Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
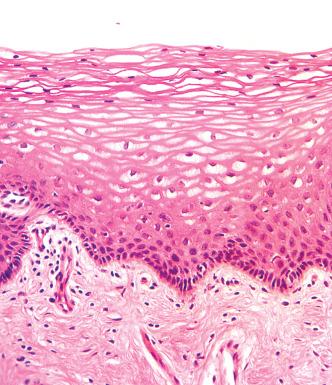
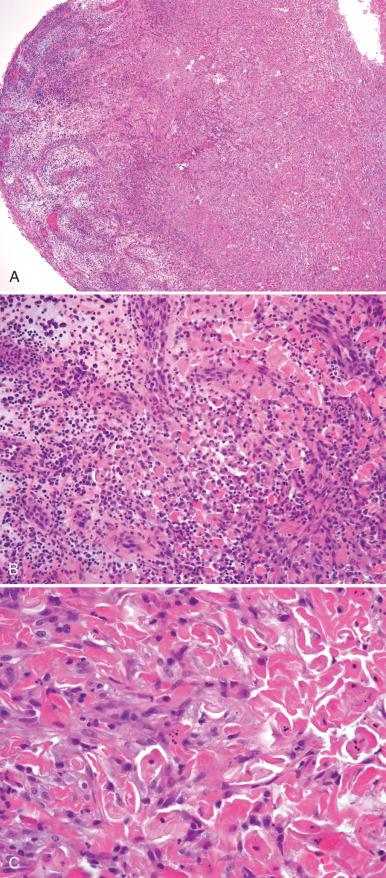
Both the anatomy and histology of the vagina vary throughout life. Traditionally, the vagina is divided into thirds—upper, middle, and lower—using pelvic, fascial, and muscular planes. The mucous membrane of the vagina is covered by a stratified, squamous, nonkeratinizing epithelium. In normal reproductive age women with cyclic menses, the superficial epithelium is glycogenated, with maximum amounts of glycogen appearing during ovulation ( Fig. 11.1 ).
The squamous epithelium is composed of four layers :
The basal layer is a generative layer with minimal cell turnover, attached to the basement membrane.
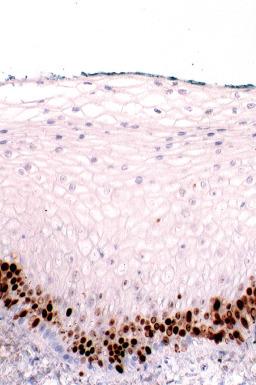
Above this is the suprabasal layer with larger round cells containing desmosomes. At the interface with the basal layer of cells undergo transient DNA proliferation, which defines the cell population destined for differentiation ( Fig. 11.2 ).
The upper intermediate layer contains large, rounded, and somewhat flattened cells with glycogen.
The final layer is the superficial layer containing small dense nuclei (see Fig. 11.1 ).
The vagina is prone to a number of disorders, including infections, soft tissue disorders, and epithelial neoplasms. These are largely discussed in Chapter 2, Chapter 4, Chapter 9, Chapter 12 , many of which have recently been reviewed. This chapter deals with benign disorders, including some infections specific to this site.
