Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Determine factors that caused the prior ACL reconstruction to fail
Address all pathologies before surgery: lower limb malalignment, muscle atrophy, limitation knee motion, gait abnormalities, misplaced tunnels.
Goals, outcome of surgery depend on preexisting joint damage, associated procedures required.
Knees with misplaced tunnels with intact menisci and articular cartilage: most ideal outcome expected.
Knees with prior meniscectomy, articular cartilage damage, other ligament insufficiency, or varus malalignment: salvage procedure.
Select cases with concomitant articular cartilage restoration procedure, meniscus transplantation
Many factors influence failure of anterior cruciate ligament (ACL) surgery. A failed ACL reconstruction is noted by a return of knee instability and increased lateral and medial tibiofemoral compartment anterior translation and subluxation as demonstrated by positive Lachman and pivot shift tests. The surgeon must determine the factors that caused the prior reconstruction to fail, which may include a misplaced vertical ACL graft, inadequate healing and maturation of the graft, associated lateral or medial ligament insufficiency, varus or valgus malalignment, or inadequate postoperative rehabilitation with residual weakness and neuromuscular control ( Table 8-1 ). In many cases, other associated major knee problems are present. These include limitation of knee motion with pain and stiffness, muscle atrophy from inadequate rehabilitation, articular cartilage damage, meniscectomy and its effects on joint symptoms and function, undiagnosed lower limb malalignment, and posterolateral (PL) or medial ligament deficiency. When present, each of these pathologies must be addressed and resolved before or during ACL revision. The goal of rehabilitation is to restore the best possible function to the lower extremity before ACL revision to minimize the possibility of failure of the revision procedure.
|
Importantly, the patient and surgeon must address the expectations and goals of the revision because often associated cartilage damage or meniscectomy requires modification or elimination of strenuous, high-impact activities. In many cases, patients have undergone multiple prior surgical procedures that did not achieve the desired outcome. The expectation of the revision operation to accomplish the patient's goals must be realistically discussed.
A number of preoperative and operative issues must be addressed in a methodical manner to salvage knee function and obtain a reasonable result after prior ACL procedures have failed. These may include the necessity to perform staged procedures to correct lower limb malalignment with an osteotomy or fill enlarged or misplaced tibial and femoral tunnels with a bone graft. Patients may require extensive rehabilitation before surgery to restore normal joint motion and neuromuscular control. The approach taken is to maximize every aspect of the patient's knee condition and not accept any abnormality, such as a slightly misplaced tunnel or concurrent knee instability, in planning the revision procedure.
Other chapters in this book address issues related to correction of lower limb malalignment, arthrofibrosis, and muscle atrophy; procedures for articular cartilage defects; meniscus transplantation; and PL and medial ligament reconstructions. Although the timing of these procedures will be addressed in this chapter, the principal focus relates to surgical planning and technique decisions that, in our experience, will improve the success of the ACL revision.
Patients presenting for ACL revision fall into one of three categories, each of which has a different prognosis. In the most ideal category are knees with a misplaced tibial or femoral tunnel that have intact menisci and articular cartilage and no associated ligament instability. In these cases, the revision procedure is similar to a primary ACL reconstruction in terms of an expected good functional outcome. In the most severe category are knees that had a previous meniscectomy, articular cartilage damage, associated ligament instabilities, or lower limb malalignment. These patients will have a less than ideal outcome and the revision represents a salvage situation. In the middle of these two categories are patients who have partial or complete loss of meniscus function, associated cartilage damage, and a residual pivot shift from a failed ACL procedure, but no associated lower limb malalignment or other ligament instability. The outcome for providing stability in these cases is good; however, further joint deterioration will occur over time and counseling must be undertaken for activity modification. In select cases, indications exist for an articular cartilage restoration procedure and meniscus transplantation. Clinical studies on ACL revision usually contain a selection bias regarding the inclusion of patients from these three categories, which accounts for the differences in reported outcomes among investigations. The majority of studies report that the outcome of ACL revision is inferior to that of primary reconstruction. Usually, the revision procedures are performed many months or years after the failure of the primary reconstruction, during which time further giving-way episodes and joint deterioration have occurred that compromise the final outcome.
A frequent clinical presentation after an ACL reconstruction with a vertical ACL graft is a negative or mildly positive Lachman test with a positive pivot shift test that reproduces the patient's complaints of residual giving-way with activities. These patients are candidates for an ACL revision in which the entire ACL graft is removed and an anatomic ACL graft replacement is performed. In rare instances, the primary ACL graft may be retained and a second graft is placed in a more suitable anatomic location to provide rotational stability, as is discussed later.
