Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Medical and other adjunctive agents and associated surgical techniques used intraoperatively and/or preoperatively and postoperatively to modulate the wound healing associated with glaucoma surgery in an effort to increase its success.
Mitomycin C.
5-Fluorouracil.
Topical intraoperative use.
Subconjunctival injected preoperative and postoperative use.
Most commonly indicated for patients with elevated risk of failure, including previous surgery, neovascular glaucoma, and black African descent.
May increase the incidence of hypotony.
May increase the rate of bleb-associated complications, including endophthalmitis.
Simple changes in application and surgical technique markedly reduce bleb-related and other complications, including hypotony.
Essential for success of externally draining contemporary microimplants.
Outcomes of glaucoma filtering surgery have been transformed by improved surgical techniques and the innovative use of antifibrotic strategies that include the local administration of antimetabolites, which reduce scarring after glaucoma filtration surgery. Antimetabolites were used mainly in high-risk patients during the 1980s. A more recent survey demonstrated that mitomycin C (MMC) is used by 97.2% of the surveyed glaucoma surgeons routinely during trabeculectomy. It is now well recognized that a target intraocular pressure (IOP) at the lower end of the normal range (around 10 mm Hg) will arrest glaucomatous progression in the majority of patients over a decade, particularly with advanced disc damage. Incisional surgery, such as trabeculectomy with drainage to the subconjunctival space, is the main treatment option if these IOP levels cannot be achieved with maximally tolerated medical therapy.
The concept that the healing response should be modulated to achieve a target IOP of as close to 10 mm Hg after subconjunctival surgery has become the accepted consensus. The healing response is the major determinant of long-term IOP levels after glaucoma surgery, and prospective studies have demonstrated that the use of antimetabolites improves trabeculectomy survival outcomes. Studies of both the XEN Gel Stent and Preserflo devices that drain into the subconjunctival space have also demonstrated the need to apply antimetabolites to prevent fibrosis and sustain the presence of the postoperative bleb. The use of MMC using the Moorfields technique dramatically increased the success rate without any increase in complications. The augmentation of tube surgery (e.g., Baerveldt, Ahmed, and Paul tubes) is less clear because most trials did not incorporate MMC use in their design. Modulation of the healing response in both the short and long term, together with meticulous surgical techniques, may enable the surgeon to set IOP at the lowest level while avoiding the complications that can be associated with antimetabolites.
The conjunctival healing response, the phases of the response, and the greater understanding of the multiple mechanisms involved continue to inform the treatment options. These therapeutic options and modes of delivery are further discussed later.
The majority of attention has been focused on antimetabolites, such as 5-fluorouracil (5-FU) and MMC. However, other strategies exist to prevent fibrosis and scarring after glaucoma filtration surgery (summarized in Table 10.28.1 ). Many of the agents listed in Table 10.28.1 have multiple actions on the healing cascade. Other agents, such as corticosteroids, are used as adjuncts to antimetabolites and are typically used over a longer period. Intraoperative beta irradiation (750–1000 cGy) by a strontium-90 probe has similar effects to antimetabolites or at the higher dose even stronger. A randomized trial of 320 patients with open-angle glaucoma, who were of black African descent, found the estimated risk of failure of trabeculectomy at 1 year to be 5% in the irradiated arm compared with 30% in the placebo group. The incidence of cataract at 2 years in the irradiated arm, however, was significantly greater. Combining MMC and beta irradiation has a synergistic effect and achieved lower postoperative IOP in one study, and a randomized trial showed that beta radiation 10 Gy was 5.5 times more likely to achieve an IOP <16 mm Hg off medication than MMC. More recently, several antagonists to growth factors are being tested in clinical practice. The antifibrotic agents currently used most commonly are discussed in this chapter.