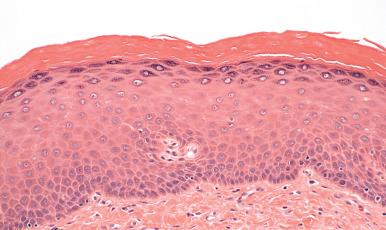
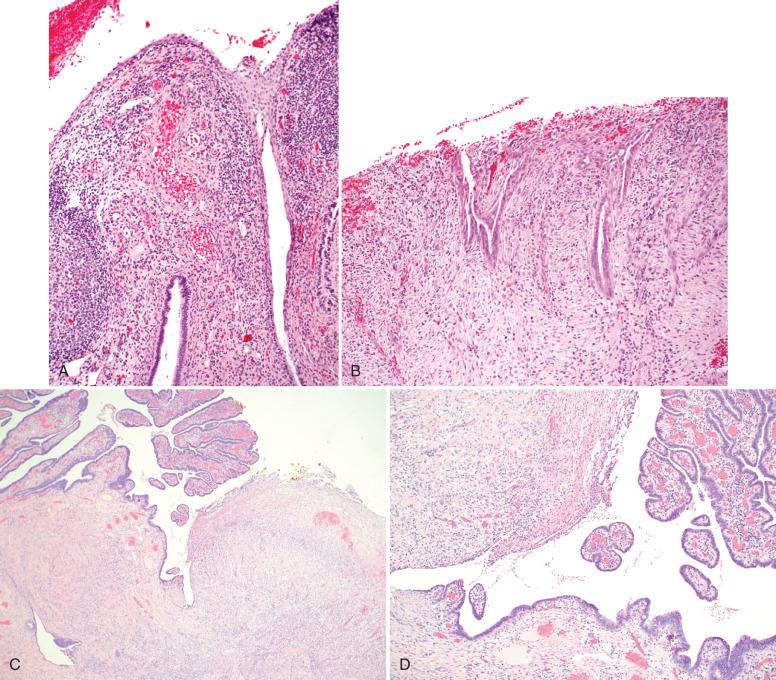
The most common alterations of the vaginal mucosa occur as a consequence of prolapse and atrophy. Vaginal prolapse is due to loss of support of the ligaments that suspend the vagina, usually as a consequence of prior pregnancies. Signs and symptoms of vaginal prolapse include fullness in the region of the bladder, vagina, and rectum, lower abdominal discomfort and backache, vaginal discharge and, most notably, increased frequency of urination and inadequate bladder emptying. At times, edema may be associated with vaginal prolapse ( Fig. 11.3 ).

The pathologist often encounters vaginal specimens from patients with prolapse during the evaluation of routine vaginal hysterectomies. The histopathologic findings in prolapse typically include mild epithelial acanthosis and hyperkeratosis ( Fig. 11.4 ). If epithelial erosion has taken place, reparative changes are also present and can be seen on cytologic evaluation of prolapse. Similar findings are seen in patients who are using pessaries. The pathologist who is familiar with these findings will usually have little difficulty distinguishing them from vaginal intraepithelial neoplasia (VAIN; see Chapter 12 ) inasmuch as there is minimal nuclear atypia. In the presence of inflammation or repair, excluding VAIN may be more problematic but can be done easily with immunostaining for p16, if needed.
The principal consequence of prolapse is symptomatic patient discomfort. Women with symptomatic prolapse can be managed with pessary placement or corrective surgery. Factors to consider when operating on this population include the location(s) of anatomic defects, severity of prolapse symptoms, activity level of the patient, and concerns regarding the durability of the repair. Cancer has been reported in association with vaginal prolapse, but is extremely rare and is not considered a risk with this disorder.
Atrophic vaginitis usually occurs in the postmenopausal patient, when estrogen levels are low and no longer support glycogenization of the vaginal epithelium. However, it is also common in the reproductive years (postpartum during breast-feeding). In atrophic vaginitis, the vaginal pH is often more than 5.0, and the wet prep contains a profuse number of parabasal and inflammatory cells. Symptoms include vaginal dryness, itching, and vulvodynia, usually localized.
The classic appearance of atrophic vaginitis on gross examination consists of small punctuate hemorrhages in the mucosa. A serosanguineous or watery discharge may be present, and a wet prep reveals parabasal cells and polymorphonuclear leukocytes (PMNs). Cytologic smears may be difficult to interpret because parabasal cells with an increased nuclear-to-cytoplasmic ratio predominate. These patients are often referred for colposcopy, revealing a thin friable vaginal epithelium with enhancement of the underlying vasculature. Lugol solution uptake is minimal because of the lack of estrogen-induced glycogen in the epithelium, resulting in a diffuse light brown to yellow color.
