Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Local anesthesia has many practical uses and is straightforward to administer because of the superficial nature and consistent anatomic course of the sensory nerves surrounding the hand and wrist. It is increasingly used as the sole anesthetic in the outpatient setting for WALANT (wide awake, local anesthesia, no tourniquet) procedures.
Local anesthetics can be administered to individual digits (digital block) along named sensory nerves, such as the superficial radial and dorsal ulnar branches, or locally in random patterned areas to provide complete anesthesia.
This technique facilitates detailed examinations of important structures within the digits and hand in an emergency room setting, such as ensuring tendon continuity in a patient with an acute digit laceration.
Local anesthesia is also useful when evaluating a patient’s motion in real time in the operating room. For example, it may be used to ensure that a complete A1 pulley release has been performed with no residual triggering.
This technique is also useful for patients with critical cardiopulmonary illness because it can obviate the need for general anesthesia.
WALANT is often not appropriate for children and adults who cannot follow instructions or remain still for prolonged periods of time.
Lidocaine is the most widely used agent, with an onset of action of 3 to 5 minutes and duration of action of 60 to 120 minutes. It is most often found in either 1% or 2% concentrations.
Bupivacaine is also commonly used for longer duration of pain control (400–450 minutes). It has a much longer onset of action of 15 to 20 minutes. It often comes in either 0.25% or 0.5% concentrations.
Lidocaine and bupivacaine can be mixed in various ratios to provide the combined benefits of quick onset with lidocaine and long duration of action with bupivacaine.
The advantages of using epinephrine mixed with a local anesthetic (1:200,000 or even 1:100,000) are twofold; it causes vasoconstriction within the surrounding tissue, limiting blood loss during any open procedure, and it also increases the lidocaine/bupivacaine duration of action by preventing systemic