| Event | Potential Modulation |
|---|---|
| Previously damaged conjunctiva | Stop medical therapy, especially those causing very red eye, if possible |
| “Preactivated” cells | Preoperative corticosteroids for 1–2 weeks (may not be possible if pressure responder) |
|
|
| Release of plasma proteins and blood cells |
|
|
Agents preventing/removing fibrin—e.g., heparin, tissue plasminogen activator (although breakdown products may be fibrogenic) |
|
Blood–aqueous barrier stabilizing agents (e.g., corticosteroids) |
| Release of growth factors into aqueous |
|
| Aqueous begins to flow through wound | |
| Migration and proliferation of polymorphonuclear neutrophil cells, macrophages, and lymphocytes |
|
| Antimetabolites (e.g., 5-FU/MMC) | |
| Activation, migration, and proliferation of fibroblasts |
|
| Wound contraction |
|
| Fibroblast synthesis of tropocollagen | MMC, 5-FU, IFN-α |
| Glycosaminoglycans and fibronectin | MMC, 5-FU, MMP inhibitors |
| Collagen cross-linking and modification | Anti–cross-linking agents (e.g., β-aminopropionitrile/penicillamine) |
| Blood vessel endothelial migration and proliferation and blood vessel leakage | Inhibitors of angiogenesis and blood vessel leakage (e.g., bevacizumab and ranibizumab, angiostatin) |
| Resolution of healing | MMC, 5-FU |
| Apoptosis | Death receptor ligands |
| Disappearance of fibroblasts | Stimulants of apoptosis pathways |
| Fibrous subconjunctival scar | |
|
Pirfenidone in idiopathic pulmonary fibrosis |
Certain patient characteristics increase the risk of scarring and failure after glaucoma surgery, as summarized in Table 10.28.2 . However, the risk may still vary within subgroups. More than one risk factor, although each may be categorized as low risk individually, overall may result in placing the patient in a higher risk category. Furthermore, there may be hidden risk factors for failure in what were previously regarded as low-risk “first-time surgery” groups. There are recognized changes after chronic topical treatment. Fibroblasts appear to be activated in Tenon's capsule in patients with open-angle glaucoma. The extent to which topical treatment might affect patient outcomes after surgery is not fully understood, but there appears to be a clearer correlation with inflammation and fibrotic failure. The use of antifibrotic agents after tube drainage surgery has not been conclusively proven, and studies on the use of antifibrotics with newer surgical devices are still ongoing.
| Risk Factors | Risk (+ to +++) | Comments |
|---|---|---|
| Ocular | ||
| Neovascular glaucoma (active) | +++ | May require panretinal photocoagulation ± anti-VEGF |
| Previous failed filtration surgery | ++ (+) | Consider tube surgery |
| Previous conjunctival surgery | ++ | Uncertain |
| Chronic conjunctival inflammation | ++ (+) | |
| Previous cataract extraction (conjunctival incision) | ++ (+) | Particularly surgery within last 3 months |
| Aphakia (intracapsular extraction) | +++ | |
| Previous intraocular surgery | ++ | Depends on type of surgery and particularly with conjunctival opening, e.g., Vitreo-retinal surgery |
| Uveitis (active, persistent) | ++ | |
| A red, injected eye | ++ (+) | The more vasodilated (red eye) the worse the prognosis. On Moorfields bleb grading the highest grade of redness over 6 weeks postoperative follow-up increases the risk of failure 600% versus minimally infected eye |
|
|
Particularly if they cause a red eye |
| High preoperative intraocular pressure (higher with each 10-mm Hg rise) | + (+) | |
|
+++ (+) | |
| Inferiorly located trabeculectomy | + | Increased risk of endophthalmitis |
| Patient | ||
| African-Caribbean descent | ++ | |
| West African descent | ++ (+) | |
| East African descent | + | |
| Indian subcontinent descent | + | |
| Hispanic descent | (+) | |
| Japanese descent | (+) | |
| Older adult (>60 years) | (+) | |
| Adolescent/younger adult (16–40 years) | + (+) | |
| Children (<16 years) | ++ | |
Patient characteristics associated with a high risk of surgical failure include previous failed trabeculectomies, previous cataract surgery through a conjunctival incision, neovascular glaucoma, inflammatory eye disease, aphakia, neovascular glaucoma, black African ancestry, recent intraocular surgery, young age, and chronic topical medication. Most glaucoma specialists agree that patients with any of these should have higher concentrations of antimetabolite treatment.