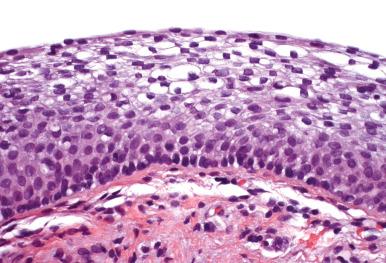
The histopathology of atrophic vaginitis is characteristically that of a nonglycogenized epithelium ( Fig. 11.5 ). The epithelium may be attenuated, comprised of no more than four to six cell layers, but may be normal in thickness, with uniform, slightly pale to homogeneous nuclei and smooth, uniform-appearing chromatin. If coexisting inflammation is present, the distinction between atrophic vaginitis and HSIL may be difficult but can be made easily by immunostaining for a proliferative marker, such as Ki-67 (see Chapter 12 ). In general, atrophic vaginitis is more problematic clinically, colposcopically, and cytologically than histologically ( Fig. 11.6 ).
The general treatment of vaginal atrophy is hormone therapy. Many forms are available, including estrogenic preparations administered vaginally (e.g., creams, tablets, estradiol-releasing ring), intravaginal dehydroepiandrosterone (DHEA), and oral hormone therapy. At times, nonhormonal therapy is recommended. Vaginal moisturizers and lubricants may also be beneficial. Following estrogen replacement, parabasal cells will mature into intermediate and superficial squamous cells, returning to a normal colposcopic appearance.
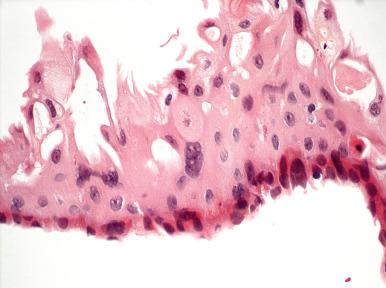
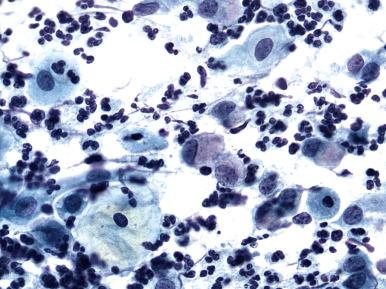
Radiation therapy for cervical, vaginal, and occasionally endometrial cancers can have serious consequences. The vaginal mucosa tends to be thin and friable, characteristic of atrophy, and colposcopic evaluation can be difficult. Typically, there is minimal uptake of Lugol solution, a sign of poorly glycogenized epithelium. Irregular vessels may appear, making interpretation difficult. Papanicolaou (Pap) smear changes of radiation therapy can be confused with vaginal intraepithelial neoplasia or cancer on cytologic interpretation. These changes include cytoplasmic vacuolization, nuclear enlargement, and multinucleation ( Fig. 11.7 ). However, the nuclear-to-cytoplasmic ratio remains low, and chromatin remains smooth rather than coarse.
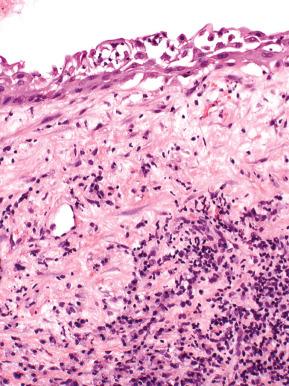
In addition to atrophic changes, radiation induces ischemic changes via its effects on the vasculature. In severe cases, superficial necrosis and repair are present ( Fig. 11.8 ). Significant vaginal scarring can occur following radiation. Younger age and higher tumor dose are associated with a higher grade of stenosis.