absorption. We recommend using epinephrine for common surgical procedures, such as first dorsal compartment release or carpal tunnel release, to limit bleeding in these highly vascular areas.
A solution of 1% lidocaine in epinephrine is nearly 1000 times more acidic than subcutaneous tissue. It can be buffered with standard 8.4% sodium bicarbonate (NaCO 3 ) in a 1 mL:10 mL (NaCO 3 :Lidocaine) ratio. The reduction in acidity is necessary to reduce the pain associated with injection.
Fig. 1.1 shows the sensory distribution of the dorsal hand.
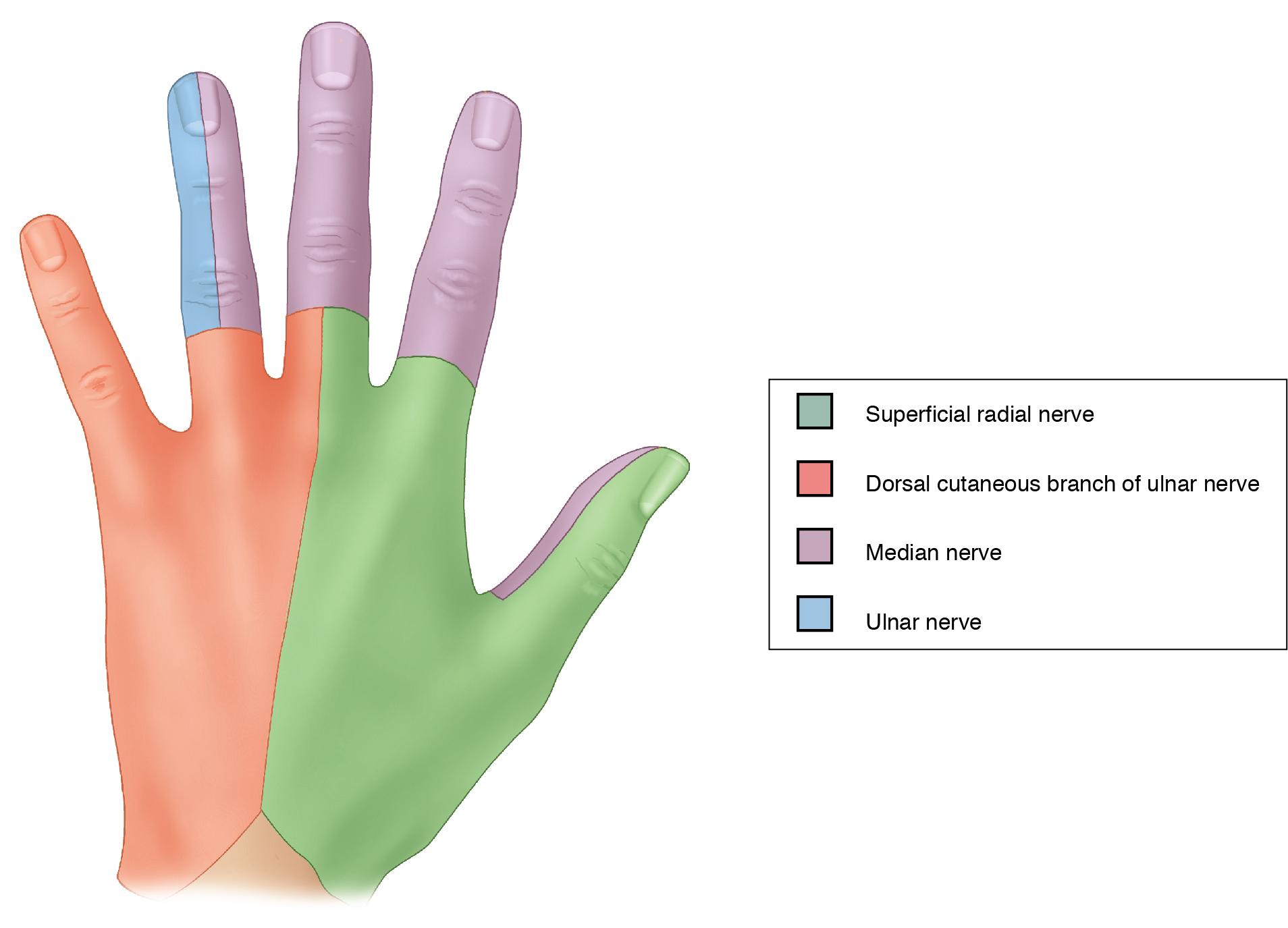
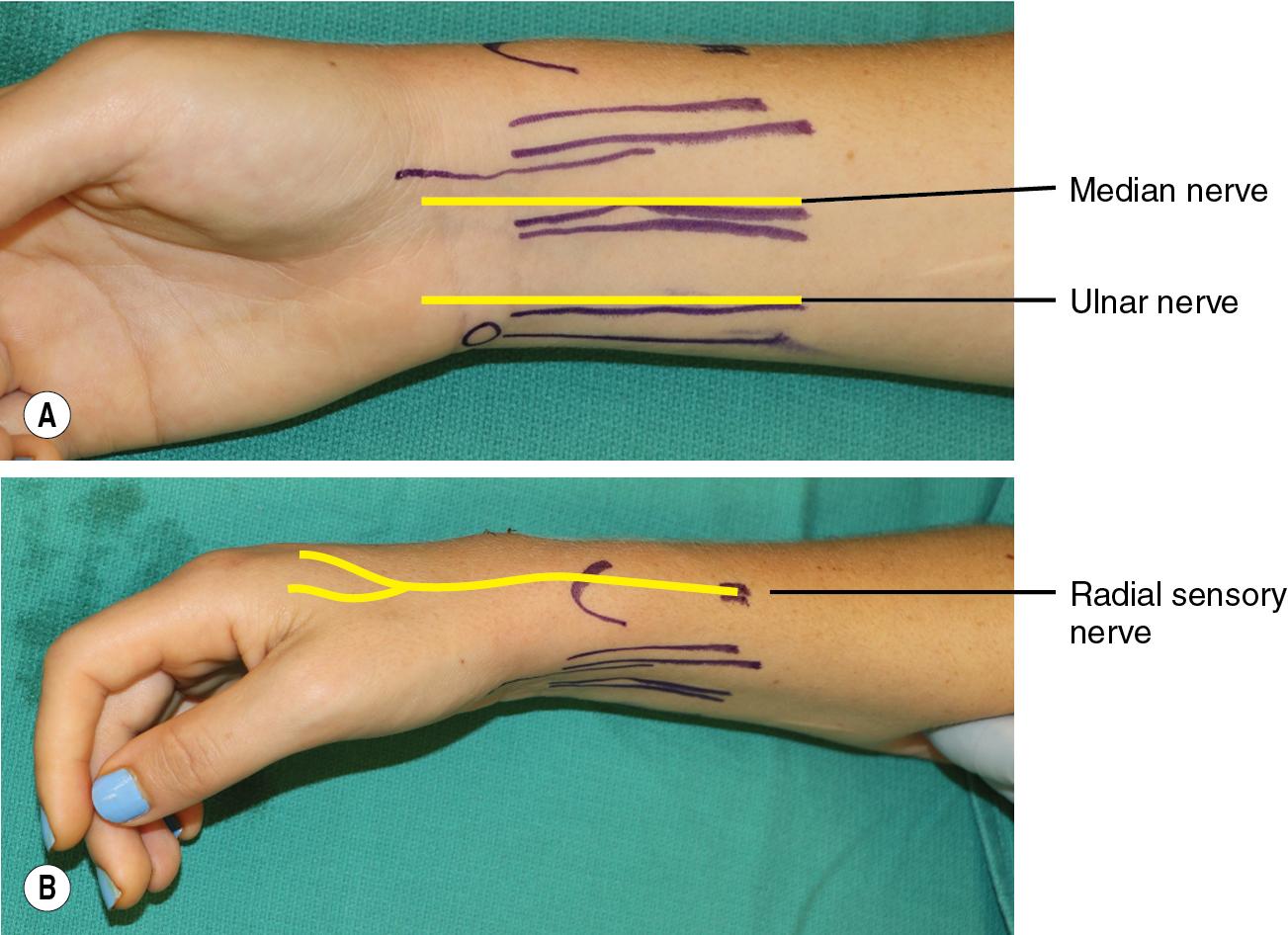
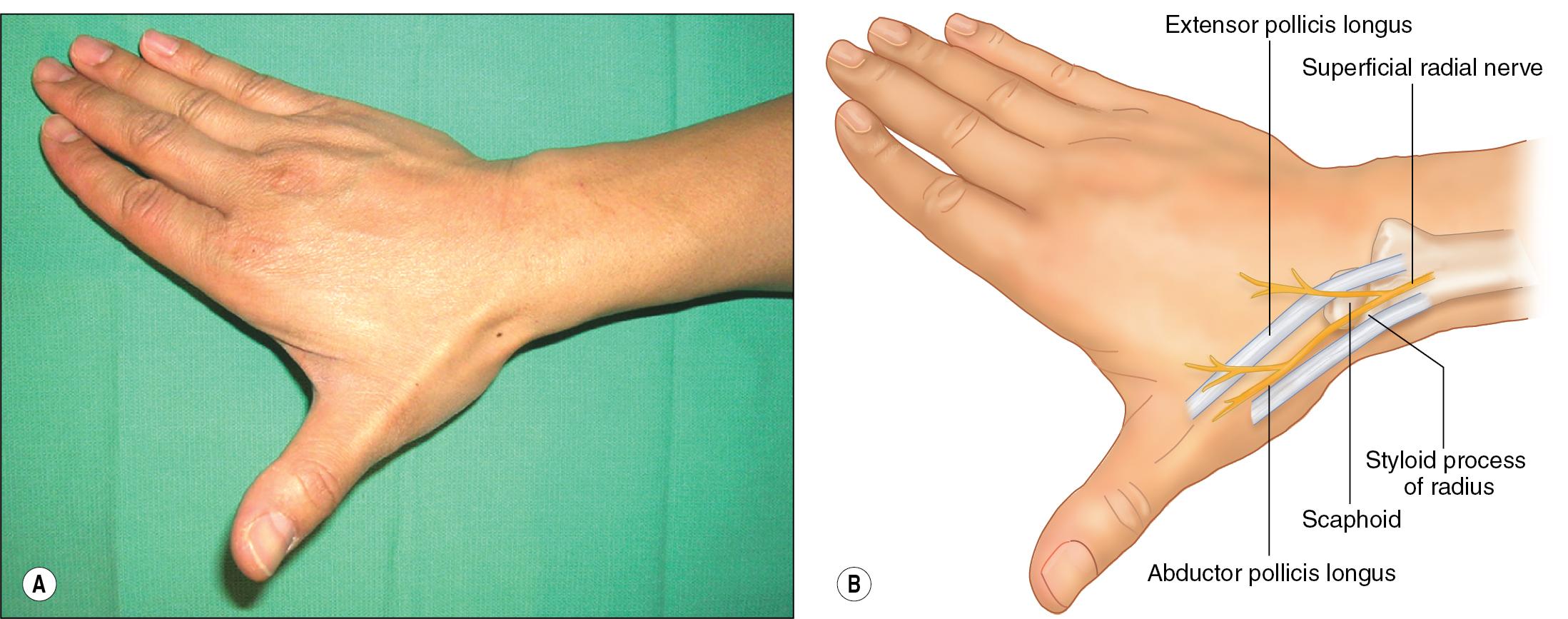
Fig. 1.2 shows the location of the radial, median, and ulnar nerves. The radial nerve crosses the wrist in the area of the radial styloid. The purely sensory nerve arborizes proximal to the radial styloid and crosses the wrist divided into a few major branches that travel in subcutaneous tissues anywhere from just volar to the styloid and as far dorsal/ulnar as the area in line with the middle finger metacarpal ( Fig. 1.3 ).
