Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Chronic pruritus can be debilitating, causing great distress to patients.
A patient with no obvious reason for having chronic itch and no primary skin rash needs a full workup with a thorough history, physical examination, and laboratory and/or imaging studies to rule out underlying disease.
The pathophysiology of chronic itch involves a phenomenon of neural sensitization, which takes place at the level of the skin, spinal cord, and brain.
Itch, or pruritus, is a sensation resulting in a desire to scratch.
Chronic itch is defined as pruritus lasting for more than 6 weeks. It can be generalized or localized to a certain area of the body and can cause great distress to patients. Suffering from chronic pruritus can lead to sleep disturbances, mood changes, symptoms of anxiety and depression, and can interfere with daily activities or work.
Yosipovitch G, Bernhard JD. Chronic pruritus. N Engl J Med . 2013;368(17):1625–1634.
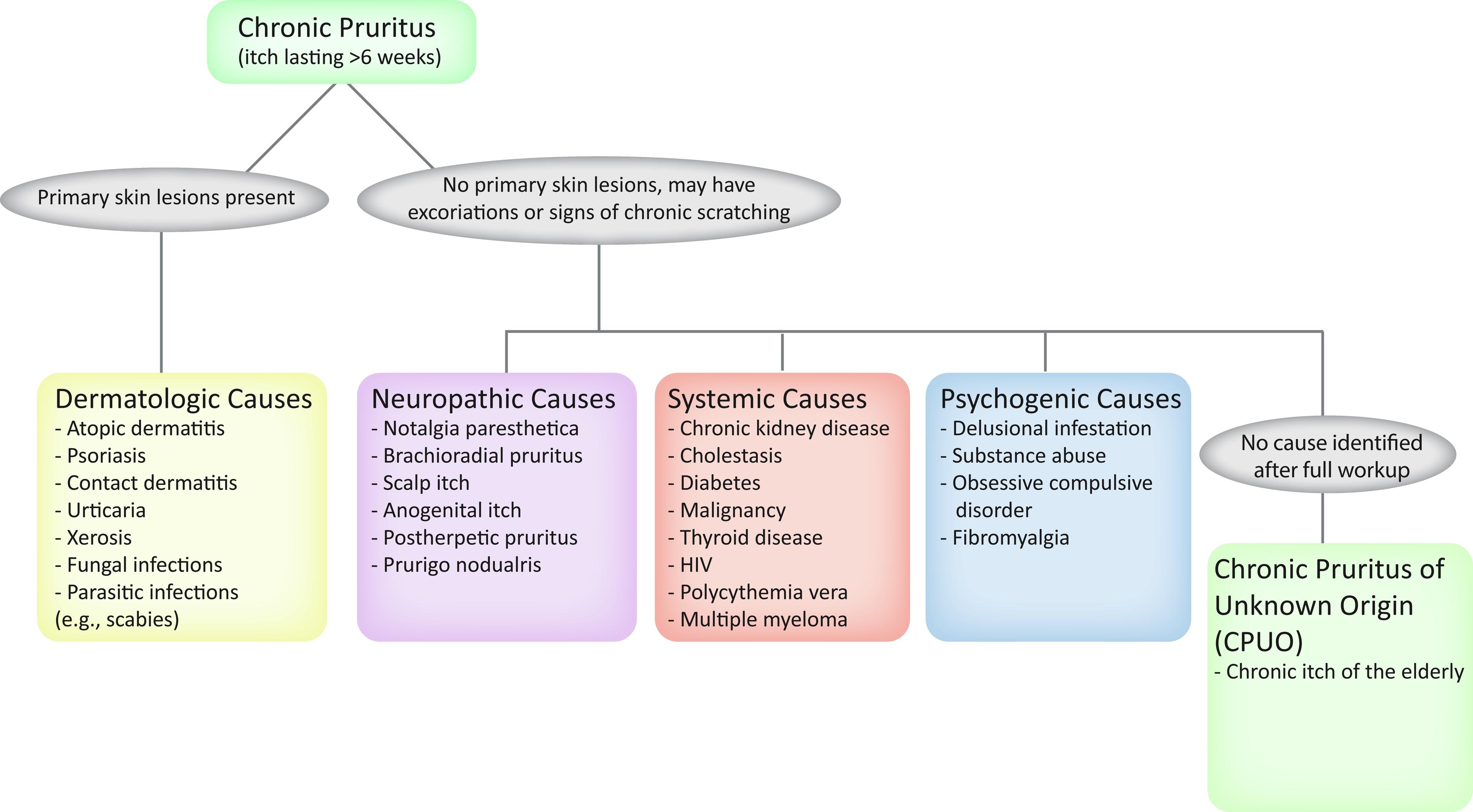
Itch can be classified into four different categories: dermatologic, systemic, neuropathic, or psychogenic ( Fig. 68.1 ). Dermatologic causes of pruritus show primary skin lesions and include conditions such as atopic dermatitis, psoriasis, scabies, contact dermatitis, and urticaria. Systemic, neuropathic, and psychogenic causes of chronic itch do not have primary skin lesions, but lesions from scratching may be present. Systemic causes of pruritus include chronic kidney disease, cholestatic disease, human immunodeficiency virus (HIV), and Hodgkin’s disease, to name a few. Neuropathic causes of pruritus include conditions such as brachioradial pruritus (BRP), notalgia paresthetica, and postherpetic pruritus. Finally, psychogenic causes include delusional infestation and substance abuse.