Prophylactic vaginal dilation prior to starting the radiation, during radiation, and following radiation treatment has been recommended. One factor associated with success with vaginal dilation is motivation. It is important to provide sufficient patient information and support for this process to be successful. Severe complications of radiation therapy include rectovaginal fistula and vesicovaginal fistula.
Lichen sclerosus is a common vulvar condition. However, it is rarely seen on the vagina. To date, there have been two reports of vaginal lichen sclerosus developing in menopausal patients . Intravaginal steroids are the initial treatment for this condition.
Benign lesions following hysterectomy include the following, in decreasing order of frequency.
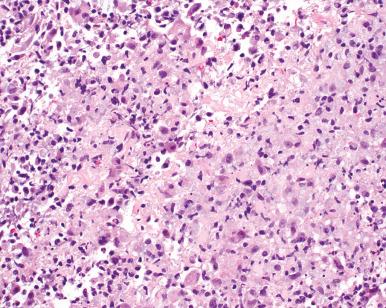
Granulation tissue is a common cause of postsurgical vaginal bleeding and frequently is biopsied, particularly if there are concerns stemming from a prior surgical procedure for a neoplasm. Typically, granulation tissue appears as a raised red, lobular lesion in the upper vagina, near or within the sutured cuff. The histologic features are characteristic, with abundant vascular growth, epithelial erosion, and intense inflammation ( Fig. 11.9 ). The process evolves (heals) over time, with a greater proportion of the lesion being occupied by fibrous tissue with less prominent vessels.
In some cases, abundant squamous cells can be trapped within the granulation tissue, giving the false impression of a squamous neoplasm. However, at higher power, the two components can be distinguished ( Fig. 11.10 ).
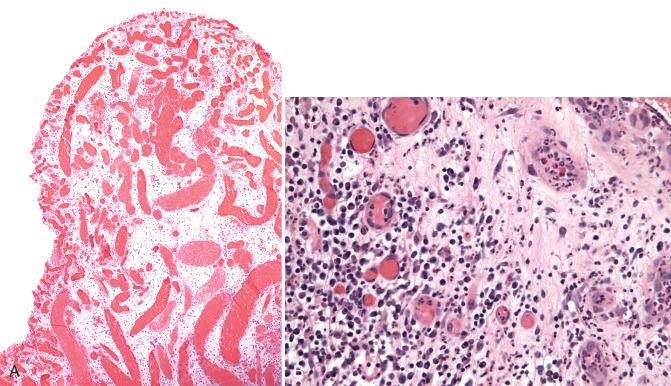
Tubal prolapse occasionally occurs following a hysterectomy, when the tubes are fixed near the apex of the vaginal cuff. It usually follows vaginal hysterectomy but also occurs with an abdominal or laparoscopic hysterectomy if the tubes are spared. Patients may present with abdominal pain, dyspareunia, postcoital bleeding, and/or vaginal discharge.
A small nodule resembling granulation tissue is visible at the vaginal apex. A cytologic diagnosis of tubal prolapse is rare. The cytologic appearance of a prolapsed fallopian tube includes classic columnar cells with cilia and sheets of cells with small granular uniform nuclei in an orderly arrangement. Squamous metaplasia, with nuclear enlargement and an increased nuclear-to-cytoplasmic ratio corresponding to reactive atypia, but with fine and evenly distributed chromatin and smooth nuclear contours, may occur.
The biopsy discloses tubal plicae with a bland tubal epithelial lining ( Fig. 11.11 ). However, misdiagnosis as neoplasia can occur if the tubal epithelium is not recognized. Moreover, fallopian tube prolapse has been associated with an exuberant angiomyofibroblastic stromal response. The richly vascularized stroma is arranged in a retiform pattern, with mildly atypical glandular inclusions derived from tubal epithelium. If the tubal glandular component is overlooked, this might be erroneously diagnosed as a mesenchymal lesion of the vagina, such as vaginal fibroepithelial polyp, angiomyofibroblastoma, or aggressive angiomyxoma (see Chapter 9 ).
