Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The concept of endovascular therapy of atherosclerotic occlusive disease was introduced in the 1960s when Dotter performed the first transluminal angioplasty in a patient with ischemic extremities. His novel technique, however, could not reliably maintain luminal patency and did not receive wide acceptance as a treatment of vascular occlusive lesions. Subsequent device modifications led to the development of an angioplasty balloon composed of latex material. The clinical success of this new construct was limited, in part because of its improved compliance, and could not fully dilate a calcified lesion. The introduction of an angioplasty balloon made of polyvinyl chloride in 1976 by Gruntzig and Hopff, followed by rigid balloons composed of polyethylene and polyethylene terephthalate, marked a significant advance in endovascular therapy. The latter angioplasty balloons displayed a low compliance and high radial force in a fully inflated condition. As the technology and techniques of endovascular therapy continued to improve and become more widely accepted as outcomes data became available, transluminal balloon angioplasty evolved to an important modality in the treatment of peripheral vascular disease.
Despite numerous studies demonstrating the short-term clinical success of transluminal angioplasty, it has several limitations, in part because of the architectural variation of atherosclerotic lesions. Early restenosis or occlusion following angioplasty can occur because of elastic recoil of the arterial wall or intimal dissection. Vessels that are heavily calcified, completely occluded, or that contain ulcerated plaques might not be amenable to balloon angioplasty. Moreover, residual luminal irregularities following angioplasty occasionally trigger mural thrombus formation, leading to thrombotic occlusion. Late restenosis following angioplasty can occur as a result of intimal hyperplasia or atherosclerotic progression.
In an effort to improve the results of transluminal angioplasty, researchers proposed the concept of intravascular stents as a means of maintaining vessel patency against the restenotic process and improving the clinical outcome of balloon angioplasty. Since Dotter first reported his successful deployment of intravascular stents in canine femoral and popliteal arteries in 1969, a variety of stent devices composed of various materials have been introduced. Intravascular stenting is recognized as a potentially effective modality in overcoming elastic recoil of the arterial wall, stabilizing intimal dissection at the site of angioplasty, and maintaining the luminal patency of arteries with calcified and eccentric atherosclerotic plaques.
The 2000 Trans-Atlantic Inter-Society Consensus (TASC) guidelines were developed to assist physicians in the management of peripheral arterial disease. The classification of inflow of aortoiliac lesions was updated in 2007 as TASC II to reflect the advances in endovascular technology. General guidelines included in the TASC II document state that lesions classified as TASC A ( Table 24.1 ) should be treated preferentially with endovascular techniques, whereas lesions classified as TASC D should be treated preferentially with open surgery. The recommendations for lesions classified as TASC B or C are not as clear. Good surgical judgment including surgical experience, available technology, and patient overall health needs to be considered when deciding on the appropriate initial treatment plan.
| Type | Definition | Treatment Choice |
|---|---|---|
| A | Unilateral or bilateral stenoses of CIA | Endovascular |
| Unilateral or bilateral single short (<3 cm) stenosis of EIA | ||
| B | Short (≤3 cm) stenosis of infrarenal aorta | Endovascular preferred |
| Unilateral CIA occlusion | ||
| Single or multiple stenoses totaling 3–10 cm involving the EIA not extending into the CFA | ||
| Unilateral EIA occlusion not involving the origins of the internal iliac or CFA | ||
| C | Bilateral CIA occlusions Bilateral EIA stenoses 3–10 cm long, not extending into the CFA for good-risk patients |
Open surgery preferred |
| Unilateral EIA stenosis extending into the CFA | ||
| Unilateral EIA occlusion that involves the origins of the internal iliac and/or CFA | ||
| Heavily calcified unilateral EIA occlusion with or without involvement of origins if internal iliac and/or CFA | ||
| D | Infrarenal aortoiliac occlusion | Open surgery |
| Diffuse disease involving the aorta and both iliac arteries requiring treatment | ||
| Diffuse multiple stenoses involving the unilateral CIA, EIA, and CFA | ||
| Unilateral occlusions of both CIA and EIA | ||
| Bilateral occlusions of EIA | ||
| Iliac stenosis in patients with AAA requiring treatment and not amendable to endograft placement or other lesions requiring open aorta or iliac surgery |
The desired characteristics of an intravascular stent depend on the anatomic placement and lesion characteristic for which it will be used. In general, the optimal stent needs to be encased in a low-profile device to cross high-grade lesions, and the stent should be deployed easily and accurately. Flexibility and durability are important characteristics that need to be combined with a low thrombogenic nature and high radial force. Moreover, the stent should have noticeable radiographic opacity to facilitate visualization. Finally, the ideal stent would be biocompatible, to promote endothelialization without causing intimal hyperplasia.