The most definitive study of 5-FU injections in high-risk patients was the randomized, prospective National Eye Institute 5-Fluorouracil Filtration Surgery Study, which showed a 51% failure rate after filtration surgery in patients with previous unsuccessful trabeculectomy or in those who had undergone cataract surgery with a conjunctival incision. In the group who received 5 mg 5-FU injections (twice a day for days 1–7, once a day for days 8–14, a total 21 injections), the failure rate was 51% compared with 74% in the placebo group after 5 years. Since then, randomized studies undertaken to compare intraoperative MMC application (0.4–0.5 mg/mL) with 5-FU injections have suggested that in high-risk patients, a single application of MMC provides superior long-term pressure control compared with injections of 5-FU without the risk of keratopathy. Corneal epithelial complications are much more common with injectable 5-FU, but both groups had thin avascular blebs, these being more prominent in the MMC-treated groups. A comparative 3-year study of West African patients found fewer postoperative hypotensive medications were required for the MMC-treated group (0.5 mg/mL for 3 minutes) compared with those who received 5-FU application (50 mg/mL for 5 minutes), although with a total of 68 patients, a statistical difference in success was not reached.
Using a single intraoperative 5-FU application, Egbert et al. carried out a randomized prospective study in a group of West African patients who had a high risk of failure. They showed success rates of 83% in the 5-FU-treated group versus 39% in the control group, with a mean follow-up of 282 days.
The intraoperative MMC regimen, rather than postoperative subconjunctival 5-FU injections, has become the treatment of choice for all patients, and higher concentrations (≥0.4 mg/mL) are considered for high-risk patients. There is increased efficacy, ease of application, and virtual absence of corneal side effects. However, longer periods of follow-up are needed to monitor and determine the development of bleb leaks, hypotony, and endophthalmitis, in view of the thinner and highly avascular blebs sometimes seen with MMC. The incidence of these so-called high-risk blebs has been dramatically reduced, however, because of the introduction of a theory of cystic bleb formation that changed the method of antimetabolite application during glaucoma surgery. Systemic corticosteroids and immunosuppressants are used in particular high-risk groups but are not routine and can have severe side effects if used by an inexperienced physician. The introduction of anti–vascular endothelial growth factor (anti-VEGF) treatment to augment incisional surgery has gained popularity. Although it is unlikely that anti-VEGF agents are as effective in preventing fibrosis after trabeculectomy as MMC, there is evidence that in combination with MMC, low IOP targets are more likely to be achieved. Better bleb morphology and a reduction in bleb vascularization have been observed after intravitreal ranibizumab in combination with intraoperative topical MMC. Subconjunctival bevacizumab has also been used successfully to rescue failing filtering blebs that exhibit neovascularization.
In patients with no previous ocular surgery and no significant comorbidity apart from glaucoma, the use of antimetabolites is more controversial. Intraoperative MMC application not only increases the success rate of surgery but also increases the incidence of hypotony, particularly when more stringent surgical measures are not taken to prevent hypotony. Bindlish et al. reported an incidence of late hypotony (IOP <6 mm Hg) in 42% of eyes at some point between 6 months and final follow-up at 5 years, in a series of 123 primary trabeculectomies with MMC. Hypotony occurs more in younger patients, particularly those who have myopia with thin sclera, probably because the sclera is too thin for the scleral flap to achieve an adequate resistance to outflow. Recent surveys of both US and UK glaucoma specialists confirm that the application of MMC is now routine for most subconjunctival incisional surgery with the exception of tube surgery devices.
5-FU injections have been used in lower-risk groups, which include those who have undergone first-time filtration surgery, young patients, and those with normal-tension glaucoma, to achieve lower IOPs and superior success rates. Complications, such as corneal epithelial changes, are more common but generally only in the short term. Cell culture experiments suggest that a single 5-minute application of 5-FU is able to inhibit fibroblasts for several weeks without severe long-term damage and be equivalent to low-dose 5-FU injections. Several studies using single applications of intraoperative 5-FU with short-term follow-up have reported promising results in low-risk patients. Lanigan et al. reported a success rate of 77% in high-risk patients (those with neovascularization, previous failed filtration surgery, aphakia, uveitis, or multiple risk factors), with a 100% success rate in the low-risk groups. Feldman et al. reported an overall success rate of 85% in high-risk patients and a success rate of 92.9% in low-risk patients; no hypotony was seen in the Feldman study. However, both studies were of short duration and had no controls. Therefore failure occurs in higher-risk patients who have a prolonged or aggressive healing response, but in lower-risk patients the success rate is very good (>90%) with no clinically significant hypotony. An improvement in survival was also found for patients in East Africa with a single 5-minute application of low-dose 5-FU (25 mg/mL), interestingly with a much lower failure rate in the control group compared with patients in West Africa. There is evidence that 5-FU trabeculectomy maintains IOP in the low teens compared with nonaugmented surgery.