Yosipovitch G, Bernhard JD. Chronic pruritus. N Engl J Med . 2013;368(17):1625–1634.
Ständer S, Weisshaar E, Mettang T, et al. Clinical classification of itch: a position paper of the international forum for the study of itch. Acta Derm Venereol . 2007;87(4):291–294.
Neural sensitization is important when discussing the pathophysiology of chronic itch. Neural sensitization refers to an increase in the sensitivity of itch-selective neurons, which decreases the threshold for itch sensation. In the skin, inflammation and abnormal innervation can lead to neural hypersensitivity. In the peripheral nervous system and skin, overactivation of nerve growth factor, substance P, and neurokinin-1 receptor also contributes to neural sensitization. Dysfunctioning inhibitory circuits and imbalance in kappa- and mu-opioid receptors, as well as overactivity of neurokinin-1 receptor, lead to neural sensitization in the spinal cord. Increased activation of certain areas of the brain, such as the anterior cingulate cortex, posterior cingulate cortex, and prefrontal area, may lead to neural sensitization in the brain. Overall, this phenomenon is part of the mechanism perpetuating chronic itch and contributes to symptoms such as alloknesis and hyperknesis.
Yosipovitch G, Rosen JD, Hashimoto T. Itch: from mechanism to (novel) therapeutic approaches. J Allergy Clin Immunol . 2018;142(5):1391.
Alloknesis is when a nonpruritic stimulus causes itch, while hyperknesis is when a pruritic stimulus causes an enhanced, or greater than normal, sensation of pruritus.
When a patient presents with complaints of itching without a rash, a thorough history and physical examination are warranted. From there, you can decide what laboratory or imaging tests are necessary, if any. Important questions to ask include:
When did the itch start?
Where is the itch located? Is it localized to a certain area or is it generalized?
In the last 24 hours, how would the patient rate the itch on a scale of 0 to 10 on average and at its worst severity?
How many hours during the day is the patient itchy?
Is the patient itchy in the morning, afternoon, and/or nighttime?
Does anything alleviate the itch? What tends to aggravate the itch?
What other medical problems does the patient have? (e.g., neuropathy, chronic kidney disease, chronic cholestatic/liver disease, diabetes, cancer, psychiatric illnesses)
What medications is the patient taking?
Does anyone else feel itchy around them or in their home?
Does the patient have a history of trauma or surgeries of the back, neck, or sacral area, or any spinal cord injury or stenosis?
When a patient presents with itch present for more than 6 weeks, you must first take a full clinical history and physical examination. This includes a detailed medication history and review of systems, with attention to symptoms that may point to an underlying systemic illness.
On physical exam, look for primary skin lesions that may point to a dermatologic cause of pruritus, such as eczematous lesions of atopic dermatitis or silvery, scaly plaques of psoriasis. Be sure to distinguish secondary skin lesions from primary lesions, for excoriations, prurigo nodules, and nonspecific dermatitis may be simply from scratching. Undress the patient to examine the genital area to rule out scabies.
If no primary skin lesions are found, consider a nondermatologic cause for pruritus. Make sure to palpate lymph nodes in the axillary and inguinal regions. Depending on what is found on history and physical examination, you may want to order laboratory and imaging tests. Laboratory tests may include a complete blood count (CBC) with differential, liver function tests (LFTs), thyroid function tests, creatinine level, erythrocyte sedimentation rate, and HIV test. Imaging tests may include chest x-ray (CXR) or imaging of the spine if you suspect a neuropathic cause, such as notalgia paresthetica or BRP.
Yosipovitch G, Bernhard JD. Chronic pruritus. N Engl J Med . 2013;368(17):1625–1634.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here