Intravascular stents can be separated into three distinct types: self-expanding stents, balloon-expandable stents, and covered stents ( Table 24.2 ). Within each of these categories, there are numerous stents with different structural materials, deployment devices, and biocompatible characteristics. In addition, there are many stents undergoing clinical trials. Table 24.3 lists the commercially available stents that can be used to treat aortoiliac occlusive disease with the US Food and Drug Administration (FDA) indication status. Some stents are tested and marketed in noniliac positions but have found use in the clinical world for arterial occlusive disease. Additionally, medicated stents and drug-coated balloons have been approved for arterial occlusive disease but are currently FDA approved only for iliac lesions. The Bard Lutonix balloon catheter (Bard Peripheral Vascular, Tempe, Arizona) and the Impact Admiral balloon catheter (Medtronic Vascular, Santa Rosa, California) have also been approved to treat superficial femoral artery (SFA) lesions, but they have also been reported for use in the iliac arteries.
| Self-Expanding | Balloon-Expandable | Covered Stent |
|---|---|---|
| Flexible | Rigid | Flexible |
| Low radial force | High radial force | Low radial force |
| Longer lengths | More effective at short lengths | Longest lengths available |
| Covering sheath in delivery system | Premounted on a balloon | Sheath or balloon premounted |
| Shortening is variable | Some shortening | Minimal shortening |
| Nitinol frame | Steel frame | Nitinol or steel frame |
| Radiopacity is low | Radiopacity is moderate | Radiopacity is moderate |
| Less accurate placement | Accurate placement | Variable accuracy |
| Device Name | Manufacturer | Stent Type | FDA Approved for: |
|---|---|---|---|
| Omnilink | Abbott | Balloon Expandable | Iliac |
| Herculink | Abbott | Balloon Expandable | Renal |
| Express LD | Boston Scientific | Balloon Expandable | Iliac |
| Express SD | Boston Scientific | Balloon Expandable | Renal, biliary |
| Formula | Cook Medical | Balloon Expandable | Renal, biliary |
| Palmaz | Cordis/Cardinal | Balloon Expandable | Iliac |
| iCast | Atrium/Maquet | Covered, Balloon Expandable | Tracheobronchial |
| Assurant Cobalt | Medtronic | Balloon Expandable | Iliac |
| Visipro | Medtronic | Balloon Expandable | Iliac |
| Absolute Pro | Abbott | Self-Expanding | Iliac |
| Supera | Abbott | Self-Expanding | SFA/popliteal |
| Luminexx | Bard | Self-Expanding | Iliac |
| LifeStent | Bard | Self-Expanding | Iliac/SFA |
| Epic | Boston Scientific | Self-Expanding | Iliac |
| Innova | Boston Scientific | Self-Expanding | SFA |
| Wallstent | Boston Scientific | Self-Expanding | Iliac |
| Zilver | Cook Medical | Self-Expanding | Iliac |
| Smart | Cordis/Cardinal | Self-Expanding | Iliac |
| Complete SE | Medtronic | Self-Expanding | Iliac, SFA. popliteal |
| Everflex | Medtronic | Self-Expanding | Iliac, SFA, popliteal |
| Protégé | Medtronic | Self-Expanding | Iliac |
| Misago RX | Terumo | Self-Expanding | SFA, popliteal |
| Fluency | Bard | Covered, Self-Expanding | AV grafts |
| Viabahn | W.L. Gore | Covered, Self-Expanding | SFA, popliteal |
| Zilver PTX | Cook Medical | Drug Eluting, Self-Expanding | SFA |
Self-expanding stents are generally manufactured so that the stents are constrained within a delivery sheath. The prosthesis is placed intravascularly through an introducer sheath that is advanced over a guidewire for deployment. Deployment is achieved by withdrawing the constraining sheath while keeping the stent in position, thus permitting the stent to self-expand and anchor to the vessel lumen ( Fig. 24.1 ). Stents in this category are generally noted for their ease of deployment and high degree of flexibility for meandering around the curves typically found in an iliac artery. These characteristics are advantageous because self-expanding stents can be used across arteries of varying diameters, specifically from the common to the external iliac. Compared with balloon-expandable stents, however, they may have lower radial force, or resistance to radial compression. These stents require oversizing by 2 to 3 mm to maintain outward radial force after deployment. Most self-expanding stent delivery systems have a smaller diameter compared with those of balloon-expandable stents. In addition, the Wallstent and the Gianturco-Z stent (Cook, Bloomington, Indiana) are available.