Sedentary patient with no symptoms with daily activities.
Patient willing to modify activity level, avoid high-risk knee motions.
Patient not able to participate or comply with rehabilitation program.
Presence of symptomatic arthritis in knees with major loss of joint space.
Varus-malaligned knees undergo high tibial osteotomy first, may not require subsequent ACL revision.
Patients with marked muscle atrophy undergo extensive rehabilitation first, restoration of muscle function may avoid ACL revision.
Complex regional pain syndrome.
Unrealistic expectations for future athletic activities.
Obesity, prior joint infection.
Patients who are sedentary and do not experience giving-way or swelling episodes with daily activities and have little exposure to strenuous or high-risk activities are treated conservatively. These patients are advised to maintain an ideal body weight and have periodic knee examinations. In addition, patients who are willing to modify their activity level to avoid high-risk knee motions such as pivoting and cutting are placed into a conservative treatment program. Patients who are unable to participate or be compliant with postoperative rehabilitation are not surgical candidates.
The presence of symptomatic patellofemoral or tibiofemoral arthritis is a general contraindication to ACL surgery, because pain symptoms remain postoperatively. Although pain symptoms may be lessened by restoring knee stability, significant joint damage may still limit daily activities. Weight-bearing 45-degree posteroanterior (PA) views are important to determine the millimeters of remaining medial or lateral tibiofemoral joint space. Patients are frequently surprised to learn that the joint space is absent or nearly absent because their symptoms have not yet limited daily activities. In these knees, conservative measures are instituted until such time that unicompartmental or total joint replacement is warranted.
Patients with ACL deficiency, symptomatic medial tibiofemoral arthritis, and varus malalignment require corrective valgus-producing high tibial osteotomy (HTO). These patients often do not require subsequent ACL surgery, because there are limitations in activities owing to the joint damage. These patients often report improved joint instability because the varus thrust gait pattern is eliminated with osteotomy.
Patients with marked lower extremity muscle atrophy often require a delay in surgery for many months until adequate muscle function has been restored. These patients have an increased risk for postoperative complications, including quadriceps muscle shutdown, patella infera, and arthrofibrosis. In some cases, the restoration of muscle function may lead to increased knee stability, avoiding ACL revision.
The presence of residual signs and symptoms of a complex regional pain syndrome (CRPS) requires careful examination and questioning regarding the presence of burning pain, abnormal skin hypersensitivity, extremity discoloration, and intolerance to cold and ice. Even after resolution of a prior CRPS, there is an increased frequency for return of the syndrome in these knees that must be promptly recognized in the postoperative period (see Chapter 40 ).
It is not unusual for patients who require ACL revision to have unrealistic expectations of future athletic activities. The goals of the revision procedure are reviewed in detail, and the patient educational process involves recommendation of recreational and low-impact activities only, avoiding strenuous activities in knees with associated joint cartilage damage.
Patients with a body mass index of 30 or greater are usually not surgical candidates. A history of prior infection with subsequent joint arthritis often contraindicates ACL revision. There may be associated medical conditions contraindicating surgery. The use of nicotine products is strongly discouraged and absolutely contraindicated if osteotomy alignment procedures are required.
Perform thorough history, review prior medical and operative records.
Comprehensive physical examination assesses knee flexion and extension, patellofemoral indices, tibiofemoral crepitus, tibiofemoral joint line pain, muscle strength, gait abnormalities.
Perform all stability tests to document abnormal tibial translation, rotations, and tibiofemoral compartment translation.
Knee arthrometer test: 134 N.
Radiographs: standing anteroposterior at 0 degree, lateral at 30 degrees; weight-bearing PA at 45 degrees; patellofemoral axial views; double-stance hip-knee-ankle alignment; lateral and posterior stress views as indicated.
MRI, including articular cartilage image techniques.
Cincinnati Knee Rating System for subjective, objective, functional scoring.