The median nerve crosses the wrist within the carpal tunnel, and the palmar cutaneous branch crosses in a similar region of the wrist but more superficially. The nerve runs between the palmaris longus (PL) and the flexor carpi radialis (FCR) tendons, and for patients with PL, this tendon can be used to help landmark for injections.
To identify the PL, have the patient pinch their thumb to their ring/small finger and locate the tendon bulge in the wrist ( Fig. 1.4 ).
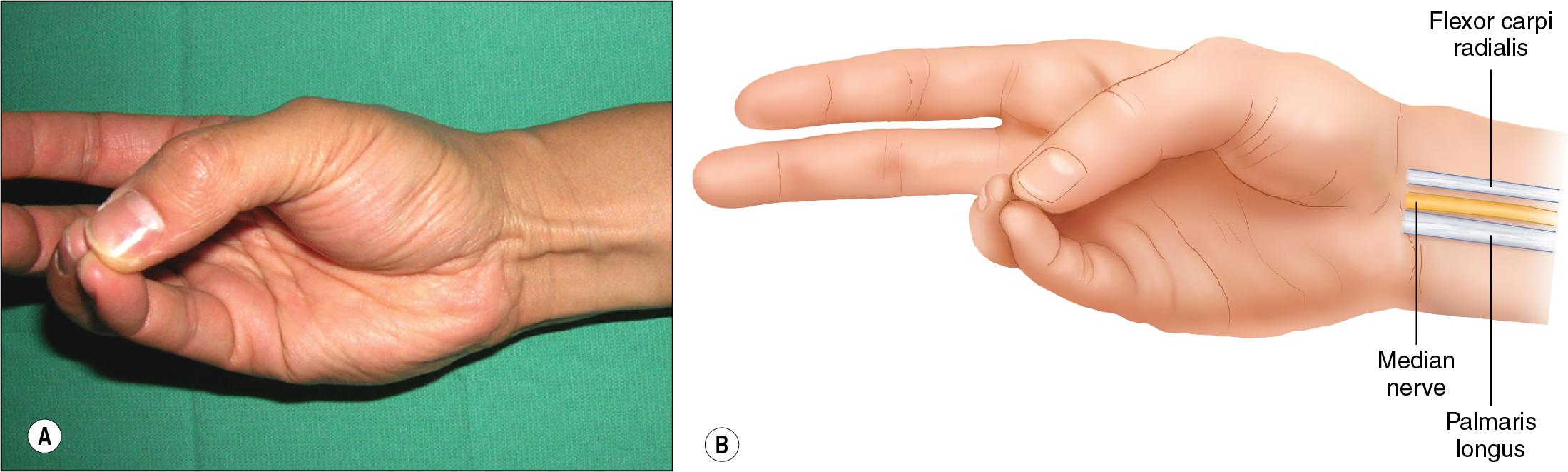
If not present or identifiable, the ulnar border of the FCR tendon can be used as the landmark.