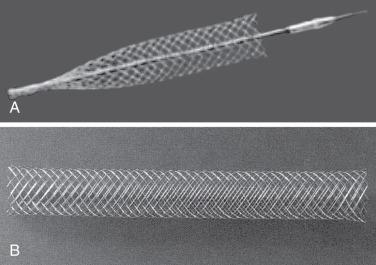
Another type of self-expanding stent is the nitinol stent, which was first introduced by Dotter and colleagues in 1983. Nitinol is a nickel-titanium alloy that has a unique temperature-associated memory property. The nitinol wires can be shaped into a coil spring configuration to serve as a stent when heated to 500°C. As it cools down to 0°C, the nitinol coil straightens into a linear alignment that can be constrained into a delivery catheter for stent deployment. The exposure to warm body temperature after deployment causes the nitinol stent to resume its original coil spring shape. Several clinical studies have evaluated the application of these stents in vascular occlusive lesions.
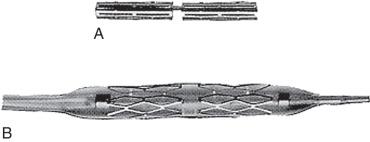
The balloon-expandable stent is first mounted and compressed onto an angioplasty balloon. The original stents were all operator mounted; newer stents are premounted by the manufacturer. Once the stent is positioned intraluminally, it is deployed by inflating the balloon to expand the stent ( Fig. 24.2 ). Unlike a self-expanding stent, the balloon-expandable stent can be expanded beyond its nominal diameter by using a larger angioplasty balloon catheter. Most balloon-expandable stents are characterized by excellent radial strength because of intrinsic stent rigidity once deployed, which can be advantageous in treating stenotic vessels containing calcified plaques. The rigid property of such a stent, however, can create a technical dilemma when treating lesions in tortuous vessels. Moreover, it makes a contralateral approach for iliac artery stenting a challenge, although newer stents are more trackable and flexible.
The first covered stent approved by the FDA for use in the iliac system was the Gore Viabahn stent (Gore, Flagstaff, Arizona). It is a flexible Nitinol stent lined with expanded polytetrafluoroethylene. The flexibility of nitinol, as in self-expanding stents, allows it to closely conform to the vessel shape. In addition, it has a heparin-bioactive surface that is thromboresistant. It is important to conduct predeployment percutaneous transluminal angioplasty (PTA) of the affected area with subsequent coverage of the entire PTA-treated area with the covered stent. This stent is deployed by untwisting the screw-connector at the base of the deployment knob and slowly pulling the knob away from the adapter. In the Gore Viabahn Endoprosthesis Feasibility Study, 45 limbs in 42 subjects were treated for iliac artery occlusive disease. There was a 12-month primary patency of 86% and a procedural success rate of 93%. This was the first-generation endoprosthesis without the heparin bioactive surface. The Gore VBX stent-graft is a balloon-expandable covered stent with more flexible design. The stent has been recently approved for iliac artery indication.
The main argument for the use of a covered stent rather than an uncovered stent is that the layer material will provide a direct barrier to tissue ingrowth from neointimal hyperplasia. However, restenosis can develop at edges that are not covered by graft material where intima injury may have occurred. Covered stents are also sometimes used when there is concern about the integrity of the arterial wall, such as cases involving perforation.
Interim results from the Covered versus Balloon Expandable Stent Trial (COBEST) conducted in Australia have provided excellent results for challenging aortoiliac occlusive disease. Patients with a classification of TASC B, C, or D in the iliac level were randomized to the Advanta V12 group versus a bare metal stent group. They were followed with duplex ultrasound at various intervals and freedom from stent occlusion was assessed. The covered stent group had a significantly lower restenosis rate and greater freedom from stent occlusion than the bare metal stent group. The covered stent also showed superiority when treating TASC C and D lesions.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here