A thorough history is performed, including a detailed account of all knee injuries and the operative procedures that have been performed. In revision knees, prior operative records are obtained to verify the surgical findings, condition of the articular cartilage and menisci, and graft placement. A comprehensive physical examination is performed, including assessment of knee flexion and extension, patellofemoral indices, tibiofemoral crepitus, tibiofemoral joint line pain, muscle strength, and gait abnormalities. The surgeon must determine all of the abnormal translations and rotations in the knee joint. The medial posterior tibiofemoral step-off on the posterior drawer test is done at 90 degrees of flexion. Quantification of posterior tibial translation may be performed using stress radiography in knees with posterior cruciate ligament (PCL) ruptures to determine if the rupture is partial or complete (see Chapter 16 ). The appropriate tests to determine the integrity of the ACL are performed, including KT-2000 (MEDmetric) arthrometer testing at 20 degrees of flexion (134-N force) to quantify total anteroposterior (AP) displacement. The pivot shift test is recorded on a scale of 0 to III, with a grade of 0 indicating no pivot shift; grade I, a slip or glide; grade II, a jerk with gross subluxation or clunk; and grade III, gross subluxation with impingement of the posterior aspect of the lateral side of the tibial plateau against the femoral condyle.
Insufficiency of the PL and medial ligament structures are determined by varus and valgus stress testing at 0 and 30 degrees of knee flexion. The surgeon estimates the amount of joint opening (in millimeters) between the initial closed contact position of each tibiofemoral compartment, performed in a constrained manner avoiding internal or external tibial rotation, to the maximal opened position. The result is recorded according to the approximate millimeters of increase in the tibiofemoral compartment opening of the affected knee compared with that of the opposite normal knee. Abnormal medial or lateral joint opening may be measured with stress radiographs. The results are always confirmed at arthroscopy by the gap test. The tibiofemoral rotation dial test at 30 and 90 degrees detects increases in external tibial rotation with posterior subluxation of the lateral tibial plateau or anterior subluxation of the medial tibial plateau caused by medial ligament injury. A word of caution is necessary, because it is possible to confuse increased external tibial rotation for a PL injury and miss the medial side ligament injury that requires correction. The presence of a varus recurvatum in both the supine and standing positions is carefully assessed. Gait analysis is performed to detect a varus or valgus thrust or hyperextension thrust. Patients can often demonstrate their knee instability on standing, with a few degrees of knee flexion, by producing an external femoral rotation that reproduces the pivot shift phenomena. Abnormal varus or valgus tibiofemoral joint opening may also be demonstrated by the patient.
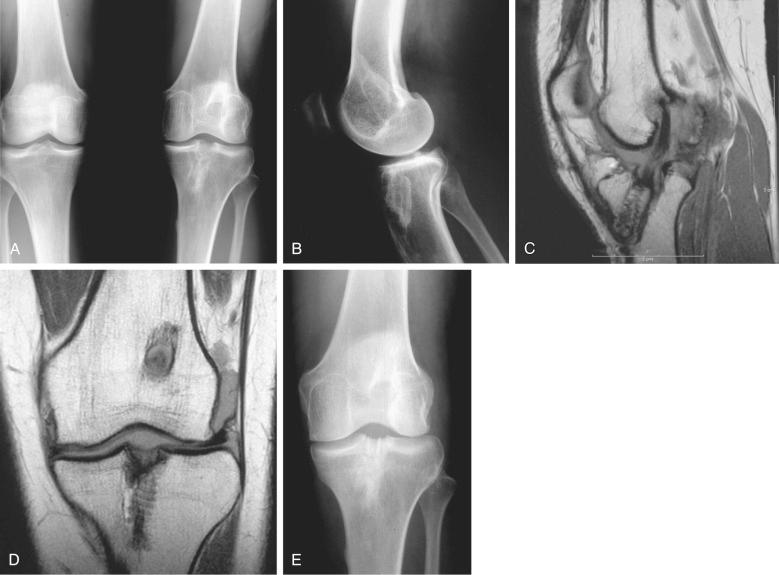
Radiographs taken during the initial examination include standing AP at 0 degree, lateral at 30 degrees of knee flexion, weight-bearing PA at 45 degrees of knee flexion, and patellofemoral axial views. Double-stance full-standing radiographs of both lower extremities, from the femoral heads to the ankle joints, are obtained in knees in which varus or valgus lower extremity alignment is detected on clinical examination. The mechanical axis and weight-bearing line are measured as discussed in Chapter 26 . Magnetic resonance imaging (MRI) is performed to provide further details of tunnel placement and the condition of the articular cartilage and menisci. Fast-spin-echo and other MRI protocols (T2 mapping) are available to obtain superior quality articular cartilage images. The tibial tunnel placement is visualized on sagittal views and measurements made to determine if the tunnel is too posterior, which often requires a staged bone graft procedure.