Comparative studies for primary trabeculectomy have not found one antimetabolite to be clearly superior to another. A trial of 5-FU 50 mg/mL versus MMC 0.2 mg/mL in first-time trabeculectomy (low risk) in the United States did not show any statistically significant differences, to date, in efficacy or side effects of 115 eyes randomized to receive either treatment. These findings were similar to those of WuDunn et al., who used the same doses of 5-FU and MMC. However, the lack of significant differences may be in part because of the postoperative manipulation of the bleb emphasizing the importance of postoperative management.
A single antimetabolite regimen may not be adequate for all patients. The type and dose of drug need to be titrated depending on the individual patient's risk factors and healing response. The authors use a “titratable” regimen that is based on laboratory and clinical data gained from experience using the different single-application agents and concentrations (the authors call this the Moorfields/Florida regimen [“More Flow regimen”]). This regimen evolves constantly, but the present one is summarized in Box 10.28.1 . Postoperative subconjunctival injections of anesthetic/corticosteroid/anti-VEGF agents at the time of surgery and in the clinic with the addition of 5-FU may be used in addition to the application of intraoperative antimetabolites.
No risk factors
Short-term topical medication
Very old adults with thin conjunctiva
Chronic topical medications or others that cause a red eye
Previous cataract surgery without conjunctival incision (capsule intact)
Several low-risk factors
Combined glaucoma filtration surgery/cataract extraction
Previous conjunctival surgery (e.g., squint/detachment surgery)
East African ancestry
Neovascular glaucoma (combine with bevacizumab)
Chronic persistent uveitis (antiinflammatory/immunosuppression)
Previous failed trabeculectomy/tubes with or without antimetabolites
Chronic conjunctival inflammation
Cicatricial conjunctival disease
Multiple risk factors
Aphakic glaucoma (a tube with antimetabolites may be more appropriate in many of these cases)
West African ancestry
An intraoperative, single-dose regimen for scarring after glaucoma filtration surgery. (This regimen is still evolving.) Other factors may also determine the choice of agent, such as the need for a low target pressure resulting from advanced disease (require a stronger antimetabolite treatment). Beta radiation 10 Gy can also be used.
Postoperative 5-FU injections can be given in addition to the intraoperative applications of antimetabolite.
5-FU , 5-Fluorouracil; MMC , mitomycin C.
There are great variations in the technique used to administer intraoperative antimetabolites, which may account for some of the published variations in efficacy and complications. It is important for individual surgeons to maintain a consistent technique and to periodically reevaluate their experience in the use of this technique. Intraoperative MMC applications are commonly used, but preoperative MMC injections are also now used before glaucoma filtration surgery. It is now better understood how antimetabolites, particularly MMC, work in vivo, causing long-term tissue cell death and growth arrest. There is remnant functional activity in peripheral fibroblasts, which form a ring of scar tissue around the bleb (“ring of steel”). This has allowed the development of strategies in antimetabolite delivery and associated surgical techniques, which increase safety and improve bleb appearance dramatically ( Fig. 10.28.1 ). Optimization of the application technique has been and is important for refinement and long-term IOP control of MIGS devices that drain into the subconjunctival space. In particular, it has been important for the development of the Preserflo (formerly InnFocus implant), where our technique of MMC facilitated the use of MMC with this implant, without which the success rate was much lower. Also critical is the “R1R2” principle, where R1 is the outflow resistance due to the device and R2 is the outflow resistance caused by the bleb, with the addition of the two determining the final IOP.