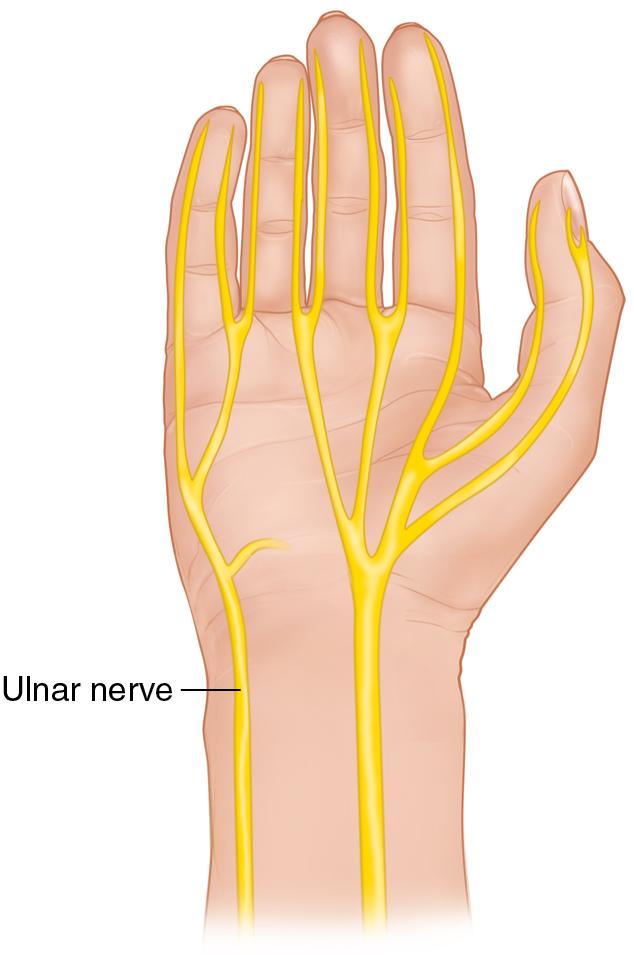
The ulnar nerve crosses the wrist in the area of the flexor carpi ulnaris (FCU) tendon, proximal to its insertion on the pisiform (before entering the Guyon canal).
The ulnar artery is radial to the nerve and to the FCU tendon.
The dorsal sensory branch also runs ulnar to FCU at the level of the wrist, more superficial to the major ulnar nerve trunk ( Fig. 1.5 ).
Common digital nerves travel between the metacarpals. The injection site to perform a block of the common digital nerve to anesthetize multiple fingers at once is at the level of the distal palmar crease, approximately 1 cm proximal to the metacarpophalangeal joint.
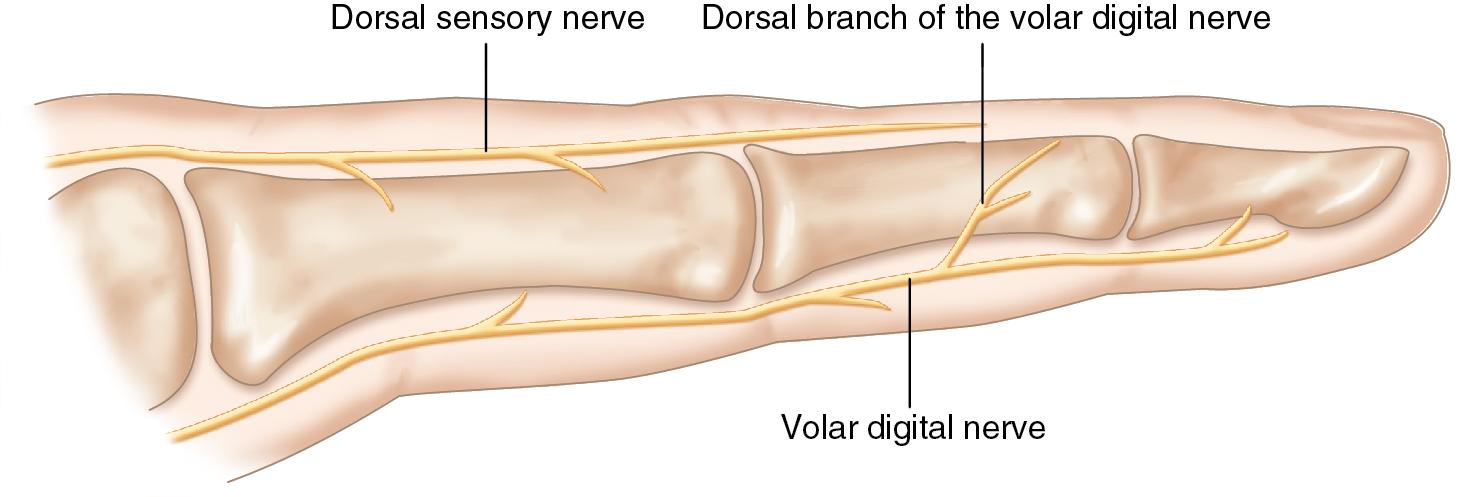
Each finger has a volar and dorsal nerve on the ulnar and radial sides (for a total of four digital nerves). The volar branches are larger, and within the finger are volar to the corresponding digital artery. The volar branches pass from the common digital nerve proximal to each webspace and enter the finger ( Fig. 1.6 ).
Blocks are most easily performed with the patient supine and the arm extended out on a hand table. The great degree of motion through the shoulder, elbow, and wrist allow for these blocks to be performed in a variety of hand and arm positions.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here