At our center, patients complete questionnaires and are interviewed for the assessment of symptoms, functional limitations, sports and occupational activity levels, and patient perception of the overall knee condition according to the Cincinnati Knee Rating System (CKRS; see Chapter 41 ). The forms are available online for the patient to obtain before their consultation.
Determine all factors related to failure index ACL procedure for treatment plan.
Identify tibial and femoral tunnel location and necessity for bone graft.
Identify hardware previously used.
Obtain full knee motion, muscle strength, return of adequate neuromuscular function.
Determine need for concomitant cartilage/meniscus procedures, extraarticular procedures, and other ligament reconstructions to correct all instabilities.
Address patient expectation and goals of surgery.
The factors that may have been related to or directly caused the failure of the prior ACL reconstruction must be identified and addressed either before or during the revision procedure. A meticulous physical examination, previously discussed, is performed to detect associated ligament deficiencies, valgus or varus lower limb malalignment, or gait abnormalities. The type of hardware used previously is identified to ensure that the proper equipment is available for removal during the revision procedure, if required. If existing hardware does not interfere with new tunnel placement and is in a difficult location to reach, it may be left alone.
All abnormalities or potential problems are addressed preoperatively, including patient expectation issues, muscular weakness, painful neuromas, residual CRPS, and anterior knee pain caused by patellofemoral cartilage damage. A loss of full knee extension creates problems. It is important to obtain full knee motion before revision surgery. The exceptions are grafts placed too far anteriorly or cyclops lesions that produce a mechanical block to full extension or flexion. During the revision procedure, anterior intercondylar blockage is eliminated by adequate notchplasty and correct graft placement. In these knees, there may also be associated tightness to the posterior capsular structures, which have shortened, requiring a vigorous postoperative program. If the lack of extension is greater than 5 degrees, the procedures are staged by first performing an arthroscopic debridement and cyclops lesion excision, followed by rigorous rehabilitation to regain full motion, and then ACL revision reconstruction.
Knees with grossly positive clinical laxity tests have involvement of the secondary ligament restraints, primarily the PL structures. Associated medial or lateral ligament laxity is an indication for medial or lateral ligament reconstruction.
Considerable counseling and patient education are required on the expected results and outcomes from the revision procedure. This is especially important in knees with preexisting arthritis or loss of meniscal function or those that require additional major operative procedures. In nearly one half of revision knees, a major concomitant procedure will be required. Patients need to understand the technical difficulties inherent in the operative procedures and that the results are typically not as favorable as primary ACL reconstruction. A surgeon-rehabilitation team is required to provide instruction on rehabilitation to ensure that the postoperative exercise program will be successfully followed by the patient.
We prefer B-PT-B autograft; use contralateral knee if previously harvested.
QT-PB autograft second option.
STG autograft (four- or six-strand) option for recreational athletes, more sedentary patients.
B-PT-B or Achilles tendon-bone allograft reserved for multiligament procedures, special cases where graft harvest to be avoided, or patient refuses contralateral autograft harvest.
Graft harvest: See Chapter 7 .
Currently, there is no standard graft choice for ACL revision reconstruction. Autograft tissue sources include bone-patellar tendon-bone (B-PT-B), quadriceps tendon-patellar bone (QT-PB), and semitendinosus-gracilis (STG) tendons. We prefer B-PT-B autogenous grafts. If the ipsilateral patellar tendon was previously harvested, the contralateral patellar tendon is a potential graft source. Ipsilateral patellar tendon graft reharvest is not recommended because of persistent changes on MRI and graft morphology reported in these knees 7 to 10 years postoperatively. A B-PT-B autograft is not recommended if there is associated patellofemoral arthritis (Grade 2B or 3A classification; see Chapter 44 ), anterior knee pain, or history of patellar subluxation or dislocation. A B-PT-B autograft is not performed when patient issues suggest a decreased ability to follow the more involved rehabilitation program and initial pain related to this graft.
A second option is a QT-PB graft taken from the same or opposite knee, with grafting of any residual patellar bone defect. The quadriceps tendon has the greatest cross-sectional area (100 mm 2 ) and is ideal in revision knees if the prior tunnels are in the desired anatomic ACL site, but are slightly expanded.