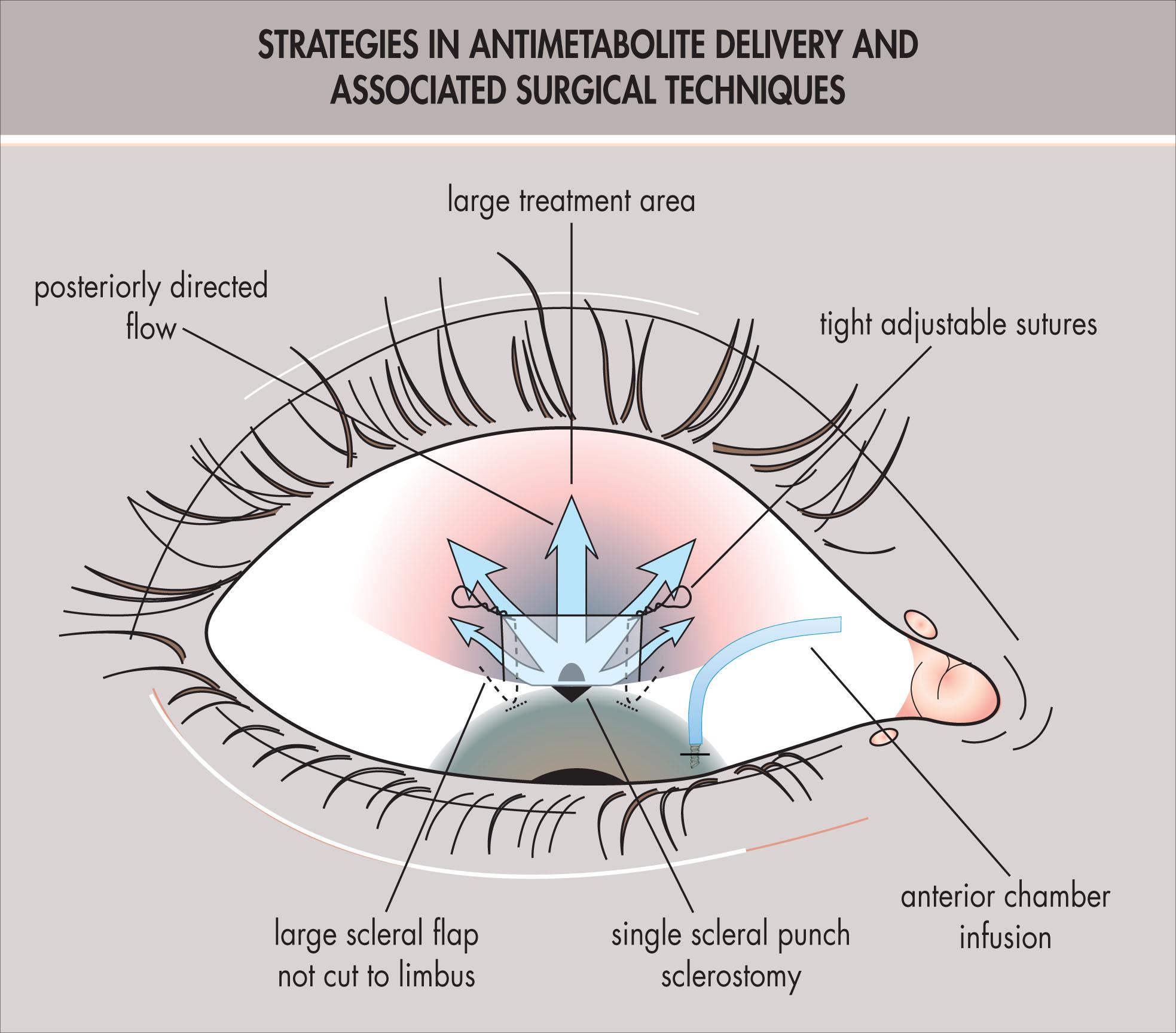
This change has led to a reduction in the number of cystic blebs from 90% to 29% and has reduced bleb-related complications, particularly endophthalmitis, from 15% to 0% over a 3-year follow-up period ( Fig. 10.28.2 ). More recent reports of this safer trabeculectomy technique have recorded a success rate of 96.7% (IOP <21 mm Hg) at 3 years in a complex case mix, and Stalmans et al. reported a success rate of 100% (IOP <21 mm Hg) in lower-risk patients at 15.7 months mean follow-up with few complications (flat anterior chamber 1.8%; hypotony beyond 3 weeks 1.5%). Simple adjustments of technique should result in much lower complication rates for many thousands of patients (summarized in Box 10.28.2 ).
