Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Intra-axial lesions invading, or located in, eloquent areas related to the language cortex, especially in the dominant hemisphere. The infiltrative rather displacing nature of gliomas makes this approach very suitable for low-grade gliomas (astrocytoma, oligoastrocytoma or oligodendrogliomas) and high-grade gliomas.
The goal of intraoperative speech mapping is:
to determine the limits of the resection and the best surgical corridor to approach the lesion.
to allow maximal resection while limiting functional impairment of eloquent areas.
An increasing body of evidence supports longer survival and better quality of life in low-grade gliomas (LGG) after gross total resection or smaller residual tumor volumes.
Intraoperative mapping and functional imaging have transformed into resectable some brain tumors previously considered inoperable. They also have considerably decreased the postoperative functional deficits.
Non-cooperative patient because of disease or psychosocial issues.
Inability to follow commands or to reproduce the speech tests in the preoperative training.
Anticipation of airway compromise during the awake portion (e.g. morbid obesity, medically intractable seizures, or sleep apnea).
Comorbidities that could promote brain herniation through the craniotomy window (e.g. anticipated intracranial hypertension).
Neuropsychological and language evaluation may be helpful to detect complex neurologic symptoms and to determine the behavioral tasks (paradigms) that will be used for the functional MRI (fMRI) and intraoperative mapping.
Neuroimaging considerations ( Figure 1.1A–F ): Positron emission tomography (PET) and fMRI can be used for surgical planning and to localize the eloquent areas preoperatively. If those tests indicate that the lesion is involving functional language cortex or is adjacent to it, an awake craniotomy with intraoperative speech mapping is usually required.
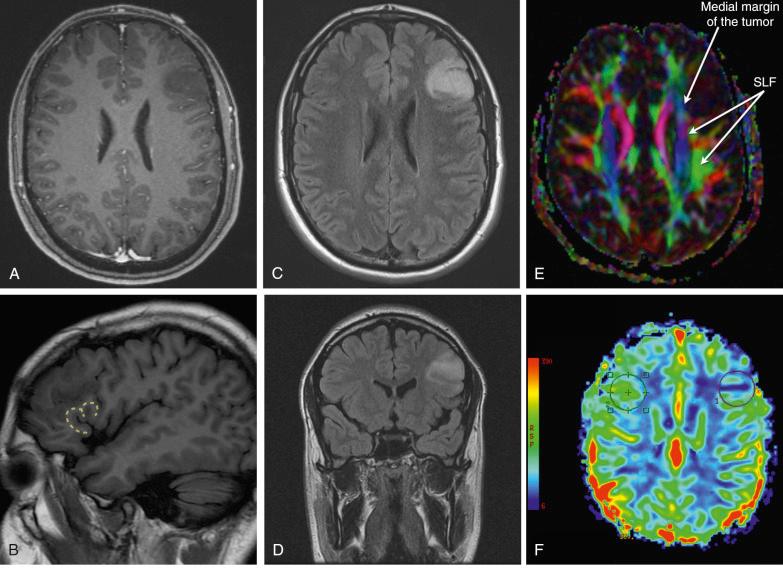
fMRI is preferred because it allows a noninvasive cortical mapping avoiding the use of radioisotopes. fMRI measures relative changes in oxygenated and deoxygenated hemoglobin. Especially in language mapping, fMRI or PET cannot distinguish between essential and complementary but non-essential areas. fMRI can guide the surgical planning but cannot be the sole means to locate the eloquent areas and to establish the resection margins.
With the combination of different speech paradigms, fMRI can give an estimate of the localization of eloquent areas related to language cortex and hemispheric language lateralization or codominance.
Despite its limitations, diffusion tensor imaging (DTI) can also be useful to assess the white matter tracks. The most important tracks related to speech are the superior longitudinalis fasciculus (SLF), the arcuate fasciculus and the inferior fronto-occipital fasciculus (IFOF). Those fascicles conform a dorsal pathway (phonological processing) and a ventral pathway (semantic processing).
Regions of interest: Broca's area (pars triangularis and opercularis of the inferior frontal gyrus), Wernicke's area (posterior temporal and inferior parietal areas in the angularis and supramarginal gyrus), supplementary motor area (superior frontal gyrus), dorso-lateral prefrontal area and anterior insular cortex.
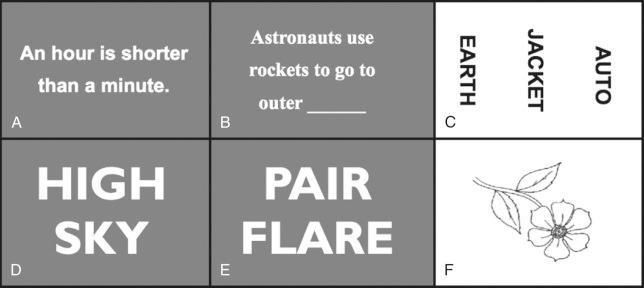
Behavioral tasks (paradigms): Spontaneous speech, fluency, counting, object naming, spelling, reading, writing, comprehension, silent word generation, rhyme detection, semantic decision, repetition, word-stem completion and switching from one language to another in bilingual patients ( Figure 1.2A–F ).
The functional maps can be fused with the morphologic regions depicted by standard MRI ( Figure 1.3A–D ).
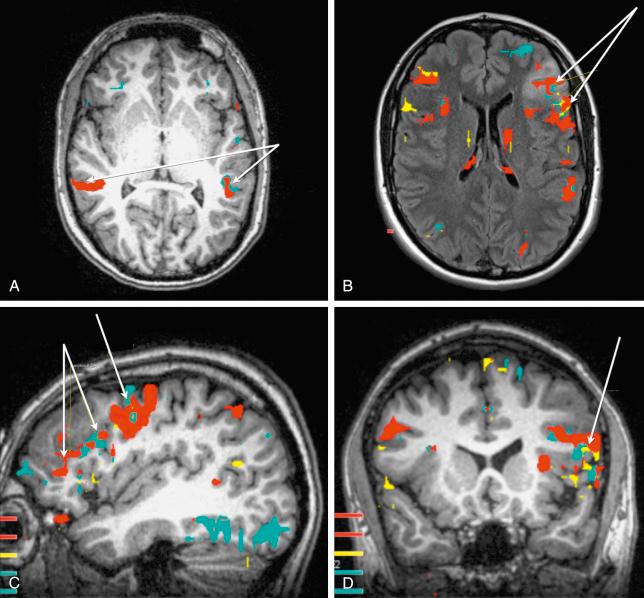
Preoperative redistribution and plasticity of the language function: In some cases, function is within the tumor, limiting the chances to perform a gross total resection. The eloquent areas can also be redistributed around the lesion, favoring wider resections. In optimal cases, functional compensation by remote regions already exists preoperatively, favoring a complete macroscopic removal of the tumor.
This surgery is performed under sedation with propofol plus fentanyl or dexmedetomidine without intubation or with laryngeal airway. The patient will be sedated from the positioning time to the dural exposure monitoring with BIS (bispectral index) or entropy to control the moment of awakening. Then the patient is woken up to perform several tasks during brain mapping and tumor resection.
When mannitol is needed, a dose of 0.5 g/kg is administered. Higher doses of mannitol may cause nausea. Alternative options to decrease brain edema are steroids and hypertonic solutions.
Body temperature should be maintained at about 36–37 °C.
Possible adverse effects caused by electrical stimulation are induced seizures and edema.
The major complaints during the awake portion are neck pain and stiffness, restlessness and dry mouth. These can be alleviated with good positioning, water-soaked sponges and slight changes in position of the arms and legs.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here