A third option in knees with good bone quality and normal-sized tunnels is an STG autograft, which may be either a four-strand or six-strand graft (see Chapter 7 ). In recreational athletes and more sedentary patients, a four- or six-strand STG autograft is recommended. Newer fixation methods have increased the success rate and the rehabilitation postoperatively is easier on the patient.
If autograft tissues are not available or the patient refuses a contralateral autograft harvest, then a B-PT-B or Achilles tendon-bone allograft is recommended. A lateral extraarticular iliotibial band (ITB) procedure is recommended with ACL allografts in knees that demonstrate a grade III pivot shift test or greater than 10 mm of increased AP translation on KT-2000 testing to reduce the high failure rate noted after revision ACL allograft reconstruction and the delay in allograft healing and maturation. A posterior or anterior tibialis allograft is not recommended. It is desirable to have one portion of the graft with a bone plug for increased rate of graft healing in one of the tunnels.
Patient uses chlorhexidine wash operative limb three days before surgery.
Antibiotic infusion 1 hour before surgery.
Nonsteroidal antiinflammatory medication morning of surgery, continued 5 days postoperative.
Knee to be reconstructed initialed by surgeon, time-out in operating room.
Lateral and medial gap test done during arthroscopic examination to determine need for concurrent ligament reconstructive procedures.
The patient is instructed to use a chlorhexidine wash of the operative limb (“toes to groin”) three days before surgery, including the evening before and morning of surgery. Lower extremity hair is removed by clippers, not a shaver. Antibiotic infusion is begun 1 hour before surgery. The use of a nonsteroidal antiinflammatory drug (NSAID) and a postoperative firm double-cotton, double-Ace compression dressing for 72 hours (cotton, Ace, cotton, Ace layered dressing) has proven effective in diminishing soft tissue swelling in knee surgery cases. In complex multiligament surgery, the antibiotic is repeated at 4 hours and continued for 24 hours. A urinary indwelling catheter is not used unless there are specific indications. The patient's urinary output and total fluids are carefully monitored during the procedure and in the recovery room. The knee skin area is initialized by the surgeon before entering the operating room, with a nurse observing the procedure. The identification process is repeated with all operative personnel with a “time out” before surgery to verify the knee undergoing surgery, procedure, allergies, antibiotic infusion, and special precautions that apply. All personnel provide verbal agreement.
The patient setup and positioning and graft harvest techniques for B-PT-B, STG, and QT-PB autografts are done as described in detail in Chapter 7 .
All knee ligament subluxation tests are performed after the induction of anesthesia in both the injured and contralateral limbs. The amount of increased anterior tibial translation, posterior tibial translation, lateral and medial joint opening, and external tibial rotation are documented. A thorough arthroscopic examination is conducted, noting articular cartilage surface abnormalities and the condition of the menisci. Appropriate debridement and meniscus repair or partial excision are performed as necessary.
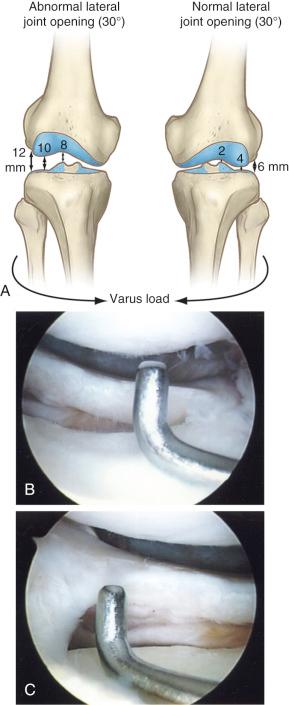
The lateral and medial gap tests are done during the arthroscopic examination (see Chapter 17 ). The knee is flexed from 25 to 30 degrees and a varus load of approximately 89 N applied. A calibrated nerve hook is used to measure the amount of tibiofemoral compartment opening ( Fig. 8-1 ). Knees that have 12 mm or more of joint opening at the periphery or 10 mm at the midpoint of the tibiofemoral compartment require a PL or medial ligament reconstructive procedure.
The general principles the senior author (F.R.N.) applies to ACL reconstruction are discussed in Chapter 7 (see Table 7-8 ).
Identify prior tibial tunnel entrance after removal of soft tissues and graft material at the ACL attachment location.
Identify lateral meniscus attachment, PCL, posterior ridge, medial tibial spine, medial articular cartilage.
Posterior expanded tibial tunnel extending all the way to the RER is not acceptable for revision graft, requires staged bone grafting with autogenous bone.