![Fig. 10.28.2, Focal cystic bleb prone to leakage, infection, and dysesthesia in the left eye (limbus-based conjunctival flap, small scleral flap, and smaller area of mitomycin C [MMC] 0.4 mg/mL treatment). Diffuse noncystic bleb appearance in right eye of the same patient (fornix-based flap, larger scleral flap, and larger area of MMC 0.5 mg/mL treatment). Fig. 10.28.2, Focal cystic bleb prone to leakage, infection, and dysesthesia in the left eye (limbus-based conjunctival flap, small scleral flap, and smaller area of mitomycin C [MMC] 0.4 mg/mL treatment). Diffuse noncystic bleb appearance in right eye of the same patient (fornix-based flap, larger scleral flap, and larger area of MMC 0.5 mg/mL treatment).](https://storage.googleapis.com/dl.dentistrykey.com/clinical/AntifibroticAgentsinGlaucomaSurgery/1_3s20B9780323795159001997.jpg)
Use of weaker agents (intraoperative 5-fluorouracil), lower concentrations of mitomycin C for lower-risk individuals or individual at high risk of hypotony or other complications of antimetabolites
Nonfragmenting sponges (polyvinyl alcohol rather than methylcellulose)
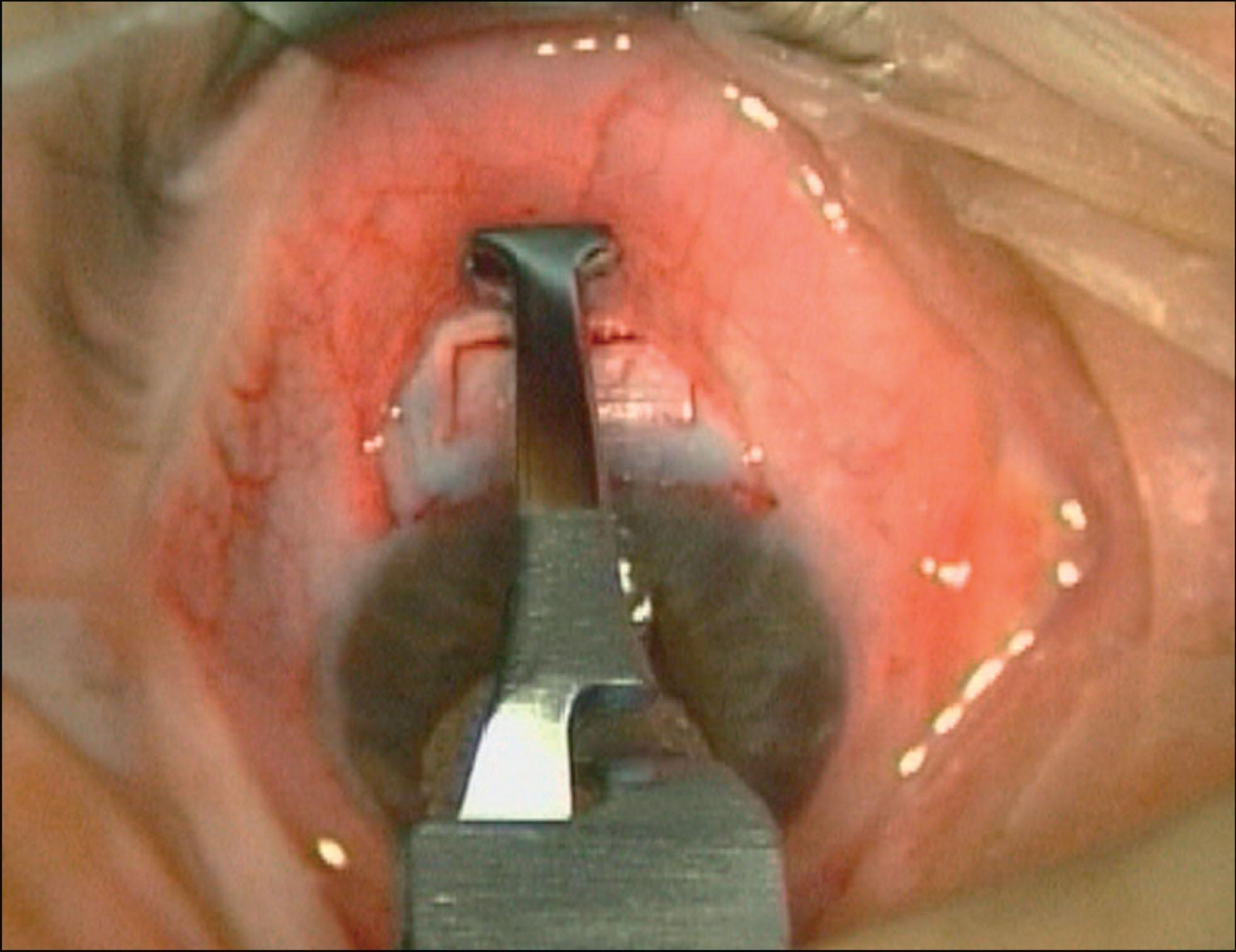
Protection of cut edge with special clamp (John Weiss or Duckworth & Kent, Baldock, UK) to prevent dehiscence
Treatment under both scleral flap and conjunctival flap; the use of the sponge both under the scleral flap and the conjunctiva does seem to enhance the success rate
Measures to secure scleral flap—smaller sclerostomy, larger scleral flaps, multiple tight sutures that are both adjustable (adjustable suture control) and releasable
Intraoperative flow control—continuous positive pressure infusion giving accurate indication of flow, maintaining blood–aqueous barrier, and washing out cytokines
Measures to produce diffuse noncystic blebs—large scleral flaps, fornix-based conjunctival flap, or extremely posterior limbus-based incision and large surface area of antimetabolite treatment; b ig (treatment area, scleral flap) and b ackward (aqueous flow direction) is b etter for b lebs
The optimal concentration of intraoperative MMC has not been established. Chen et al. reported results in high-risk patients since 1981 without failures, but a 66% rate of hypotony with MMC 0.4 mg/mL, a 22% failure rate with no hypotony with MMC 0.2 mg/mL, and a 37% failure rate with no hypotony with MMC 0.1 mg/mL. In a randomized, prospective study of Japanese patients given primary surgery, Kitazawa et al. had a 100% success rate with MMC 0.2 mg/mL (but transient hypotony maculopathy and cataract progression in 18%) and a 64% success rate with MMC 0.02 mg/mL with no hypotony or cataract progression. For intraoperative 5-FU, both 50 mg/mL and the weaker 25 mg/mL have been used, but no direct comparison has been made between the two.
