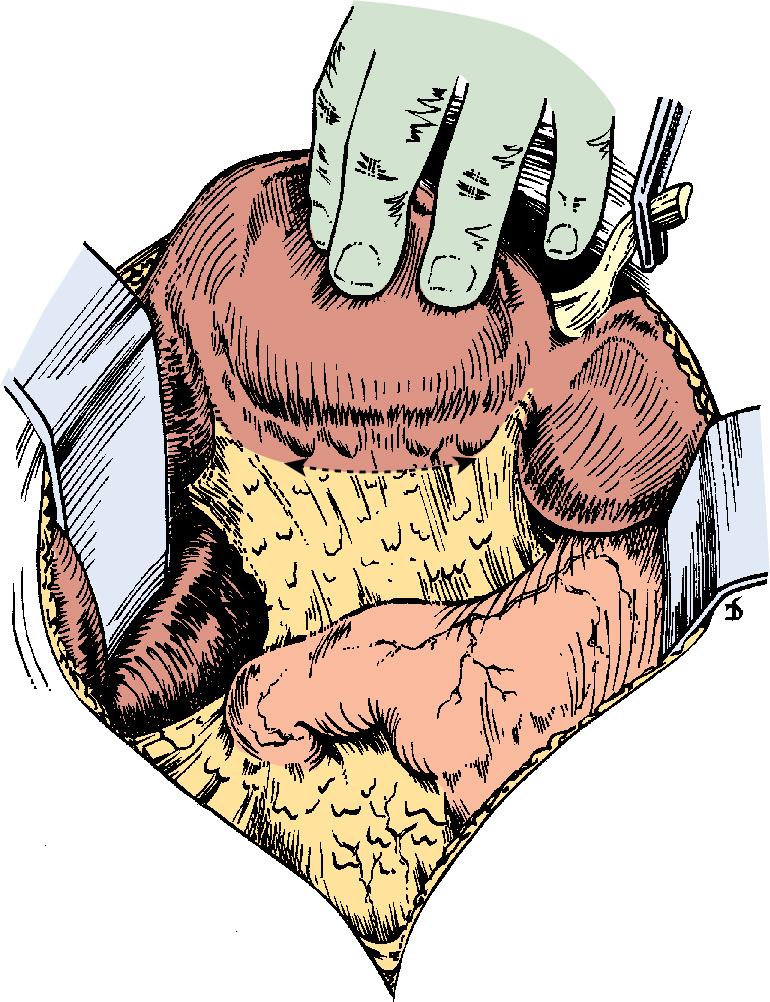
A right subcostal incision affords satisfactory exposure of the gallbladder, portal structures, and duodenum. Division of the lateral peritoneal attachments of the right colon, followed by mobilization of transverse colon mesentery off of the duodenum, provides visualization of the duodenum (see Chapters 37 and 117 ). A generous Kocher maneuver facilitates access to the common bile duct located in the lateral border of the hepatoduodenal ligament. Cephalad retraction of the undersurface of the liver at the base of segment IVB will optimize visualization of the extrahepatic biliary system ( Fig. 32.4 ) (see Chapter 119 ). Additionally, cholecystectomy can enhance exposure of the hepatoduodenal ligament and facilitate intraoperative transcystic cholangiography, which can help to delineate biliary anatomy. Dissection of the gallbladder and cystic duct also identifies the confluence of the cystic duct and common bile duct. Once the common bile duct has been successfully identified, the overlying peritoneal tissue can be dissected free to allow access to the anterior portion of the duct (see Chapters 37 , 42 , and 117D ).
The anterior aspect of the common bile duct is exposed, and two stay sutures are placed on either side of the midpoint of the planned longitudinal incision (see Chapter 37 ). The choledochotomy should be located anteriorly to avoid compromising blood vessels that typically run along the medial and lateral aspects of the common bile duct and common hepatic duct. To avoid injury to the cystic duct, the site of cystic duct insertion should be identified, as this may occur in a medial or posterior location. During the incision, caution should be taken to avoid injuring the posterior wall of the duct. The length of the choledochotomy will depend on the diameter of the duct and size of stones present with the lumen, but is generally 1 to 2 cm. Another consideration regarding the location of this incision is proximity to the duodenum; in the event that a choledochoduodenostomy may be required for appropriate drainage, every effort should be made to position the incision distally enough to permit a tension-free anastomosis to the proximal duodenum.
After choledochotomy, flushing of the duct (distally toward ampulla) with saline irrigation can result in expulsion of stones. Following this, a deflated Fogarty balloon catheter is passed distally through the ampulla into the duodenum. Once the tip of the catheter is palpated within the duodenal lumen, the balloon is inflated, and the catheter is withdrawn until resistance is encountered, indicating that the balloon is positioned against the sphincter of Oddi. The balloon is slowly and partially deflated while applying continuous tension, allowing passage into the distal common bile duct. At this point, the balloon is carefully reinflated, and the catheter is swept proximally, sweeping retained stones up toward the cholodochotomy. This process is repeated until no stones return. The catheter is then passed proximally to retrieve any stones within the common hepatic duct and intrahepatic biliary tree. Rigid instruments such as clamps or stone forceps can cause injury to the bile duct and should therefore be used with caution. A choledochoscope can be utilized to visualize remnant stones, which can be captured with basket retrieval in which the basket is passed beyond the stone, opened, and pulled back to ensnare the stone. The choledochoscope and associated basket with stone are then withdrawn. At the conclusion of duct exploration, confirmation of proximal and distal duct clearance is performed either by choledochoscopy or completion cholangiography.
When an impacted stone at the distal common bile duct cannot be cleared via choledochotomy, a transduodenal approach can be employed. A 2- to 4-cm longitudinal incision on the lateral aspect of the second portion of the duodenum allows visualization of the ampulla. Stay sutures are placed on either side of the incision to maximize exposure (see Chapters 37 and 117D ). If there is difficulty visualizing the ampulla, a small catheter can be passed through the choledochotomy into the duodenum. A sphincterotomy is performed at the 11 o’clock position to follow the direction of the bile duct, and the sphincter is incised to the level of the impacted stone or probe. This location minimizes the chance of pancreatic duct injury, which is generally located opposite the planned sphincterotomy site. The stone is then extracted, and the common bile duct mucosa is approximated to the duodenal mucosa with absorbable sutures (sphincteroplasty) to avoid postoperative papillary stenosis. Once again, a catheter is passed to ensure resolution of obstruction, and choledochoscopy or cholangiography is used to confirm the absence of residual stones. The duodenotomy is typically closed in one layer. If sphincteroplasty is not successful, the obstruction can be bypassed with a choledochoduodenostomy (discussed later).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here