Posterior tibial tunnel located in posterior one third of the native ACL attachment, with 5-mm bridge between the tunnel and RER, if not dilated, may be relocated anteriorly.
Use cortical allograft dowel to fill posterior one third of tunnel.
Or perform double-bundle reconstruction. Posterior tibial tunnel used for PM bundle, second anterior tibial tunnel used for AM bundle when two femoral tunnels possible.
Place arthroscope in AM portal, view entire lateral notch and notch roof.
Remove all soft tissues and graft material.
Perform limited notchplasty to view furthest posterior aspect of lateral notch.
Map out central anatomic ACL; position knee 20 to 30 degrees of flexion.
Majority knees will have vertical grafts on roof of notch, allowing new lateral wall tunnel to be placed.
For dilated and slightly misplaced femoral tunnel, use two stacked interference screws to provide a buttress against one side of the tunnel. Only possible if tunnel is close to ideal anatomic position. Otherwise, staged bone graft required.
It is next important to determine that the tibial and femoral tunnels can be placed into the ideal position before the selected graft is harvested and prepared. The selection and preparation of autografts is performed only after the tibial and femoral tunnels have been determined to be adequate or have been bone grafted previously.
It is usually not difficult to identify the prior tibial tunnel entrance into the joint after removal of the soft tissues and graft material at the ACL attachment location. The adjacent lateral meniscus attachment may be encased in scar tissue and is preserved. The PCL, posterior ridge, medial tibial spine, and medial articular cartilage are all identified. The furthest extent of the posterior ACL tibial attachment is approximately 8 mm anterior to the posterior ridge (RER). This is a critical measurement because many primary ACL operative procedures place the ACL graft into the posterior one third of the ACL attachment. It is often the case that during the drilling procedure for the posterior tibial tunnel, or in using this tunnel for the femoral tunnel placement that the tunnel is enlarged posteriorly out of the native ACL footprint and extends to the RER. This situation results in a vertical ACL graft. Often, the preoperative MRI will allow measurements of the tunnel location relative to the AP width and the surgeon is already aware of this problem ( Fig. 8-2 ).

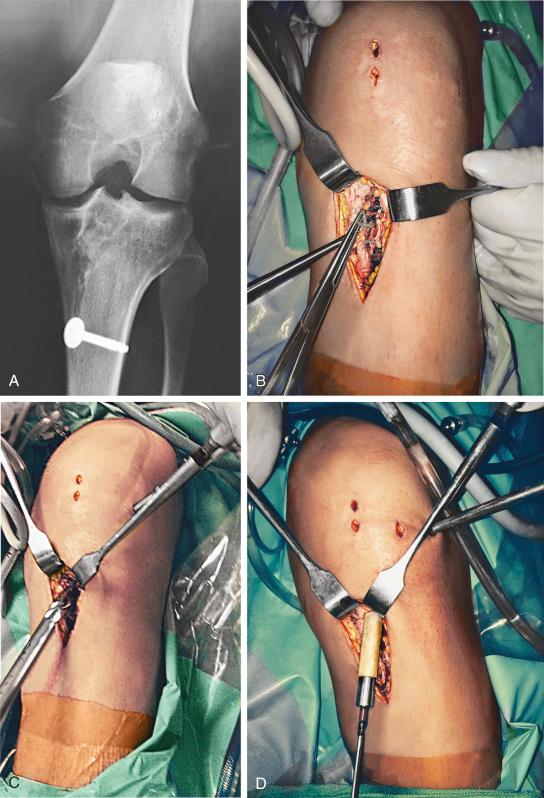
It may initially appear that the tibial tunnel is acceptable; however, after removing all of the soft tissues or when the tibial tunnel drilling is performed, the surgeon may discover that a posterior tibial tunnel exists that extends all the way to or through the RER, which is not acceptable for the revision graft. These cases require staged bone grafting ( Fig. 8-3 ). On occasion, the posterior tibial tunnel is located in the posterior one third of the native ACL attachment, with only a 5-mm bridge between the tunnel and RER. If the tibial tunnel is not dilated requiring grafting, it is possible to drill and relocate the tibial tunnel approximately 8 mm anteriorly into a more advantageous central ACL attachment position. A cortical allograft dowel is positioned to occupy and fill the posterior one third of the tunnel, maintaining the graft in the ideal central position. Another technique is to fashion the bone plug of a revision allograft, maintaining an enlarged bone block to fill the posterior portion of the tibial tunnel and prevent the collagen portion of the graft displacing posteriorly. A third technique is to perform a double-bundle reconstruction with the posterior tibial tunnel used for the PL bundle (assuming the graft is placed into the native ACL tibial footprint and not located in an abnormal posterior position). A second anterior tibial tunnel is used for the anteromedial (AM) bundle. Use of double-bundle grafts in a revision procedure requires that the femoral tunnel location also be ideal, which is often a problem. A misplaced femoral tunnel may prevent two additional tunnels to be adequately placed because these tunnels could possibly weaken the femoral condyle.