The optimal time of exposure also has not been determined. Megevand et al. retrospectively compared eyes treated with MMC 0.2 mg/mL for 2 or 5 minutes. There was no statistically significant difference in success rate or complications, but hypotony and endophthalmitis still occurred. In another study, MMC was administered intraoperatively at 0.5 mg/mL for 5 minutes or 0.4 mg/mL for 3 minutes in Indian patients. No significant difference occurred in postoperative IOP, hypotony, or postoperative filtration failure rate. However, the group treated with the higher concentration for 5 minutes had a higher incidence of serous choroidal detachment. One patient from each group developed postoperative endophthalmitis during the study period. Shorter applications of 2–3 minutes, compared with 5 minutes, appear to have the same efficacy, but if applications are shortened to less than 2 minutes, suboptimal cellular and tissue absorption may occur. In a study of 5-FU uptake in tissues, the concentrations reached a plateau at 3 minutes. Even shorter application times may result in greater variations in drug delivery.
Changes in the concentration of the agent are more likely to give reproducibly titratable effects compared with variations in exposure time. Therefore to achieve consistent and predictable results, it is probably more important that the individual surgeon becomes accustomed to one or two concentrations and one exposure time. We use MMC 0.2 or 0.5 mg/mL for 3 minutes on the basis of our previous studies.
Small variations in technique may have profound effects on the clinical result and complications. The type of sponge may significantly affect the amount of drug delivered. Chen et al. originally used a Gelfoam sponge, but most clinicians use commercially available sponges (e.g., Weck cell, Merocel), which have different retention and drug-releasing capabilities and may be cut to different sizes. Attempts to standardize the dose of drug delivered have been made, and the accurate application of MMC drops to a standard sponge will deliver a known dose. We currently use polyvinyl alcohol sponges (Merocel, Mystic, CT, USA) because these do not disintegrate like methylcellulose and leave fragments in the wound that can cause significant foreign body granulomas. A MMC formulation kit licensed by the US Food and Drug Administration is now available (Mobius Therapeutics, St. Louis, MO, USA).
On the basis of clinical observation, a hypothesis as to why cystic blebs occur has been put forward ( Fig. 10.28.3 ). By treating larger areas, bleb-related complications can be reduced. This clinical finding has been confirmed experimentally. A specially designed clamp (2-686; Duckworth & Kent, Baldock, UK) for use during either limbal or fornix-based surgery helps protect the conjunctival edge from exposure ( Fig. 10.28.4 ).