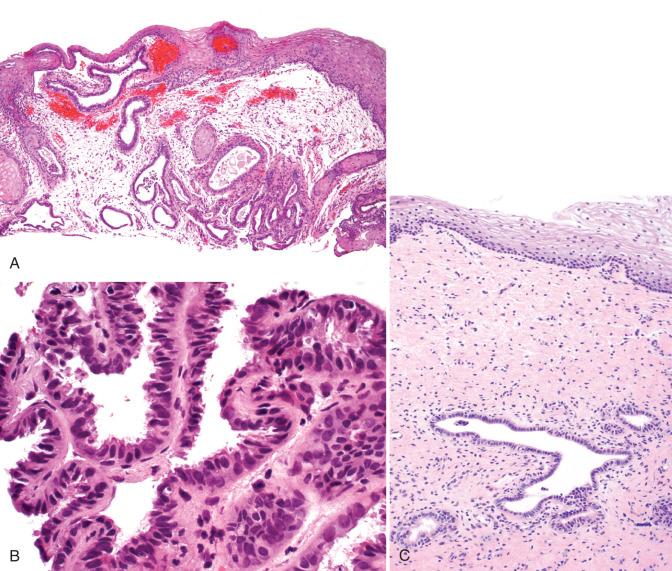
The association of in utero exposure with diethylstilbestrol (DES), vaginal adenosis, and clear cell adenocarcinoma of the vagina was revealed in the early 1970s. Adenosis is found in about one-third of women exposed to DES in utero and is responsible not only for vaginal abnormalities, but also uterine structural anomalies (see Chapter 1 ). The principal defect consists of the congenital presence of columnar epithelium of the endocervical or endometrial type in the vaginal apex. Vaginal adenosis was appreciated prior to the DES era but was extremely rare.
Colposcopic findings in vaginal adenosis consist of a red and granular vaginal lesion, which fails to stain with iodine and that may be continuous with the cervix. The upper third of the vagina is almost always affected, the middle third is involved in 10% of cases, and the lower third in 2% of cases. The histologic findings include benign endocervical glandular epithelium, endocervical epithelium with squamous metaplasia, and endocervical epithelium, with tubal endometrioid metaplasia, the latter characterized by ciliated cells ( Fig. 11.12 ). If the glandular lesion is large, additional and less common findings include papillae (papillary adenosis), microglandular hyperplasia, particularly if the patient has taken oral contraceptives or been pregnant, Arias-Stella reaction, intestinal metaplasia, and varying degrees of glandular atypia.
Adenosis is rarely complicated by the development of vaginal clear cell adenocarcinoma, which historically has occurred in 1/1000 to 5000 exposed individuals.
A curious finding in cytologic preparations of postmenopausal women following hysterectomy is benign glandular cells in the vaginal vault ( Fig. 11.13 ). Explanations for these cells include the following: (1) an intact cervix (supracervical hysterectomy) ; (2) vaginal endometriosis ; (3) mesonephric duct remnants and cysts; (4) vaginal adenosis; (5) fallopian tube prolapse ; (6) reparative fibroblasts in ulcers and granulation tissue; (7) rectovaginal fistulae; (8) adenocarcinoma (recurrent or metastatic); (9) exfoliated reparative squamous parabasal and basal cells resembling columnar-type cells (goblet cell metaplasia) ; and (10) cytologic effects following the use of 5-fluorouracil (5-FU). Most cases of benign columnar cells cannot be explained and appear to be of little clinical consequence if cytologically unimpressive.
Cysts of the vagina are common and are generally benign. Clinically, they may be single or multiple. At times, imaging (ultrasound, voiding cystourethrogram [VCUG]), computed tomography (CT), or magnetic resonance imaging (MRI) may be required to characterize the lesion further. It is important to rule out cystoceles or enteroceles, which can mimic a vaginal cyst.
The principal types of vaginal cysts include the following.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here