In our opinion, the mistake that is possible at ACL revision is to accept a posterior tibial tunnel position for a single-graft procedure. It is preferable to proceed with the staged bone grafting if there is any question that the bone quality is not ideal and that the revision graft would be placed into the posterior one third of the native tibial attachment and result in a windshield effect on weakened bone posteriorly eroding through to the RER. The alternatives listed previously to relocate the graft tunnel are indicated only when good bone quality exists and the prior tibial tunnel does not extend beyond the native ACL attachment. In our experience, in the majority of revision cases involving a posteriorly placed tibial tunnel, the tunnel is frequently dilated and expanded. This is not suitable for bone incorporation into the revision graft, and there is little question that staged bone grafting is necessary.
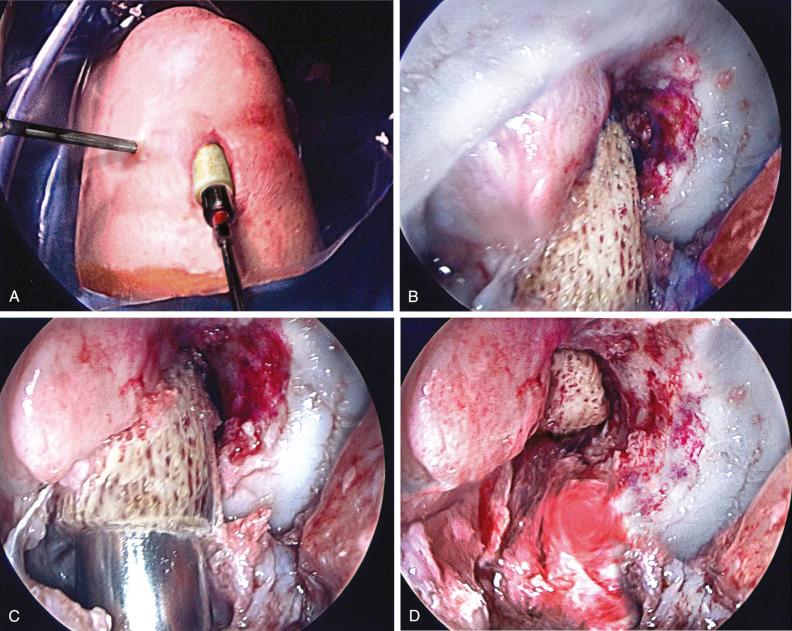
The arthroscope is placed in the AM portal to view the entire lateral notch and notch roof, and all soft tissues and graft material are removed. An angled curette, suction cutting device, and occasionally a radiofrequency probe are used. Any spurs or overgrowth of the notch are removed and a limited notchplasty performed to view the furthest posterior aspect of the lateral notch. A mistake is to not remove all of the lateral soft tissues adjacent to the lateral femoral condyle articular cartilage edge because this is the landmark for identification of the correct location of the revision graft. With a prior vertical tunnel or anterior tunnel, it is often possible to outline the native ACL attachment, which provides important identification landmarks for graft location. The ACL footprint is mapped out and the determination is made whether an ideal anatomic central tunnel is possible, as described.
In a majority of revision cases, the index graft is placed in a vertical, nonanatomic position on the roof of the intercondylar notch ( Fig. 8-4 ) and it is possible to place the revision tunnel in the ideal central ACL anatomic attachment. We use the two-incision approach to reorient the femoral tunnel entirely away from the index tunnel. It is sometimes possible to perform an endoscopic approach using an AM portal to drill the femoral tunnel with a hyperflexed knee; however, the two-incision technique is preferable in most revision procedures. In posterior wall femoral blowout situations, a reoriented tunnel wall can often be used and the bone portion of the graft fashioned so that the bone is placed in the posterior portion of the tunnel to maintain the collagen portion of the graft within the native ACL femoral footprint.