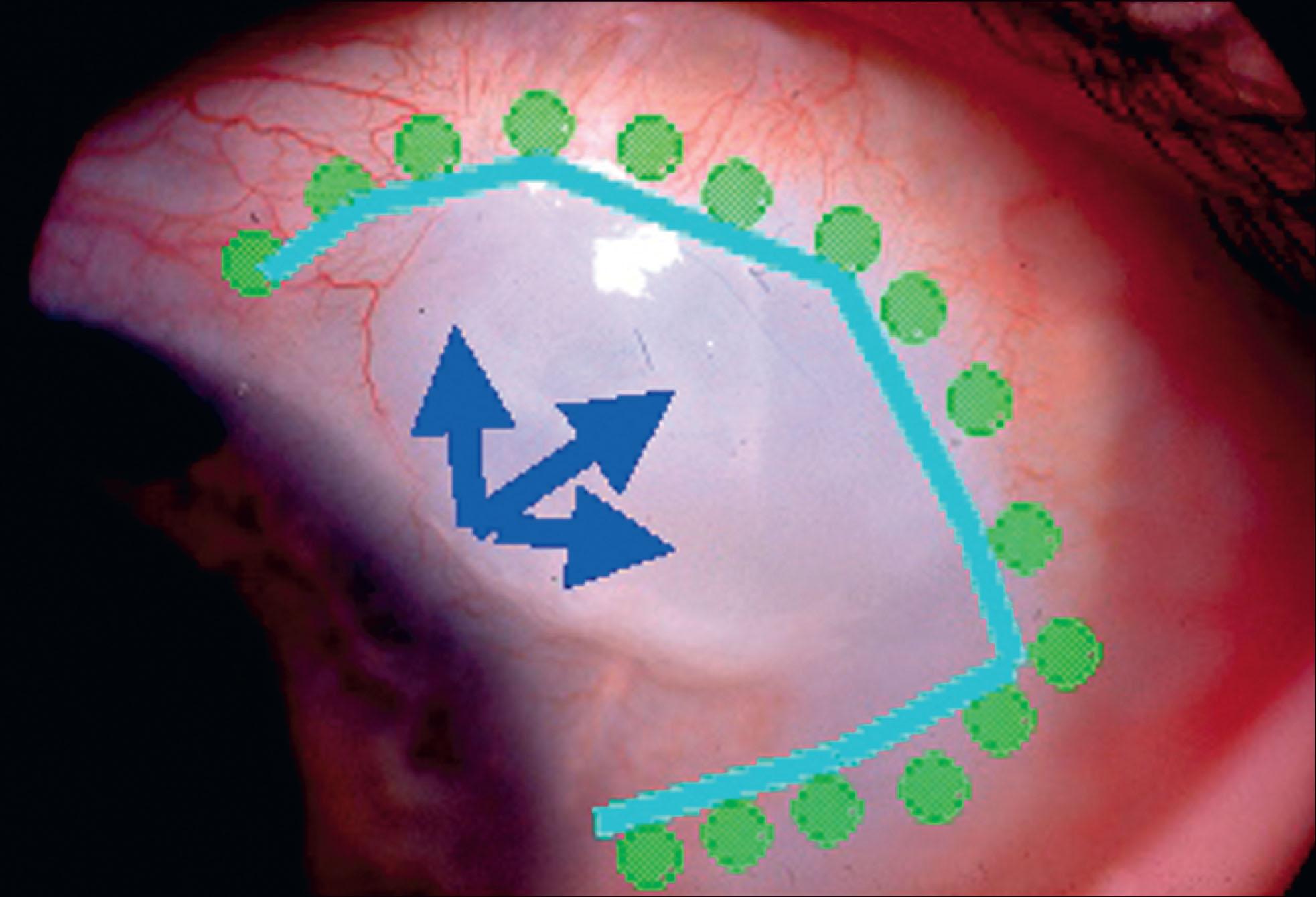
Treatment under both the scleral flap and conjunctival flap, particularly in high-risk cases, can be considered. Finally, staining of the antimetabolites with trypan blue has been described permitting the delineation of the treatment area. This principle has been adopted very successfully for current devices with good success rates and diffuse noncystic blebs.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here