The more difficult problem is the management of a dilated and slightly misplaced femoral tunnel that is at the native ACL attachment or perhaps extends a few millimeters beyond the native ACL attachment onto the intercondylar roof. The new tunnel will overlap and produce an enlarged dilated tunnel with portions extending proximal and beyond the native ACL footprint. There is a technique in which two stacked interference screws (absorbable or metallic) are used to provide a buttress against one side of a dilated tunnel to locate the graft within the ideal femoral attachment. However, this technique is possible only when the femoral tunnel is close to ideal and the stacked interference screw is truly used as a buttress screw against one side of the tunnel wall. The remainder of the femoral tunnel cannot be dilated or enlarged, and the bone quality about the femoral tunnel is not osteopenic and allows for graft fixation. The femoral tunnel for the graft does not extend to the roof of the notch or to the edge of the femoral articular cartilage.
The mistake that may be made is to accept a “slightly enlarged” femoral tunnel in which the graft placement is not ideal, such as too proximal or anterior on the lateral femoral wall. If there is any question, a bone grafting procedure is performed and the revision reconstruction done 5 to 6 months later. Meniscus repairs may be done with the bone grafting procedure to protect the meniscus, and a functional brace used until the revision procedure is performed.
Prepare graft site by removing all soft tissues, curette, and place small drill holes into the cortical tunnel walls.
Culture removed soft tissues, possible Gram stain, cell count.
Freeze-dried dense cancellous allograft core used in tunnel or to replace posterior tibial RER when deficient.
Rare cases, minimally invasive iliac crest autograft procedure, remove only the superior and outer portions, do not disturb the inner table and muscle attachments.
Major defects: cancellous allograft bone in 5- to 8-mm fragments packed between cortical-cancellous strips.
There are available principles to follow when performing bone grafting of enlarged tunnels ( Table 8-2 ). The first is to adequately prepare the graft site by removing all soft tissues, curette, and place small drill holes into the cortical tunnel walls to provide the most ideal surface for bone graft healing. Cultures of the removed soft tissues are obtained. Rarely, a Gram stain and frozen section are necessary to exclude an occult infectious process within a tibial or femoral tunnel, particularly when an allograft was used.
|
Second, a freeze-dried dense cancellous allograft core that may be fashioned to fit snuggly into the remaining tunnel provides an ideal graft for bony incorporation ( Figs. 8-5 and 8-6 ). Third, the posterior tibial RER, when deficient, may also be replaced with a core allograft. The goal is to prevent the revision graft in the newly placed tunnel from enlarging the tunnel posteriorly by a windshield-wiper effect against poor-quality bone. The same situation applies to an enlarged dilated femoral tunnel where the anterior shallow portion of the tunnel is grafted with a core allograft to obtain a good-quality bone construct. It is rare that an autogenous iliac crest autograft is required. However, in such instances, the outer iliac crest can be fashioned into a rectangular or circular dowel that is wedged into the enlarged tibial or femoral tunnel, providing a near-complete filling of the expanded tunnel and likelihood of the revision procedure being performed in 3 to 6 months. Strips of cortical cancellous bone are packed into any remaining defects. In major defects, cancellous allograft bone in the range of 5- to 8-mm fragments are packed between the cortical-cancellous strips. The bone grafting procedure is easily performed in an arthroscopically assisted manner, enlarging the portals as necessary to deliver the bone graft into the femoral tunnel. The tibial tunnel is packed in a retrograde manner, observing the final position of the graft from an appropriate arthroscopic portal. Bone graft substitutes are commercially available; however, their role instead of autogenous or allograft bone has not been established in clinical studies.
Define center ACL, usually 16 to 20 mm anterior to tibial RER or interspinous ridge.
Mark ACL center, usually adjacent and always anterior to posterior edge of lateral meniscus anterior horn attachment.
Place guide pin eccentric and 2 to 3 mm anterior and medial to true ACL center.
Determine graft length of patellar tendon on MRI.
Two-incision technique allows graft length to be adjusted by proximal advancement of femoral tunnel.
Place tibial tunnel in coronal manner, 55- to 60-degree angle, tunnel length 35 to 40 mm.
Begin tunnel adjacent to superficial MCL, 15 mm medial to tibial tubercle medial border, 10-mm distal proximal patellar tendon insertion.
Use core reamer to obtain good-quality bone to fill bone defects.
Drill tunnel, chamfer edges.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here